

Summary
Metastasis of tracheobronchial tree is an infrequent and life-threatening condition. Endobronchial metastasis is rare while endotracheal metastasis is extremely rare entity. Renal cell carcinoma (RCC) constitutes approximately 3% of all adult malignancies and metastasizes 30% cases to organs during the course of the disease. Lung is the most common target organ of RCC metastasis and usually bilateral parenchymal metastases are seen as well as tracheobronchial system. Hemoptysis may be the first manifestation and bronchoscopy is useful for both diagnosis and therapy. Argon plasma coagulation (APC) is a choice of current therapeutic techniques to achieve hemostasis from bleeding endobronchial lesions. Here we report a case of 72-year-old man was suffering hemoptysis due to endotracheal metastasis of RCC diagnosed via rigid bronchoscopy and palliated with APC successfully.Introduction
Metastasis of tracheobronchial tree, which originates from either primary bronchogenic carcinoma or a non-pulmonary tumor, is a rare but life-threatening condition. Endobronchial metastasis is rare while endotracheal metastasis is extremely rare entity [1]. Renal cell carcinoma (RCC) constitutes approximately 3% of all adult malignancies and metastasizes to regions such as lungs, liver, bone, brain, adrenals and lymph nodes by hematogenous route in approximately 30% of cases during the course of the disease. Lung is the most common organ of RCC metastasis and usually bilateral parenchymal metastases are seen as well as endobronchial metastases [2]. Hemoptysis may be the first manifestation. Bronchoscopy is useful for both diagnosis and therapy. Argon plasma coagulation (APC) is a choice of current therapeutic techniques to achieve hemostasis from bleeding endobronchial lesions.Here we report a case of a patient with complaints of hemoptysis, with an endotracheal metastasis from RCC, diagnosed by rigid bronchoscopy and palliated with APC.
Case Presentation
A 72-year-old man was referred to our clinic due hemoptysis with a history of one month. He had a nephrectomy for renal cell carcinoma, 5 years’ ago. He used to smoke for 45 years and stopped for 5 years. Thorax CT showed metastatic masses in both lungs and a round mass in mid-trachea obstructing 3/4 of the lumen (Video 1).The lobulated and fragile endotracheal mass was resected via rigid bronchoscopy for biopsy and lumen opening under general anesthesia (Video 2). A catheter was inserted through a fiberoptic bronchoscope and APC is applied for palliation of hemoptysis. During processing, FiO2 was reduced to 21% for short periods of time (Video 3). The patient was discharged the next day with more comfortable breathing and ceased hemoptysis.
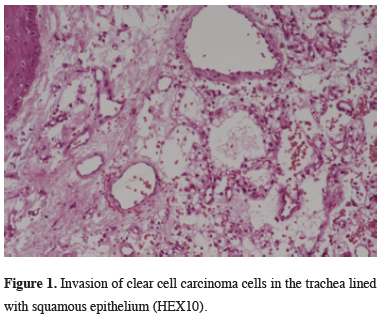
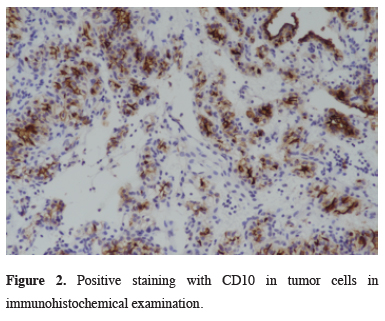
Microscopically, the tumor cells were large, the appearance of the cytoplasm clear with sharply outlined boundaries infiltrating the squamous epithelium of trachea. Immunohistochemical examination of the tumor cells showed moderate vimentin, CD10 and PAX 8 staining, and absent for TTF-1 and CK antigen staining. The morphologic and immunohistochemical features were consistent with metastatic clear type renal cell carcinoma (Figures 1,2). He was referred to the oncology clinic for appropriate systemic treatment.
 Click Here to Zoom |
Figure 1: Invasion of clear cell carcinoma cells in the trachea lined with squamous epithelium (HEX10). |
 Click Here to Zoom |
Figure 2: Positive staining with CD10 in tumor cells in immunohistochemical examination. |
Written informed consent was obtained from the patient for publication of his data.
Discussion
The lungs are the second most common site for solid tumor metastasis with parenchyma and pleura usually being involved. Metastasis of tracheobronchial tree is rather less common and often overlooked [1,3]. Sorenson et al. reported that the trachea was involved in only 5% of all tumors in the respiratory tree [3]. The origin of endotracheal or endobronchial metastasis may be various solid tumors. In a series of 83 metastatic tracheobronchial tumor patients, thyroid, kidney, esophagus and lymphoma are common primary tumors [3]. Tracheal metastatic lesions were mostly originated by intrathoracic tumors (i.e., thyroid and esophagus). Lung cancer can also be seen as endotracheal synchronous/metachronous metastasis, except for direct invasion [3-5]. In a review which published a 39-year series of 2242 secondary tracheal tumors, 92.6% (n = 1.853) were tracheal invasion of adjacent intrathoracic organs, and only 17.4% (n = 389) of cases were distant organ metastasis with hematogenous spread.The most common primary sites of tumor were thyroid, esophagus and lung in the intrathoracic group whereas colorectal carcinoma, breast and melanoma metastasis were widely seen in the distant metastatic group [1,3-6]. Shavit et al reported a case of RCC metastasis of trachea the first time in 2002 [7]. In the series of 550 interventional bronchoscopic cases published by Tsuboi et al in 2016, 9 cases were RCC tracheobronchial metastases, and tracheal metastases were reported in 4 of them [8].
Renal cell carcinoma is the ninth most common cancer worldwide and accounts for 2% to 3% of all malignant tumors in adults. During the course of the disease, it metastasizes to regions such as lungs, liver, bone, brain, adrenals and lymph nodes by hematogenous route in approximately 30% of cases. Lungs are the most common target organ of RCC metastasis [2]. Although it is generally seen as bilateral parenchymal metastasis, it could be also seen as tracheobronchial metastasis in a less common way [1,3,7].
Presenting symptoms of tracheal metastases are dyspnea, stridor, cough, and hemoptysis [1,3,9]. In our patient hemoptysis was the only symptom despite the stenosis in the trachea.
Contrast-enhanced computed tomography (CT) and/or magnetic resonance imaging are important in diagnosis as they emphasize the vascular nature of the metastatic tumor. However, a small endoluminal lesion may be confused with phlegm accumulation and overlooked. Sometimes it can only be diagnosed as a metabolic activity on PET/CT, even if there is no image on CT [10].
Biopsy from the lesion provides more accurate diagnosis while risk of bleeding and airway obstruction must be kept in mind during bronchoscopy. RCC and its endobronchial metastases are frequently hypervascular and hemorrhagic tumors. Rigid bronchoscopy should be a priority in tracheal lesions because of its large working hole, allowing the use of interventional instruments, opening the tracheal lumen by taking off larger pieces, and the possibility of powerful aspiration. However, flexible bronchoscopy may also be necessary for detailed images, cleaning of the distal airways, and the use of instruments such as cryotherapy and APC. Despite all these precautions in case of abundant bleeding, it is a life-threatening situation; a surgical team and a thoracotomy set should be prepared for further operations. Inflating the cuff of the endobronchial tube over the lesion can provide a valid airway and will be a time-saving maneuver. Classical methods (ice sludge, adrenaline saline, cryotherapy, cautery, etc.) may be useful in milder hemorrhages. APC is a technique that can control bleeding instantly without penetrating into deep tissues. The coagulation is achieved with shots made without touching which also has the ability to kill tumor cells [9,11].
Since renal cell carcinoma has traditionally been defined as a radio resistant tumor, surgical excision or other methods are rather beneficial in cases of endobronchial or endotracheal metastasis. New immunotherapy agents are also applied in the treatment of metastatic renal cell carcinoma with promising perspectives [12].
In conclusion, a variety of solid malignancies may metastasize to the tracheobronchial tree. Tracheal metastasis is rare but life-threatening conditions due to tracheal stenosis and hemoptysis. Rigid and flexible bronchoscopy should be used together while the patient is under general anesthesia, and be prepared for the risk of massive bleeding. APC provides a safe hemostasis in bleeding endobronchial tumors when performed by experienced hands. Therapeutic bronchoscopy in such cases can contribute to the quality of life and may impact survival.
Declaration of conflicting interests
The authors declared no conflicts of interest with respect to the authorship and/or publication of this article.
Funding
The authors received no financial support.
Authors’ contributions
ABK, ANK: conceived and designed the current case report, co-wrote the paper, collected the clinical data. The authors discussed the case under the literature data together and constituted the final manuscript.
Reference
1) Madariaga ML, Gaissert HA. Secondary tracheal tumors: a systematic review. Ann Cardiothorac Surg 2018; 7:183-196.
2) Arora RD, Limaiem F. Renal clear cell cancer. 2021. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2021 Jan. PMID: 33085377.
3) Sorensen J.B. Endobronchial metastases from extrapulmonary solid tumors. Acta Oncol 2004; 43: 73-9.
4) Karakattu S, Yorke J, Hoskere T, Stewart L, ElMinaoui W. A rare case of multiple secondary endotracheal metastasis from early stage small cell cancer. Respir Med Case Rep 2020; 30: 101103.
5) Zhang Z, Mao Y, Chen H, Dong J, Yang L, Zhang L et al. Endotracheal and endobronchial metastases in a patient with stage I lung adenocarcinoma. Ann Thorac Surg 2014; 97: e135-7.
6) Choi IY, Lee KY, Lee JH, Je BK, Shin JS, Um JW et al. Tracheal metastasis from rectal cancer: a case report and review of the literature. Balkan Med J 2013; 30: 120-2.
7) Shavit L, Maly B, Rosenbaum E, Grenader T. Endotracheal metastases in renal cell carcinoma: A life-threatening but treatable complication. Eur J Intern Med 2007; 18: 161-3.
8) Tsuboi R, Oki M, Saka H, Kogure Y, Oka S, Nakahata M et al. Rigid bronchoscopic intervention for endobronchial metastasis of renal cell carcinoma Respir Investig 2016; 54: 250-4.
9) Chousein EGU, Turan D, Özgül MA, Çetinkaya E. Secondary pulmonary malignancies requiring interventional bronchoscopic procedures. Turk Gogus Kalp Dama 2021; 29: 360-9.
10) Park CM, Goo JM, Lee HJ, Kim MA, Lee CH, Kang MJ. Tumors in the tracheobronchial tree: CT and FDG PET features. Radiographics 2009; 29: 55-71.



