

2Marmara University, Faculty of Medicine, Department of Cardiovascular Surgery, İstanbul
3Marmara University, Faculty of Medicine, Department of Thoracic Surgery, İstanbul, Turkey DOI : 10.26663/cts.2017.0005
Summary
Esophageal leiomyoma one of the most common esophageal tumors and frequently cause dysphagia, requiring surgical removal for symptom control. Aberrant right subclavian artery may also cause similar symptoms but its incidence is lower. We report a case who had dual pathologies as possible causes of dysphagia. A straightforward bi-portal video-assisted thoracoscopic removal of an esophageal leiomyoma was performed in a patient with an aberant right subclavian artery coursing posterosuperior to the leiomyoma.Introduction
Esophageal leiomyoma is the most common benign esophageal tumor, representing 70% of all benign esophageal tumors. Most esophageal leiomyomas are usually slow growing and only discovered incidentally or when they cause symptoms due to their size. Most common symptoms are dysphagia, heartburn and regurgitation. For incidentally discovered leiomyomas, conservative treatment may be considered while if the size larger than 5 cm, progression or suspicion of malignancy warrant surgical treatment [1]. Video-assisted thoracoscopic (VATS) enucleation approach has been reported with very encouraging results, reducing the pain and discomfort due to thoracotomy. Our approach was done with the patient in lateral decubitus position, but excellent results with prone positioning were also published [2,3].Aberrant right subclavian artery (ARSA) is one of the rare reasons for dysphagia. In 80% of the cases it runs posterior to the esophagus to connect to aorta distal to the left subclavian artery and may cause catastrophic complications if unrecognized before surgical interventions in close proximity [4]. The recurrent laryngeal nerve also has an abnormal course in cases of aberrant right subclavian artery, branching from vagus, entering directly to larynx.
In this article, we report the coincidence of an esophageal leiomyoma and an ARSA in a patient who presented to our clinic with dysphagia.
Case Presentation
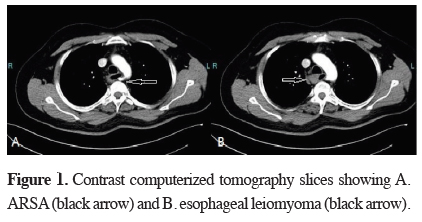
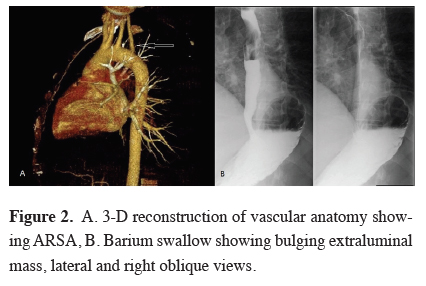
The patient was a 39 year old gentleman who was referred to our clinic for work up of dysphagia for two months. Endoscopy revealed an extraluminal mass partially obstructing the passage, endoscopic ultrasound was highly characteristic of an esophageal leiomyoma but a tissue diagnosis couldn"t be reached through biopsies. A computerized tomography of the chest with intravenous contrast showed an aberrant right subclavian artery running posterior to esophagus in close proximity to the lobular esophageal mass (Figure 1). In terms of deciding the dominant reason for dysphagia, a barium swallow was performed, which showed bulging extraluminal mass causing an incomplete obstruction of the passage (Figure 2).
 Click Here to Zoom |
Figure 1: Contrast computerized tomography slices showing A. ARSA (black arrow) and B. esophageal leiomyoma (black arrow). |
 Click Here to Zoom |
Figure 2: A. 3-D reconstruction of vascular anatomy showing ARSA, B. Barium swallow showing bulging extraluminal mass, lateral and right oblique views. |
The patient underwent a bi-portal (4th and 6th intercostal space, anterior axillary line) VATS enucleation of the leiomyoma in left lateral decubitus position. Dividing the azygous vein and a 3 cm myotomy was required to gain necessary exposure for safe removal of the tumor. The myotomy site was on the right lateral wall of the esophagus for careful avoidance of the ARSA. The myotomy was closed with three 2-0 absorbable sutures. The patient had an uneventful intra- and postoperative course and was discharged on 3rd postoperative day. He was maintained on a soft diet for 2 weeks and can consume a normal diet on 1st month of follow up, without any symptoms.
Discussion
Clinical evaluation of dysphagia requires careful consideration and can involve multiple diagnostic studies to delineate a causative factor. In this case, we present a first in the literature, a patient with two probable factors for dysphagia, a large leiomyoma and a right aberrant subclavian artery. In terms of selecting an approach, a barium swallow study showing a real time passage of bolus and leiomyoma"s impact helped us to determine the leiomyoma as the main causative factor. During the surgery, preoperative awareness of the ARSA was important for preventing an intraoperative unexpected complication [4].In cases of mucosal rupture during stripping of the tumor, simple suturation is usually enough for leak control. In our case, we did not encounter any mucosal rupture, but placed sutures anyway, with the rationale of restoring the anatomy and the blood supply.
Endoscopic ultrasound is fairly specific for diagnosis of esophageal leiomyoma and is also confirmed by pathology results in larger case series. Biopsy is also proven to be safe in cases of submucosal tumors, but has little value for changing the clinical decision making if the resection is to be done for symptomatic purposes (dysphagia) [6,7].
VATS enucleation of esophageal leiomyoma has been reported in large case series and results have been more favorable than thoracotomy [5]. In our case, VATS approach did not cause any problems regarding the dissection and visual exposure even in this case with complicated anatomy. In regards to VATS approach, we preferred a lateral decubitus positioning as exposure of anatomy is more familiar in this position. Prone positioning is also used successfully by other authors [4].
Declaration of conflicting interests
The author declared no conflicts of interest with respect to the authorship and/or publication of this article.
Funding
The author received no financial support for the research and/or authorship of this article.
Reference
1) Lee LS, Singhal S, Brinster CJ, Marshall B, Kochman ML, Kaiser LR, et al. Current management of esophageal leiomyoma. J Am Coll Surg 2004; 198: 136-46.
2) Samphire J, Nafteux P, Luketich J. Minimally invasive techniques for resection of benign esophageal tumors. Semin Thorac Cardiovasc Surg 2003; 15: 35-43.
3) Claus CM, Cury Filho AM, Boscardim PC, Andriguetto PC, Loureiro MP, Bonin EA. Thoracoscopic enucleation of esophageal leiomyoma in prone position and single lumen endotracheal intubation. Surg Endosc 2013; 27: 3364-9.
4) Pantvaidya GH, Mistry RC, Ghanekar VR, Upasani VV, Pramesh CS. Injury of an aberrant subclavian artery: a rare complication of video assisted thoracoscopic esophagectomy. Thorac Cardiovasc Surg 2005; 11: 35-7.
5) Shin S, Choi YS, Shim YM, Kim HK, Kim K, Kim J. Enucleation of esophageal submucosal tumors: a single institution"s experience. Ann Thorac Surg 2014; 97: 454-9.



