

2Department of Thoracic Surgery, Istanbul Bakirkoy Sadi Konuk Training and Research Hospital, Istanbul, Turkey
3Department of Thoracic Surgery, Memorial Bahçelievler Hospital, Istanbul, Turkey DOI : 10.26663/cts.2019.00127
Summary
Foreign body reaction and deep wound infection (DWI) following sternal resection and reconstruction represent a serious problem. In recent years, negative pressure wound therapy (NPWT) have been used in clinical practice for treatment of DWIs. However, publications regarding the use of NPWT for the prosthetic material-related inflammation and DWI are yet quite rare. We present a very rare case, which is characterized with foreign body reaction and DWI after sternal reconstruction for a giant chondrosarcoma with the treatment of surgical debridement and NPWT.Introduction
Chest wall resection and reconstruction with prosthetic material will yield satisfactory results in most patients [1]. Sternal wound infections are rare, complicating 4.6% of sternal reconstructions [2]. Their consequences are severe, however, with high mortality, morbidity, and prolonged hospital stay. Chapelier et al [3] reported that required removal of the composite prosthesis with reoperations in four patients (10.5%) for local septic complications. We report a foreign body reaction and deep sternal wound infection (DWI) after sternal reconstruction for a giant chondrosarcoma is treated by using negative pressure wound therapy (NPWT) and surgery.Case Presentation
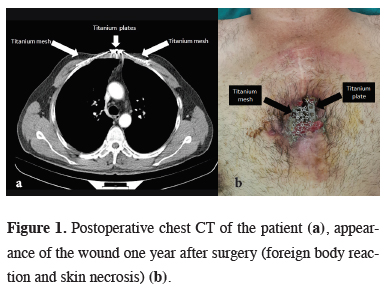
A 46-year-old male was admitted with chest pain and a mass of the anterior chest wall. Computed tomography of chest detected a sternal tumor destroying part of sternum body, which was 6x9 cm in diameter. The patient underwent a radical unblock resection of an 8x11 cm portion of anterior chest wall including the second and third costochondral joints bilaterally, and the tumoral mass with a 2-cm margin of macroscopically normal surrounding tissue. The large chest wall defect was reconstructed with titanium contourable mesh and two titanium straight plates.Histopathology was reported as low-grade chondrosarcoma. There was no problem in clinical condition, no sign of tumor relapse, the thoracic wall was stable (Figure 1a). One year after the surgery patient presented with DWI. We observed foreign body reaction and skin necrosis (Figure 1b).
 Click Here to Zoom |
Figure 1: Postoperative chest CT of the patient (a), appearance of the wound one year after surgery (foreign body reaction and skin necrosis) (b). |
We performed surgical debridement of necrotic sternum and skin including the previous surgical incision scar and removed the titanium mesh and two plates under general anesthesia (Figure 2a).
 Click Here to Zoom |
Figure 2: Peroperative image showing surgical debridement (a), primary suturation (b), postoperative view (after NPWT the wound was repaired by split thickness skin graft) (c). |
The lower and upper portions of the cruciform incision was sutured primarily, and then NPWT was applied to the central area that lost excess skin and tissue (Figure 2b).
We used NPWT for accelerated granulation tissue formation and decreased wound secretion (approximately complete after 6 sessions). During therapy, the maximum negative pressure was kept at 50 mmHg.
After the sufficient thickness granulation tissue formation, the wound was repaired by split thickness skin graft. The patient was satisfied with both cosmetic and functional results. He is healthy without any complaints at one year postoperatively (Figure 2c).
Discussion
Various prosthetic materials have been described to reconstruct large defects of the anterior chest wall, such as polypropylene mesh, metal implants, methyl-methacrylate and titanium plating [3]. It is important to promote good pulmonary function, protect the intrathoracic organs from infection and trauma, and maintain cosmetic integrity. All of these advantageous prosthetic materials might be rejected, displaced or cause septic complications such as foreign body reaction [2]. In such cases, the prosthetic material should be removed. However, this application may not be enough due to the tissue and skin loss. Therefore some studies recommended the concomitant use of the NPWT device allowing the sufficient thickness granulation tissue formation [4]. Nevertheless, the studies comparing NPWT with conventional therapy are all retrospective in nature and reinforce the need for randomized controlled trials in order to more accurately establish differences in outcomes between NPWT and conventional therapy [5]. There are few studies involving the use of NPWT for the prosthetic material-related inflammation and deep sternal infection. In this case, we used titanium mesh for sternal reconstruction. One year after surgery, foreign body reaction and DWI were detected. We initially performed surgical debridement of the necrotic tissue, and then used NPWT treatment to accelerate granulation. Most surgeons now consider NPWT devices to be the fi rst-line treatment for deep sternal wound infection however, we used to NPWT as a bridge therapy to cutaneous reconstruction.In conclusion, the use of NPWT for the prosthetic material-related inflammation and DWI is very rare. The management and treatment of these cases are difficult and besides surgery, NPWT devices could be used as a bridge therapy. We believe that using NPWT after surgical debridement of necrotic tissue provides healing in a short time.
Declaration of conflicting interests
The authors declared no conflicts of interest with respect to the authorship and/or publication of this article.
Funding
The authors received no financial support.
Reference
1) Çitak N, Çelikten A, Metin M, Pekçolaklar A, Gürses A. Radical resection of a giant recurrent chondrosarcoma of the anterior chest wall. Gen Thorac Cardiovasc Surg 2011; 59: 512-4.
2) Briccoli A, Manfrini M, Rocca M, Lari S, Giacomini S, Mercuri M. Sternal reconstruction with synthetic mesh and metallic plates for high grade tumours of the chest wall. Eur J Surg 2002; 168: 494-9.
3) Chapelier AR, Missana M-C, Couturaud B, Fadel E, Fabre D, Mussot S, et al. Sternal resection and reconstruction for primary malignant tumors. Ann Thorac Surg 2004; 77: 1001-7.



