

2Department of Thoracic Surgery, Tamale Teaching Hospital, Tamale, Ghana
3Department of Thoracic Surgery, Faculty of Medicine, Marmara University, Istanbul, Turkey DOI : 10.26663/cts.2017.0001
Summary
Background: Endoscopic treatment (ET) methods for achalasia such as balloon dilatation and botulinum toxin injection has good success for short and medium term management of achalasia. However some patients either need repeat attempts or referred to surgery. In this study we analyzed and compared the perioperative and disease specific quality of life outcomes of achalasia patients who either underwent surgery as a first line treatment and the ones who underwent ET method prior to surgery.Materials and Methods: The patients who underwent standard of care diagnostic workup and surgery for achalasia by the same surgical team between 2007 and 2014 were recorded in a prospective database. The patients who underwent surgery as a first line treatment (Group 1, n = 55) and the patients who underwent prior ET (Group 2, n = 33) were identified. Demographic data, peroperative complications, length of hospital stay, pre- and postoperative Eckardt scores were recorded and analyzed.
Results: A total of 88 patients out of 105 were available for follow up with average follow up time of 61.9 ± 35.8 months. The mean age was 43.3 ± 15.6. Mean hospital stay was 2.3 ± 0.8 days and there was no mortality. Average duration of the effectivity of ET before myotomy was 5.7 ± 7.7 months. Peroperative complications not significantly accumulated in either group. Both groups showed comparable drop in Eckardt scores.
Conclusions: Heller myotomy and Dor fundoplication is a safe and durable option for treatment of achalasia for both treatment naive patients and patients with previous repeated ET modalities.
Introduction
Achalasia is a motility disorder of the esophagus characterized by loss of neurons in myenteric plexus, impaired coordinated relaxation of lower esophageal sphincter (LES) and aperistalsis of the body of the esophagus, resulting in progressive dysphagia and esophageal dilation due to food stasis. If untreated, it leads to a poor quality of life with pain / difficulty in swallowing, retrosternal pain, regurgitation, weight loss, respiratory issues secondary to aspiration [1,2]. The severity of the symptoms is mostly assessed by using the Eckardt scoring system [1]. Although the exact cause of achalasia is unknown, most of the promising research focuses on viral and autoimmune etiologies. Currently treatment strategies offer symptomatic and functional relief through relaxation of LES barrier, there is also evidence of partial return of the peristaltic function of the esophagus after long term resolution of the outflow obstruction [3]. Endoscopic treatments like balloon dilatation and botulinum toxin injection can provide quick relief with low morbidity and mortality but repeated attempts may be needed to maintain quality of life [4]. Myotomy on the other hand, can be achieved either by minimally invasive surgery or per oral endoscopic myotomy (POEM). Laparoscopic Heller myotomy and partial fundoplication is a well-established surgical procedure for achalasia with long term data on patient selection, complications, hospital stay and overall effectiveness [5]. POEM is a promising new technique delivering good symptom relief, but concerns over lack of long term data, learning curve and post procedure gastroesophageal reflux still remain [6].Since there is a wide range of approaches available for treatment of achalasia and not a single option is firmly established as a gold standard for first choice. There is a significant subset of patients who received previous single / multiple endoscopic treatments and then referred for surgery due to the persistence of symptoms. Balloon dilatation / botulinum toxin injection can induce anatomic disruptions, loss of tissue planes, fibrosis/scar tissue around gastroesophageal junction (GEJ) and interfere with safety of standard surgical myotomy technique. We report our results of laparoscopic Heller myotomy and Dor fundoplication for patients who had previous balloon dilatation in comparison to patients who underwent surgery as a first line treatment.
Methods
112 achalasia cases were operated on in our institution between 2007 and 2015 and were recorded in a prospective database. All patients underwent appropriate informed consent procedure, agreeing for further follow up, recording and usage of anonymized medical data for scientific and medical purposes. All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2008.88 patients were available for long term follow up. Patients were assigned into two groups as Group 1 (n=55); surgery as first line treatment, Group 2 (n=33); surgery after prior endoscopic treatment. All patients had standard workup for esophageal motility disorders (esophageal standard and/or high resolution manometry, esophagogram) and their demographic data, pre/post-operative Eckardt scores, length of hospital stays and perioperative complications were recorded.
Heller Myotomy and Dor Fundoplication was performed by the same surgical team. The operation was conducted laparoscopically with 4 port placements, typically three 5 mm trocars and one 10 mm trocar.
Data was analyzed using SPSS 11.0 software. Mann Whitney U test was used for evaluating pre and post-surgery changes in Eckardt scores, Student"s T test was used for group comparison.
Results
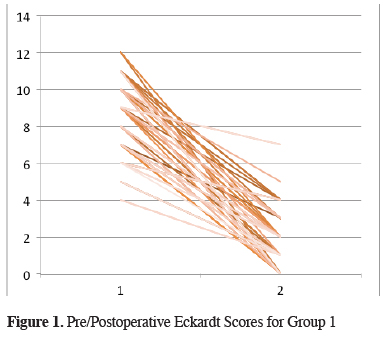
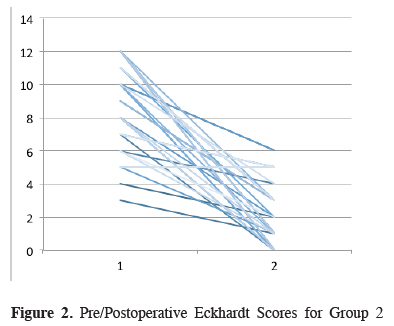
Out of 112 patients who underwent laparoscopic Heller myotomy and Dor fundoplication, 88 were available for long term follow up and consented to participate in the study. Patient characteristics and demographic data are summarized in Table 1. Group 1 and 2 had an even distribution of patient gender and age. Average duration of effectivity per attempt of endoscopic treatment was 5.7 months (1-12 months). Perioperative results and outcomes are summarized in Table 2. Both groups enjoyed comparable relief of symptoms measured by decreased Eckardt scores after surgery (Group 1=86%, Group 2=85%) (Figures 1 and 2). There was no mortality and major morbidity in either group. Average hospital stay and peroperative complications did not differ between the two groups.Table 1: Patient characteristics
Table 2: Perioperative results and outcomes
 Click Here to Zoom |
Figure 1: Pre/Postoperative Eckardt Scores for Group 1 |
 Click Here to Zoom |
Figure 2: Pre/Postoperative Eckhardt Scores for Group 2 |
Discussion
Laparoscopic Heller Myotomy and Dor fundoplication offers a durable, safe and effective solution for patients both as a first and second line treatment strategy. In terms of technical difficulty, anatomic changes and fibrosis related to stasis, dilatation and loss of normal tissue planes can be shown histologically and may be exacerbated by prior endoscopic treatment attempts [7], but this fact did not necessary translate itself into decreased benefit from surgery, increased hospital stay / morbidity. Both patient groups benefited from surgery as expected, demonstrated by drop in their dysphagia scores, correlating with existing literature [8].Even though our data reveals that average duration of symptom control after an endoscopic treatment modality is close to 6 months, there is a wide range of distribution. There are studies for balloon dilatation as a first line technique and show the same pattern as well. From a clinical point, this variation in response to treatment, low morbidity and mortality and possibility of equally safe surgery after endoscopic treatment forms the rationale for a trial of endoscopic treatment as a first line option for many gastroenterologists [4]. The outcome from laparoscopic Heller myotomy is shown to be durable beyond 1 year (86% vs 76%) with very low relapse rates when compared with balloon dilatation [9]. At 2 years, a significant subset of patients (15-30%) will require symptom control for dysphagia after balloon dilatation [9,10] (Table 3).
Table 3: Comparison of various treatment methods for achalasia
For patients failing to respond optimally to endoscopic treatment options, referral for surgery seems to be just as safe and also a definitive solution for outflow obstruction. It results in return of peristaltic function of esophagus and potentially better long term functionality [3].
POEM also shows promising results [6], but there is no long term data available. Large case series show it to be an option comparable to surgery and caution should be exercised for patients with long standing disease and for patients who are not treatment naïve. Technical impossibility of adding an antireflux barrier procedure to POEM and already increased risk of esophageal cancer in achalasia patients may be a point of concern in the future.
In conclusion, endoscopic treatment modalities for achalasia have variable durations of symptomatic control with low risk of morbidity and do not preclude surgery for more definitive solution. Laparoscopic Heller Myotomy and Dor fundoplication results in equally favorable outcomes in both endoscopically treated and treatment naïve patients, also may provide for return of esophageal motility in long term (Table 3). POEM proponents have published encouraging results but the procedural safety itself and long term results for inability to include an anti-reflux barrier needs to be evaluated.
Declaration of conflicting interests
The author declared no conflicts of interest with respect to the authorship and/or publication of this article.
Funding
The author received no financial support for the research and/or authorship of this article.
Reference
1) Alexander J. Eckardt, Volker F. Eckardt Treatment and surveillance strategies in achalasia: an update. Nat Rev Gastroenterol Hepatol 2011; 8: 311-319.
2) Gupta M, Ghoshal UC, Jindal S, Misra A, Nath A, Saraswat VA. Respiratory dysfunction is common in patients with achalasia and improves after pneumatic dilation. Dig Dis Sci 2014; 59: 744-52.
3) Roman S, Kahrilas PJ, Mion F, Nealis TB, Soper NJ, Poncet G, et al. Partial recovery of peristalsis after myotomy for achalasia: more the rule than the exception. JAMA Surg 2013; 148: 157-64.
4) Richter JE, Boeckxstaens GE. Management of achalasia: surgery or pneumatic dilation. Gut 2011; 60: 869-76.
5) Krishnamohan P, Allen MS, Shen KR, Wigle DA, Nichols FC 3rd, Cassivi SD, et al. Long-term outcome after laparoscopic myotomy for achalasia. J Thorac Cardiovasc Surg 2014; 147: 730-6.
6) Sharata AM, Dunst CM, Pescarus R, Shlomovitz E, Wille AJ, Reavis KM, et al. Peroral endoscopic myotomy (POEM) for esophageal primary motility disorders: analysis of 100 consecutive patients. J Gastrointest Surg 2015; 19: 161-70; discussion 170.
7) Bloomston M, Fraiji E, Boyce HW Jr, Gonzalvo A, Johnson M, Rosemurgy AS. Preoperative intervention does not affect esophageal muscle histology or patient outcomes in patients undergoing laparoscopic Heller myotomy. J Gastrointest Surg 2003; 7: 181-8; discussion 188-90.
8) Schoenberg MB, Marx S, Kersten JF, Rösch T, Belle S, Kähler G, et al. Laparoscopic Heller myotomy versus endoscopic balloon dilatation for the treatment of achalasia: a network meta-analysis. Ann Surg 2013; 258: 943-52.
9) Yaghoobi M, Mayrand S, Martel M, Roshan-Afshar I, Bijarchi R, Barkun A. Laparoscopic Heller"s myotomy versus pneumatic dilation in the treatment of idiopathic achalasia: a meta-analysis of randomized, controlled trials. Gastrointest Endosc 2013; 78: 468-75.
10) Boeckxstaens GE, Annese V, des Varannes SB, Chaussade S, Costantini M, Cuttitta A, et al. Pneumatic dilation versus laparoscopic Heller"s myotomy for idiopathic achalasia. N Engl J Med 2011; 364: 1807-16.



