

2Department of Anesthesia, Kocaeli Health and Technology University, European Vocational College, Kocaeli, Turkey DOI : 10.26663/cts.2023.009
Summary
An esophageal bronchogenic cyst is a rare form of a bronchogenic cyst, a foregut developmental anomaly in embryological age. Herein, we present a case that underwent surgery for the complicated mediastinal esophageal bronchogenic cyst and a thyroglossal duct cyst, another anterior foregut anomaly at the neck. Bronchogenic cysts should be operated on as early as possible due to the complications and a detailed and radiological examination should be kept in mind for other foregut anomalies that may accompany it. To the best of our knowledge, this is the first case reported as the coexistence of two foregut anomalies.Introduction
A bronchogenic cyst is an anomaly, derived from the anterior foregut. They usually appear in the mediastinum or lung parenchyma and are rarely found in the esophageal wall. Multiple extrapulmonary localizations have also been reported [1-3]. Esophageal or mediastinal bronchogenic cysts usually cause symptoms due to compression to the surrounding tissues. Particularly, the cyst may eventually rupture when infected or due to the accumulation of mucus secretion. In addition, malignant transformation is possible after chronic inflammation [4,5]. The general treatment approach for the bronchogenic cyst is surgical resection.Case Presentation
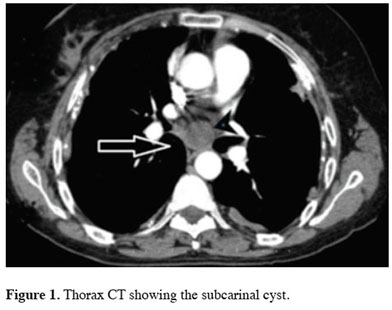
A 58-year-old female patient was referred to our clinic with symptoms of dyspnea and chest pain for over three years. With the progression of her complaint, she was admitted to the emergency service several times with pleuritic chest pain and dyspnea symptoms. The patient’s vital signs showed a heart rate of 85 bpm, a respiration rate of 16 breaths per minute, and an oxygen saturation of 95% in room air. On auscultation, no pathological finding was detected. Laboratory results revealed a normal complete blood count and basic metabolic profile. Thorax CT scan located a 26x28 mm cystic lesion in the subcarinal region containing homogeneous, low-density fluid (Figure 1).
 Click Here to Zoom |
Figure 1: Thorax CT showing the subcarinal cyst. |
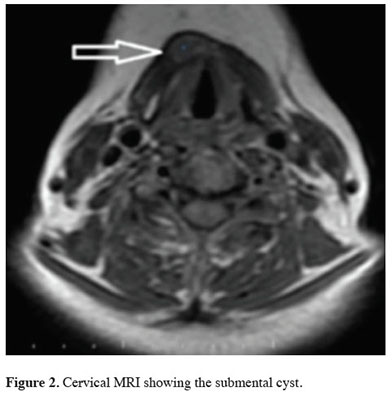
In the operation preparation period, ultrasonography of the neck was made due to her history of a multinodular goiter, which showed a submental cyst that revealed a thyroglossal duct cyst. The radiology and Ear-Nose-Throat specialist recommended a follow-up.
A cervical and thoracal MRI was performed to evaluate the relationship between subcarinal and submental cysts with the surrounding tissues or organs (Figure 2). The first lesion measuring 6x13 mm was located in the middle line of the submental region, and it was isointense in T1W1s and hyperintense in T 2W2s. The other lesion that was located paraesophageal in the subcarinal region showed a hyperintense image on T1W1s, and isointense in T2W2s, and was measured 26x28 mm (Figures 1,2). By comparing with the previous CT scan reported, it was determined that the subcarinal cyst had grown in size within 3 years.
 Click Here to Zoom |
Figure 2: Cervical MRI showing the submental cyst. |
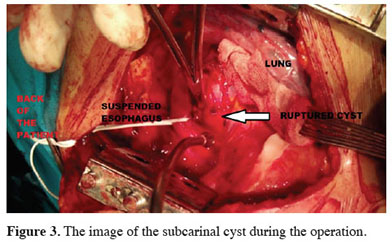
A right posterolateral thoracotomy was performed for the excision of the mediastinal cyst. The mediastinal pleura was dissected at the subcarinal-hilar level. It was observed that the lesion was partially attached to the esophageal muscle layer with the appendix. No connection with the bronchial system was observed. The appendix was not explored. The cyst ruptured spontaneously without opening its contents. The greenish cyst contents were discharged. At the level of the lesion, the esophagus was suspended and dissected circumferentially. The appendix of the cyst, which was partially embedded in the esophageal muscular layer, was excised by ligation with a 2/0 silk suture without any damage to the esophageal mucosa. The esophageal wall incision was closed with 2/0 silk interrupted sutures (Figure 3). The postoperative period was uneventful. The patient was followed up for three years.
 Click Here to Zoom |
Figure 3: The image of the subcarinal cyst during the operation. |
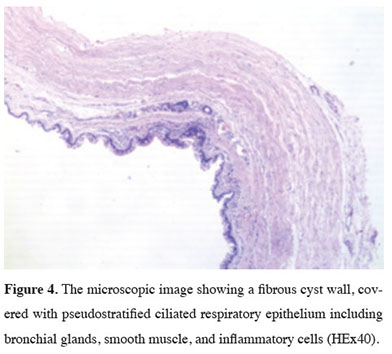
Pathological examination observed a fibrous cyst wall that was edematous that covered with pseudostratified ciliated respiratory epithelium which included bronchial glands, smooth muscle, and inflammatory cells (Figure 4). All these findings were reported in agreement with the bronchogenic cyst. There was no finding suggestive of malignancy. Written informed consent was obtained from the patient for the publication of her data.
 Click Here to Zoom |
Figure 4: The microscopic image showing a fibrous cyst wall, covered with pseudostratified ciliated respiratory epithelium including bronchial glands, smooth muscle, and inflammatory cells (HEx40). |
Discussion
In humans, a range of foregut anomalies can occur depending on the region of the foregut. Many of these defects result from abnormal morphogenesis of endodermal tissue, suggesting that there is a common developmental mechanism between the organ systemsOn the 28th day of the embryonic period, the esophagus and laryngotracheal groove are together in the same circular canal. The inner part of this canal is composed of endodermal cells, while the outer part consists of mesodermal cells. The cells in the foregut endoderm are multipotent cells that develop the thyroid, thymus, esophagus, lung, liver, pancreas, stomach, and biliary systems. The transformation of these organs and systems initiates from the endoderm and mesoderm, depending on the dose, by the Transforming Growth Factor B (TGF β) signaling released from the primitive node [6]. The foregut endoderm cells start polarizing to the ventral and dorsal regions. The development of the trachea from the endoderm cells occurs by polarizing to the ventral area and the development of the esophagus occurs from the dorsal regionally endoderm cells when foregut endoderm cells start to split into two regions. Certain molecules play an important role in polarizing and splitting this dorsal/ventral. Previous studies showed that the Sox2 gene in the dorsalization of the esophagus, the Nkx2.1 gene is effective in the ventralization of the trachea [7,8]
This balance between Nkx2 and Sox2 is provided by the proteins Noggin, FGF, Wnt, and Shh that are found in the mesoderm surrounding the endoderm and play a role in the development of body tissue. Genetic and epigenetic mutations in these genes cause foregut separation distortion/failure or epithelial/mesenchymal abnormal differentiation. Although the pathogenesis of bronchogenic cysts is currently unclear, several theories have been proposed. It has been suggested that the development of the bronchogenic cyst is caused by the mutations of the Wnt gene [8].
A thyroglossal duct cyst was reported incidentally in the neck USG was performed due to a previous history of thyroid disease in the patient who did not have a primary neck complaint. In our case, a thyroglossal duct cyst was detected with a bronchogenic cyst. To the best of our knowledge, this case is the first report featuring two foregut anomalies. The thyroglossal duct cyst is one of the foregut anomalies that is commonly seen in the cervical region. The primordial thyroid gland develops from the endoderm that originates at the base of the tongue (foramen cecum) and descends through the anterior of the hyoid bone to arrive at its final position [9]. The pyramidal lobe on the thyroid gland is a residue of the persistent thyroglossal duct. Additionally, the aperture of the duct anywhere through the descent of the thyroid gland can cause the development of a thyroglossal duct cyst. The most typical presenting symptom is an upper midline mass intimately associated with the strap muscles around the neck, which is mobile upon tongue protrusion or swallowing.
Bronchogenic cysts are one of the most common foregut malformations, usually occurring along the tracheobronchial tree in the mediastinum. Approximately two-thirds of it is located in the mediastinum and the one-third in intraparenchymal. It can also be located in the mediastinum in the paratracheal, subcarinal, hilar, and esophageal regions. Other unusual locations, such as the pericardium, thymus, subcutaneous, diaphragm, retroperitoneum, gastroesophageal junction, and cervical region, have also been reported [1-3].
The symptoms of the bronchogenic cyst may vary depending on its location, size, and complications (e.g., pressure symptoms, cyst hemorrhage, or infection). Typically, bronchogenic cyst infections are observed when they are associated with the trachea-esophageal lumen. However, a connection between the trachea-esophageal lumen and the cyst may not always be demonstrated radiologically. The heterogeneity of the cyst and the increase in cyst size in the radiological follow-up may be the best indicator to confirm that it’s infected or associated with the trachea-esophageal lumen.
Additionally, cysts are isointense on T1W1s MR images. However, when infected, the cyst’s intensity is increased on T1W1s images [10]. In our case, T1W1s images were hyperintense. This situation explained the reason for the recently increased symptoms of our patient. Although the relationship of the cyst with the esophageal lumen could not be fully demonstrated in our case, the increase in cyst’s density in the MRI images, the increase of the cyst’s size in follow-up thorax CT scans, and the infection findings in histopathological evaluation suggested that there may be a millimeter-sized connection between the esophagus and the cyst.
Bronchogenic cysts cause symptoms associated with compression of the surrounding organs and tissues [11-13]. The most serious complication in this is infection and cyst rupture. There are reports of malignancy in the cyst due to recurrent infections [2].
In conclusion, bronchogenic cysts should be operated on at the earliest as possible due to the complications and should also be evaotherin terms of other accompanying foregut anomalies. A detailed examination and radiological examination should be kept in mind for other foregut anomalies that may accompany it in the evaluation of bronchogenic cyst cases.
Declaration of conflicting interests
The authors declared no conflicts of interest with respect to the authorship and/or publication of this article.
Funding
The authors received no financial support.
Authors’ contributions
HGB,SK,AZ: conceived and designed the current case report, co-wrote the paper, collected the clinical data. The authors discussed the case under the literature data together and constituted the final manuscript.
Reference
1) Ballehaninna UK, Shaw JP Brichkov I. Subdiaphragmatic bronchogenic cyst at the gastroesophageal junction presenting with Dysphagia: a case report. Surg Laparosc Endosc Percutan Tech 2013; 23: 170-2.
2) Moon S.M, Lee S.M, Kang H, Choi H.J. Presternal subcutaneous bronchogenic cyst in adolescence: a case report and unusual ultrasonographic findings. Medicine (Baltimore) 2017; 96: e6054.
3) Koga Y, Uchiyama A, Noshiro H, Rai M, Miyatake E, Shimizu S et al. Complete extirpation of a bronchogenic cyst causing recurrent laryngeal nerve palsy by thoracoscopy: report of a case. Surg Today 2006; 36: 79-81.
4) Ott K, Sendler A, Heidecke CD, Becker K, Stein HJ, Siewert JR et al. Bronchogenic cyst of the esophagus with high tumor marker levels: a case report and review of the literature. Dis Esophagus 1998; 11: 130-3.
5) Sundaramoorthi T, Mahadevan R, Nedumaran K, Jayaraman S, Vaidyanathan KR. Intrabronchial rupture of the bronchogenic cyst. An Thorac Surg 2009; 87: 1919-20.
6) Shen MM. Nodal signaling: developmental roles and regulation. Development 2007; 134: 1023-34.
7) Zaw-Tun H.A. The tracheoesophageal septum-fact or fantasy? Origin and development of the respiratory primordium and esophagus. Acta Anat 1982; 114: 1-21.
8) Li C, Xiao J, Hormi K, Borok Z, Minoo P. Wnt5a participates in distal lung morphogenesis Dev Biol 2002; 248: 68-81.
9) Chou J, Walters A, Hage R, Zurada A, Michalak M, Tubbs RS et al. Thyroglossal duct cysts: anatomy, embryology, and treatment. Surg Radiol Anat 2013; 35:875-81.
10) Kocaoglu M, Frush DP, Uğurel MS, Somuncu I. Bronchopulmonary foregut malformations presenting as mass lesions in children: spectrum of imaging findings. Diagn Interv Radiol 2010; 16: 153-61.
11) Tomita SS, Wojtczak H, Pickard R, Vazquez WD. Congenital cystic adenomatoid malformation and bronchogenic cyst in a 4-month-old infant. Ann Thorac Cardiovasc Surg 2009; 15: 394-6.



