

2Department of Pathology, Yedikule Chest Disease and Surgery Training and Research Hospital, Istanbul, Turkey DOI : 10.26663/cts.2017.0023
Summary
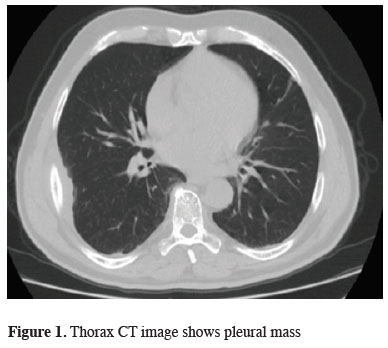
Extramedullary plasmacytoma (EMP) is a plasma cell neoplasm of soft tissue without bone marrow involvement or other systemic characteristics of multiple myeloma. A 68 year-old male presented with haemoptysis of 3 months. Computed thorax tomography (CT) revealed a 3x5 cm pleural mass adjacent to right lower lobe. The mass was diagnosed as pleural plasmacytoma.Introduction
Extramedullary plasmacytoma (EMP) is a plasma cell neoplasm of soft tissue without bone marrow involvement or other systemic characteristics of multiple myeloma. EMPs are rare and mainly emerge in the upper sections of respiratory and digestive tracts. Few clinical studies have been conducted because of the rarity of EMP. Thorax EMPs are presented mostly as mediastinal masses in reported cases. Pleural plasmacytoma appear to be rarer than mediastinal plasmacytoma [1-4].Herein we report a rare unusual presentation of EMP in a 67-year-old male with a pleural mass observed on PET, presented with hemoptysis and back pain.
Case Presentation
A 68 year-old male presented with haemoptysis of three months. No fever, chest tightness, bone pain, dispnea or weight loss was noted. He has been using antiaggregants due to a coronary stent. His breathing was slightly coarse without rales or rhonchi on auscultation. His chest radiography revealed a right pleural shadow, the computed thorax tomography (CT) revealed a 3x5 cm pleural mass adjacent to right lower lobe (Figure 1). Tracking back to his history, he was a smoker, without occupational or environmental exposure to air pollutants or micro-organisms. No family member died of lung cancer before.
 Click Here to Zoom |
Figure 1: Thorax CT image shows pleural mass |
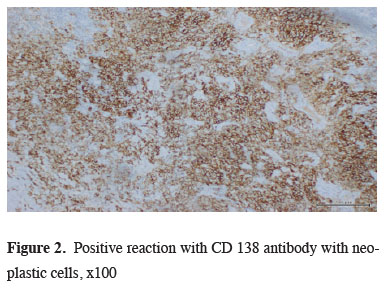
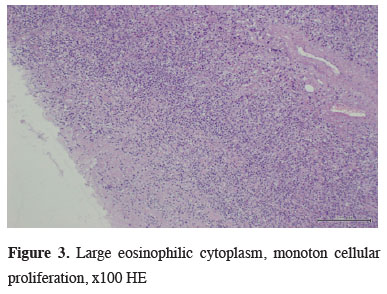
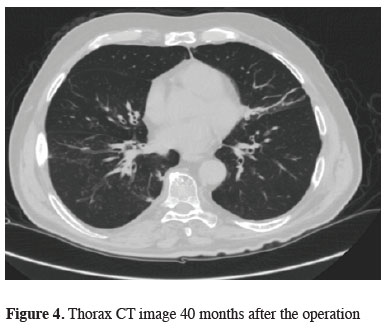
The bronchoscopic examination revealed no endobronchial lesion or abnormal secretions. A pulmonary function test revealed no defect. The whole body positron emission tomography (PET-CT) revealed no other lesion other than right lower pleural mass which had standardized uptake value (SUV) of 5.0. The hemogram, leukocyte differentiation count, and coagulation values were all within normal limits. A CT-guided biopsy, trans-thoracic thin needle aspiration, was performed to conduct a histopathologic diagnosis for the pleural mass, but the result was nonspecific. A biopsy through video-assisted thoracoscopic surgery (VATS) was planned. A 2.5 cm working incision in seventh intercostal midaxillary line and a 11 mm scope port were designed for removing the 3x5 cm pleural mass localized on 5th costal area. The microscopic examination showed a solid mass made up mostly of plasma cells. These tumor cells stained positively for kappa light chains and CD138, but negatively for lambda chains. (Figures 2,3) After confirming that the pleural mass was pleural plasmacytoma, the patient received a series of related evaluations such as serum calcium, urine Bence-Jones protein and plasma electrophoresis for M protein detection. However, all were negative. The skull, spine and pelvis X-ray revealed no osteolytic lesions. The bone marrow biopsy revealed normal patterns of cell distribution. Finally, the patient was referred to the oncology department for radiotherapy. He received external beam radiotherapy 35 Gy in 15-20 fractions over 3-4 weeks which caused radiation pneumonitis. He is on follow-up every 6 months up to date (Figure 4).
 Click Here to Zoom |
Figure 2: Positive reaction with CD 138 antibody with neoplastic cells, x100 |
 Click Here to Zoom |
Figure 3: Large eosinophilic cytoplasm, monoton cellular proliferation, x100 HE |
 Click Here to Zoom |
Figure 4: Thorax CT image 40 months after the operation |
Discussion
Plasma cell neoplasms is classified as, multiple myeloma (bone marrow and other systemic involvements), solitary myeloma (bone plasmacytoma), extramedullary (soft tissue) plasmacytoma, and plasmablastic sarcoma [1]. EMP, which belongs to the category of non-Hodgkin's lymphoma, is present in about 3% of all plasma cell neoplasms [1,2]. It is defined as a soft-tissue plasma cell tumor occurring in the absence of systemic signs of multiple myeloma, such as bone osteolytic lesions, plasma cell infiltration in bone marrow, lytic bone lesion, or serum or urine myeloma protein [3]. EMP affects males three to four times more often than females, with an average age of 55. However, one third of patients with EMP are under 50 years old [3,4]. The EMPs are located predominantly at the upper aero-digestive tract. Pulmonary plasmacytoma was first reported by Gordon and Walker in 1944 [5].Diagnosis of undetermined pulmonary nodular or pleural lesions can be accomplished by transbronchial biopsy, CT guided needle biopsy, as well as surgical biopsy through the VATS or open thoracotomy [6,7]. VATS has been increasingly used for the diagnosis or treatment of undetermined solitary or multiple pulmonary nodules because it is more accurate in diagnosis than needle biopsy and less invasive in treatment than the open procedure [8]. If the result of transthoracic needle biopsy was specific to plasmacytoma, then we would not have performed VATS procedure.
The EMP should be differentiated from other plasma cell tumors. There should be no systemic signs to exclude the possibility of multiple myeloma. In addition, the EMP should also be differentiated from other types of plasma cell tumor, such as reactive plasmacytoma and plasma cell granuloma, or lymphoma such as marginal and immunoblastic subtypes [2,9]. EMP is positive for CD138 and monoclonal cytoplasmic kappa light chain expression of malignant plasma cells [2].
Radiotherapy is the treatment of choice for pleural plasmacytoma because like other plasma cell tumors, EMPs are highly radiosensitive with 80 to 100% of patients successfully achieving local control and with a 50% to 65% ten-year disease-free survival rate [9]. There is no published evidence for the role of adjuvant chemotherapy in the treatment of solitary extramedullary plasmacytoma.
The prognosis of patients with EMP is usually better than those with multiple myeloma. The EMPs, unlike solitary myeloma, advances to multiple myeloma only in a minority of cases. Our patient is observed in each 6 month due to the risk of multiple myeloma formation in patients with plasmacytoma.
We wanted to share this case report to remind our colleagues that plasmacytomas can present as solitary pleural masses and, surgery is used only for the diagnosis. Each PET positive lesion should be explored by minimal invasive methods. As aggressive surgery is not a treatment for pulmonary plasmacytomas, after diagnosis, radiotherapy and oncological follow-up should be appropriate.
Declaration of conflicting interests
The authors declared no conflicts of interest with respect to the authorship and/or publication of this article.
Funding
The authors received no financial support.
Reference
1) Fanning SR, Hussain MA, Perez-Zincer F. Plasmacytoma, extramedullary. Emedicine 2006 http://www.emedicine.com/med/ topic2532.htm.
2) Dimopoulos MA, Hamilos G. Solitary bone plasmacytoma and extramedullary plasmacytoma. Curr Treat Options Oncol 2002; 3: 255-259.
3) Galieni P, Cavo M, Pulsoni A, Avvisati G, Bigazzi C, Neri S, et al. Clinical outcome of extramedullary plasmacytoma. Hematologica 2000; 85: 47-51
4) Holland J, Trenkner DA, Wasseman TH, Tinberg B. Plasmacytoma. Treatment results and conversion to myeloma. Cancer 1992; 69:1513-1517.
5) Gordon J, Walker G. Plasmacytoma of the lung. Arch Pathol 1944; 37: 222-4.
6) Miller DL. Management of the subcentimeter pulmonary nodule. Semin Thoracic Cardiovasc Surg 2002; 14: 281-285.
7) Whyte RI. Advances in the staging of intrathoracic malignancies. World J Surg 2001; 25: 167-73.



