

2Department of Neurosurgery, University of Health Sciences, Tepecik Medical Practice and Research Center, Izmir, Turkey DOI : 10.26663/cts.2020.0007
Introduction
Pneumocephalus is a rare condition that defines the pathologic presence of the intracranial air. It is often seen after trauma (skull base or sinus fractures), neoplasms, infections and intracranial operations. Pneumocephalus, which occurs after thoracic operations is rare, but a possible mortal complication. D’Addario reported the first case of pneumocephalus developed after a thoracic operation in the literature in 1974 [1]. Since then, the pneumocephalus after thoracic surgical operations in the literature is rare.Here we present a case of pneumocephalus, as a complication of a non-small cell superior sulcus lung tumor resection.
Case Presentation
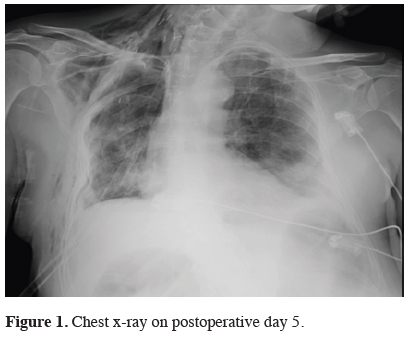
A 70-year-old male patient referred to our hospital with a complaint of cough. The routine examinations and laboratory tests were done and a mass in the right upper lobe of the lung was detected on thorax CT. Transthoracic needle aspiration biopsy was performed, and squamous cell lung cancer was diagnosed. No distant metastasis was detected in PET/CT scan. The patient, whose tumor was considered as a superior sulcus tumor, received two cycles of neoadjuvant chemotherapy (carboplatin and paclitaxol), and a partial response was obtained. The thoracic magnetic resonance imaging (MRI) of the patient revealed no findings of tumor invasion to any vascular or neural structures. The patient underwent a right upper lobectomy and resection of the first three ribs via a Shaw-Paulson incision. There were no complications in the early postoperative period. On the fifth postoperative day, he developed impaired consciousness and his head deviated to the left side as shown at the chest x-ray (Figure 1).
 Click Here to Zoom |
Figure 1: Chest x-ray on postoperative day 5. |
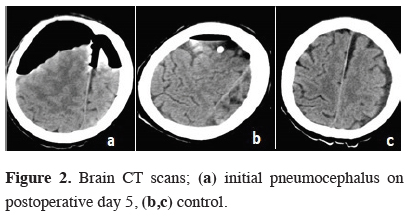
Pneumocephalus and shifting to the left of the midline was detected in the brain computed tomography (CT) scan (Figure 2a).
 Click Here to Zoom |
Figure 2: Brain CT scans; (a) initial pneumocephalus on postoperative day 5, (b,c) control. |
Air decompression was performed via single burr hole drainage by neurosurgeons. Post-procedure Glasgow coma scale of the patient increased from 5 to 12 within 48 hours. The patient was followed up in the Trendelenburg position for a period after the cranial operation. Broad spectrum antibiotics were given to prevent meningitis and encephalitis. There was a regression in pneumocephalus in the control brain CT scan (Figures 2b,c), and the cranial drain of the patient was removed on the postoperative day 8 after an improvement in the neurological condition was observed. Chest drains were removed after the air drainage stopped. However, due to pulmonary infection and respiratory insufficiency, the patient was intubated, and the follow up in the intensive care unit continued with mechanical ventilation support. Despite antibiotic administration and mechanical ventilation, unfortunately the patient died due to severe pulmonary infection and hypoxia on day 12.
Discussion
Pneumocephalus after superior sulcus operations is thought to occur due to extensive dissection around the intercostal nerve root, or due to a dural tear caused by excessive rib retraction resulting from stretching of the intercostal nerve. As for in the postoperative period of the patients whose chest drains were removed, a positive intrapleural pressure resulting from an air leak from the pulmonary parenchyma may form pneumocephalus through this dural tear.In the literature, the number of days between the operation and the onset of pneumocephalus findings varies considerably. Pneumocephalus may present in the early postoperative period, as well as in the relatively later period, such as the 19th day or 30th day [2,3]. This difference also depends on the differences or severity of the pathophysiology of the pneumocephalus mentioned above. The pathogenesis in our patient was thought to be a dural injury that may have occurred during the tumor dissection. Our case was presented on the fifth postoperative day, and the Glasgow coma scale was 5.
When the symptoms of pneumocephalus are examined, the headache is always present. Deterioration in the mental status, loss of consciousness, nausea, vomiting, vertigo, aphasia, dysphasia, hemiplegia are common, but, these are nonspecific findings for the pneumocephalus. The most specific finding for the pneumocephalus is the splashing sound (bruit hydro-aerique) heard by the patient as a result of moving the patient’s head quickly [4]. The initial pneumocephalus symptoms of our patient were impaired consciousness and deviation of the head to the left side. The deviation of the head may occur in several cranial pathologies. But since there is no report in the literature about its relationship with postoperative pneumocephalus cases, we believe the awareness of this symptom could help to diagnose the patient earlier.
In the treatment of the pneumocephalus seen after the thoracic surgery operations, there is not yet a consensus on the literature. Conservative treatments such as bed rest, upside-down position (Trendelenburg position), antibiotic prophylaxis, re-chest tube drainage are discussed to be sufficient for some patients [5]. When a subarachnoid-pleural fistula is diagnosed during the thoracotomy, the fistula should be repaired with a suture ligation or a vascularized muscle pedicle. Also, surgical tissue adhesives can be used to seal the fistulae [5]. If tension pneumocephalus is present, cranial decompression also takes part in the treatments [6]. When the conservative treatments are unsuccessful, there are also publications recommending re-operations to repair the dural tear that occurred [7].
Pneumocephalus is a severe and mortal complication. Especially in patients with superior sulcus tumors, it may be seen even in non-operated patients [8]. For this reason, clinical awareness is essential. It should not be forgotten that pneumocephalus can be seen not only in the superior sulcus tumor surgeries but also after the epidural anesthesia practices [9].
In conclusion, it should be kept in mind that pneumocephalus may develop in the superior sulcus tumor resection for the early recognition of this rare complication. When pneumocephalus is detected, a rapid solution should be produced, and a treatment plan must be made with the neurosurgery department. If a shift is present, cranial decompression should be performed, and the conservative and/or surgical treatment should be planned promptly depending on the etiology with a multidisciplinary approach.
Declaration of conflicting interests
The authors declared no conflicts of interest with respect to the authorship and/or publication of this article.
Funding
The authors received no financial support.
Reference
1) D’Addario R, Greenberg J, O’Neill TJE, Spagna P. Pneumocephalus: an unusual case. J Neurol Neurosurg Psychiatry 1975;37:271-4.
2) Philipp J, Boogaerts JG, Dryjski J. Subarachnoid-pleural fistula complicating thoracotomy. J Clin Anesth 2011;7:590-2.
3) Schuchert MJ, Myers TG, DeGraft-Johnson J, Bejjani GK, Luketich JD, Landreneau RJ. Pneumocephalus after resection of a lung cancer with posterior chest wall involvement. Ann Thorac Surg 2009;87:1609-11.
4) Brown III WM, Symbas PN. Pneumocephalus complicating routine thoracotomy: symptoms, diagnosis, and management. Ann Thorac Surg 1995;59:234-6.
5) Barbetakis N, Samanidis G, Paliouras D, Tsilikas C. Tension pneumocephalus complicating Pancoast tumor resection. Interac Cardiovasc Thorac Surg 2009;8:680-1.
6) Ladehoff M, Zachow D, Koch C, Nowak G, Echelmeyer A, Arnold H, Giese A. Cerebellar haemorrhage and tension pneumocephalus after resection of a Pancoast tumour. Acta Neurochir 2005;147:561-4.
7) Schuchert MJ, Myers TG, DeGraft-Johnson J, Bejjani GK, Luketich JD, Landreneau RJ. Pneumocephalus after resection of a lung cancer with posterior chest wall involvement. Ann Thorac Surg 2009;87:1609-11.



