

Summary
Background: Pectus excavatum (PE) is the most commonly seen chest wall deformity of childhood age. One of the most widely accepted methods in preoperative patient evaluation is the pectus index. In this study, it is aimed to measure the depth perception which is not aesthetic; aimed to establish an objective criteria which is simple, cheap, effective, and can be measured with physical examination or anthropometry instead of radiological examination dependent measurements.Materials and Methods: 18 patients who were admitted to our clinic between May 2015 and August 2016 with complaints of PE deformity and who were planned for surgical repair were included in the study. Sternal deformity’s depth, anthropometric measurements, pectus indexes, echocardiography, and pulmonary function test results and patient symptoms were classified.
Results: 18 patients were included in the study. The mean patient age was 14.27 years. One patient had mild mitral insufficiency and a flappy mitral front leaflet. One patient had mitral valve prolapse. No restrictive or obstructive results were observed in the pulmonary function test. There was no significant differences between the pectus index and sternal depth.
Conclusions: According to this study, there is a surgical indication in patients whose sternal depth is 1.2 cm and higher, regardless of the pectus index.
Introduction
The normally accepted body build involves a long chest wall and low anteroposterior depth in tall and slender people and deeper anteroposterior depth in short and bulky people. The replacement of cylindrical structures observed during childhood with the expansion of the chest in the transverse plane as age progresses is considered normal [1]. All other body build types are considered thoracic wall deformities.There are various types of thoracic wall deformities, including the absence of one or more ribs, shortness of ribs, bifurcation of ribs, bridging, or posterior fusions of ribs, pectus excavatum (PE), pectus carinatum, sternal cleft, ectopia cordis, and Poland syndrome [2].
PE is a congenital chest wall deformity that presents with posterior depression of the middle and lower one-third of the sternum and posterior curvature of the costal cartilages [3].
Patients may be asymptomatic or may present with esthetic concerns as well as exertional dyspnea, dyspnea at rest, chest pain, and palpitation [4].
Various methods have been proposed for the evaluation and classification of these deformities. Thirty-two indexes have been defined for the degree of PE, treatment planning, and postoperative evaluation [5]. However, the pectus index is the most preferred and is included in the Kelly criterion.
This study aimed to determine whether the decision to perform surgery could be made by conducting a physical examination to quantitatively determine non-esthetic sternal depth measurements for pectus excavatum.
Methods
This prospective, case-control study was approved by the ethics committee for non-interventional clinical research of the Selçuk University Faculty of Medicine (approval number, 2015/222). Verbal and written informed consents were obtained from all patients. Further, this study was designed in accordance with the principles of the Declaration of Helsinki.The study included total 18 patients who were admitted to the Department of thoracic surgery of the Selçuk University Faculty of Medicine between May 2015 and August 2016 with complaints of PE deformity, who had no history of surgery due to PE, and who were examined by two thoracic surgeons and advised to undergo minimally invasive PE repair owing to a diagnosis of moderate-to-severe PE. Those patients who were not indicated for surgery, those who had previously undergone PE repair, and those with mild PE revealed upon physical examination were excluded from the study. Mild PE was evaluated based on the definition of the moderate and non-severe group of patients who did not require surgical intervention and could be treated using physical therapy or vacuum treatment [6].
Examinations
All patients underwent non-contrast computed tomography (NCTT). The pectus index was calculated using computed tomography. The ratio of the horizontally longest distance through the rib cage to the distance between the sternum and vertebrae at the deepest point of the PE in the axial section of the NCTT was used to calculate the pectus index. We also calculated the sternal depression index using computed tomography. This index was obtained by calculating the ratio of the maximum internal sagittal diameter of the left hemithorax to the distance between the anterior wall of the vertebral column and the posterior margin of the deepest part of the sternum [5].
The patients were enquired regarding any cardiopulmonary complaints they may have had during their initial visits. Pulmonary function test (PFT) and echocardiography (ECHO) were performed for all patients. Besides, the presence of pathologies due to PE in ECHO and PFT was also assessed.
Anthropometric measurements
The parameters measured were as follows:
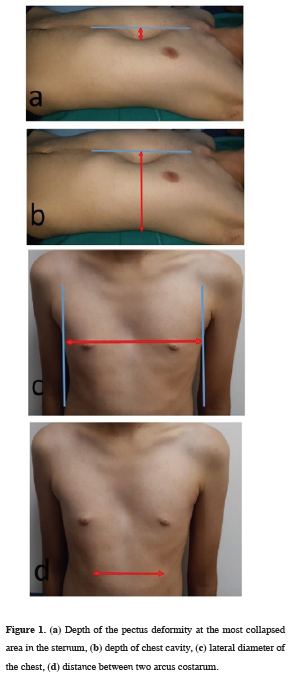
• Depth of the pectus deformity at the most collapsed area in the sternum (Figure 1a),
• Depth of chest cavity (Figure 1b),
• Lateral diameter of the chest (Figure 1c),
• Distance between two arcus costarum (Figure 1d),
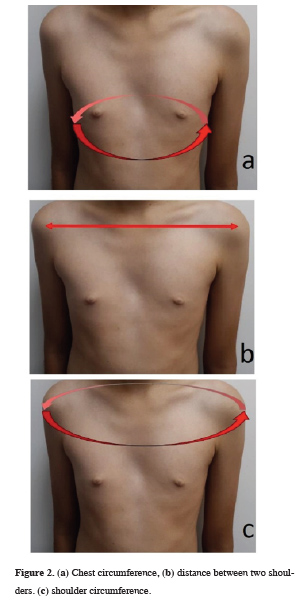
• Chest circumference (Figure 2a),
• Distance between two shoulders (Figure 2b),
• Shoulder circumference (Figure 2c),
• Anthropometric index (the ratio of the depth of deformity in the sternum to the anterior–posterior distance of the rib cage).
 Click Here to Zoom |
Figure 1: (a) Depth of the pectus deformity at the most collapsed area in the sternum, (b) depth of chest cavity, (c) lateral diameter of the chest, (d) distance between two arcus costarum. |
 Click Here to Zoom |
Figure 2: (a) Chest circumference, (b) distance between two shoulders. (c) shoulder circumference. |
Threshold and Statistical Analysis
The anthropometric index, sternal depression index, anthropometric distances, and pectus index of the patients with PE deformities were statistically measured and compared.
Based on the sternal depression index, the severity of the PE deformity was considered mild when the index was <2.4, moderate when the index was 2.4 - 2.9, and severe when the index was >2.9.
Those patients with a pectus index >3.25, which is the limit value according to the Kelly criteria, were grouped as having a positive pectus index PI (+), whereas those with a pectus index <3.25 were grouped as having a negative pectus index PI (−).
Homogeneity tests were performed, and both groups were compared using student’s t-test. The statistical package for the social sciences (SPSS) software v.16.0 was used for statistical analysis.
Results
Total of 18 patients (5 females and 13 males) were included in the study. The mean patient age was 14.27 (7-24) years.
Measurement results by conventional indices
The mean pectus index of all patients was 3.51 (range, 2.22 - 4.80). Of the 18 patients included in the study, 9 were PI (+) and 9 others were PI (−). The mean pectus index of the patients in the PI (+) group was 4.19 (range, 3.50 - 4.80), whereas that of the patients in the PI (−) group was 2.84 (2.22 - 3.17).
The total number of patients with mild PE based on the sternal depression index was 13. Based on this index, four patients had moderate PE and one had a severe deformity. The mean sternal depression index of all patients was 2.09 (range, 1.50 - 2.91).
The mean anthropometric index of all patients was 0.13 (range, 0.07 - 0.29).
The mean depth measurement of all patients was 2.2 (range, 1 - 3.5) cm. The mean depth of the patients in the PI (+) group was 2.28 (range, 1 - 3.5) cm, whereas that of the patients in the PI (−) group was 2.11 (range, 1.2 - 3) cm (Tables 1, 2).
Table 1: Demographic characteristics and index results of the patients included in the study.
Table 2: The means of PI (+) and PI (−) groups and all patients according to various indices.
Anthropometric measurement results
The mean shoulder circumference of all patients was 80.83 (range, 61 - 102) cm. The mean distance between the two shoulders of all patients was 28.61 (range, 16 - 38) cm.
The mean distance between the two arcus costarum of all patients was 12.16 (range, 5 - 22) cm. The mean chest circumference of all patients was 73.61 (range, 60 - 96) cm. The mean lateral diameter of the chest of all patients was 24.94 (range, 12 - 31) cm.
The mean distance between the anterior–posterior thoracic diameter of all patients was 15.88 (range, 11 - 20) cm. (Table 3).
Cardiopulmonary results
One patient experienced pain and constriction, another patient experienced only constriction. The remaining 16 patients did not experience any cardiac or pulmonary issues or discomfort. Echocardiography results were completely normal in 16 of the 18 patients (88.8%). One patient had mild mitral insufficiency and a flappy mitral front leaflet. One patient had mitral valve prolapse (MVP). No restrictive or obstructive results were observed in PFT.
Statistical results
The variance homogeneity test results of the groups with positive and negative pectus indexes were statistically significant for all variables. The Levene’s test for equality of variances values was all greater than the p value (0.05). In other words, the variances of all the variables were equal, and the independent sample t-test (Student’s t-test), which is a paired comparison test, could be applied. When the groups with positive and negative pectus indexes were compared, a statistically significant difference was observed between the groups in terms of the mean sternal depression index, mean lateral diameter of the chest, and mean distance between the anterior–posterior thoracic diameter (p < 0.05). No statistically significant difference was observed between the groups in terms of the anthropometric index, depth, shoulder circumference, the distance between two shoulders, the distance between two arcus costarum, and mean chest circumference (p > 0.05) (Table 4).
Table 4: Statistical evaluation of the mean of anthro-pometric measurement parameters.
Discussion
The PE is the most common congenital chest wall deformity observed during childhood, and it is more common in men with a ratio of 3 - 9:1 [7,8]. Of the 18 patients, 5 were female and 13 were male. With a ratio of 3:1, the ratio of females in our study was lower than that reported in the literature but somewhat similar.The pectus index, which defines the relationship between thoracic height and diameter, was defined by Haller in 1987. The index was used as a decision-making tool for managing PE. The pectus index is measured using thorax computed tomography of the axial section at the section with the maximum deformity of the thorax [9].
The generally accepted Kelly criteria for surgery indication are as follows: 1; progressive and symptomatic PE deformities, 2; restrictive and/or obstructive disease indicated by the PFT, 3; cardiac compression or displacement, atelectasis in the lung, and a pectus index ≥3.25 based on computed tomography 4; cardiac anomalies, such as MVP or branch block, and 5; recurrent PE after unsuccessful repair [10,11].
In the literature, severely decreased lung function and vital capacity have been defined in patients with a pectus index >3.6 [12]. In the present study, 8 patients had a pectus index >3.6, and their PFT results were normal. Further, the ECHO results of 7 of the 8 patients with a pectus index >3.6 were completely normal. In terms of cardiac results, our study is consistent with the reported literature. Seven of out 8 patients who were admitted to our clinic with esthetic concerns were described as “operable” by the clinician.
Glinkowski et al emphasized that physiological and cosmetic indications for surgical treatment of PE have become more prominent, and they attributed it to the development of minimally invasive surgical techniques [13]. This study is one of the several studies associating PE surgeries to esthetic reasons. In our study, we observed that the concept of depth that appears to the eye as “deep” was ≥1 cm. The smallest depth criterion in the study, i.e., 1cm, was observed in one patient, and the pathology in this patient was detected via ECHO. Of the 17 patients admitted to the clinic with a depth of ≥1.2 cm, 88.2% had only depth complaints and 82.3% had no findings on ECHO or PFT. Only 2 of the 18 patients had cardiopulmonary complaints. The sternal depth of these patients was measured as 1.8 and 3 cm. These results indicate that the patients’ complaints are mostly associated with depth or hollowness. All these data suggest that esthetic reasons may be a new indication for surgery in patients with a depth of ≥1.2 cm who present only with sternal depression complaints.
The sternal depression index, a method defined in the literature, is used for classifying the pectus severity. The sternal depression index is the ratio of the maximal sagittal height of the left hemithorax to the minimum distance between the posterior wall of the sternum and the vertebral anterior surface of the same section at the point where the sternum is the narrowest. This index measures sternal depression, i.e., the severity of the PE. It is defined as mild PE if the ratio <2.4, moderate PE if it is between 2.4 - 2.9, and as severe PE if it is >2.9 [5].
According to this classification, 13 patients had mild, 4 had moderate, and 1 had a severe deformity. We also found that 72.2% of the patients for whom pectus deformity was planned to be corrected had a mild deformity. This high rate indicates that there exist indications other than the sternal depression index that drive both the patient and clinician to surgery. One interpretation regarding this study suggests that the primary indication is “esthetic concerns of the patient” and the conclusion of the clinician regarding “the presence of PE.” However, this evaluation may not be possible only by assessing the sternal depression index.
In this study, the mean sternal depression indexes in the PI (+) and (−) groups were 2.37 and 1.81, respectively, and the difference was statistically significant (p = 0.001). This difference indicates that the sternal depression index is correlated with the widely used pectus index, which is based on the Kelly criteria. However, the fact that the mean sternal depression index of all patients was <2.4 suggests that the positivity of the pectus index is not correlated with the severity of the PE. This signifies that if the severity of the PE is used in determining the indication for surgery, patients other than those with severe deformity can also be operated based on the patient’s complaints or clinician’s evaluation, even if the pectus index is greater than the threshold value.
Anthropometric measurements are important for the accurate documentation and observation of patients. Štefánková et al reported that anthropometry offers applicable and noninvasive methods for the evaluation of the PE and emphasized that these methods should be performed before performing CT [14]. The anthropometric index is a proportional value calculated through anthropometric measurements. It has been included in our study because it is an index that is based on the idea that an inexpensive and effective method, which is easy to learn and apply, may replace conventional methods. However, no statistically significant difference was observed between the patient groups with PI (+) and (−) in terms of anthropometric measurements of the distance between the two arcus costarum, chest circumference, distance between the shoulders, and shoulder circumference. The reason for this result might be that age differences, muscle mass, and sex differences, and structural characteristics of patients might play an important role in the measurement of parameters related to body parts, such as shoulders and chest circumference. In terms of measurements of the anterior–posterior thoracic and lateral diameters of the chest, a statistically significant difference was found between patients with a positive and negative pectus index. No such studies have been reported yet; however, the differences between the two groups indicate that the measurement of these distances may be significant when deciding on surgery.
In this study, the depth of the deformity in the sternum was measured and the results were compared between the PI (+) and (−) groups in cm; however, no statistically significant difference was found. The threshold value of the anthropometric index is 0.12 [5,15]. In our study, the anthropometric indexes in the PI (+) and (−) groups were 0.15 and 0.12, respectively. Although no difference was observed between the two groups, the anthropometric and pectus indexes were correlated in terms of the threshold value. This signifies that a measure based on the metric measurements in the body correlates with the pectus index. This correlation is not surprising because the rationale behind this measurement is the ratio of the depth of the sternal deformity to the anterior–posterior thoracic diameter. A criterion that is correlated with the pectus index is more advantageous as it is easily applicable and does not require tomography. However, the subcutaneous thickness, body mass index, and weight of the patient are thought to play an effective role in this ratio. The significant difference between the two groups in the measurement of the anterior–posterior diameter of the thorax indicates that it is correlated with the calculation of this index.
The mean sternal depths in the PI (+) and (−) groups were 2.28 and 2.11, respectively, and the difference was not statistically significant. This result shows that the depth measurements between the PI (+) and PI (-) groups are not different. In the English literature, depth measurement in PE and the comparison of the pectus index have been very rarely reported. In the present study, the sternal depths were similar among patients who were admitted to our thoracic surgery outpatient clinic and indicated for surgery by the two clinicians.
The indication for surgery was based on the clinician’s physical examination performed when the patient’s complaint was noteworthy or when a significant level of depression was revealed in the physical examination; therefore, the level of sternal depression in the patients was measured in cm. In the present study, there was no difference in the PI (+) and (−) groups in terms of depth; this was interpreted as a confirmation that depth measurement was an indication for surgery regardless of the pectus index. In the literature, according to a survey conducted among thoracic surgeons, 40.7% of the surgeons reported that thoracic indexes were “rarely necessary” or “unnecessary.” Further, 13.6% of the surgeons stated that the pectus index was unnecessary and that 56.32% of the specialists stated that the threshold value of 3.25 was inaccurate for the pectus index [5]. These rates also indicate that thoracic surgeons use different criteria for surgical indications. Among the clinicians who determine the indication for surgery, a considerable number of specialists believe that the pectus index is unnecessary or the threshold value is inaccurate. In the present study, no association was observed between the pectus index and depth, and the use of the pectus index did not affect the indications for surgery and also showed that the requirement of thorax computed tomography is minimal.
Daunt et al reported that the vertebral level was not always the same in all the definitions of “the largest diameter” and “the height in the deepest place” used for calculating the pectus index [16]. Besides, Archer et al, through their study with 433 patients, reported that the diameter and height measurements at each vertebral level were different [9]. In the present study, we determined that the pectus index was correlated with neither the anthropometric indexes nor the patient’s depth measurements.
Mortellaro et al reported that the pectus index was an important factor in determining the anatomical severity of the defect in the PE; however, it is still insufficient to predict the intraoperative and postoperative results [17]. Birkemeier et al reported that although measurement of the pectus index is the most widely accepted method, it showed different rates during expiration, inspiration, and relaxation in NCTT [18]. Accordingly, the pectus index was found to be significantly lower during inspiration than during inspiration and relaxation. All these results affect the measurement of the pectus index and therefore the indication for surgery.
The limitation of our study is that it was a single-center study. Involving more number of patients might provide stronger and better results.
In conclusion, although the pectus index is a generally accepted method under the Kelly criteria for patients with PE in terms of determining the indications for surgery, the results of this study indicate that the pectus index does not correlate with the main complaints and symptoms of the patients. No association could be established between the pectus index and the clinician’s decision for surgery after the clinical evaluation of a patient. The calculation of the pectus index via NCTT scans should not be mandatory in determining the operative criteria in patients with PE. In this context, the depth of the deformity as well as the depth of the anterior–posterior diameter and lateral diameter of the chest determined via metric measurements to be performed during clinical visits of the patients, will be effective in the decision for surgery. It is recommended that NCTT, which has disadvantages like radiation and cost, should not be used in patients unless deemed extremely essential, and patients should be evaluated using simple methods, such as two-way direct chest X-ray, echocardiography, PFTs, and sternal depth measurements.
Declaration of conflicting interests
The authors declared no conflicts of interest with respect to the authorship and/or publication of this article.
Funding
The authors received no financial support for the research and/or authorship of this article.
Acknowledgement
We would like to offer special thanks to deceased Assoc. Prof. Dr. Murat Oncel, although no longer with us, for his support and efforts.
Reference
1) Donnelly LF, Frush DP. Abnormalities of the chest wall in pediatric patients. AJR Am J Roentgenol 1999;173:1595-601.
2) Shamberger RC. Chest Wall Deformities. In: Shields TW, LoCicero III J, Ponn RB, Rusch VW, eds. General Thoracic Surgery. Sixth ed. Philadelphia: Lippincott Williams & Wilkins; 2005:653-81.
3) Işıtmangil T. Primary Repair of Chest Wall Defects. In: Yüksel M, ed. Adult Chest Surgery. İstanbul: Nobel Tip Kitabevi; 2011:986-1053.
4) Koumbourlis AC. Pectus excavatum: pathophysiology and clinical characteristics. Paediatr Respir Rev 2009;10:3-6.
5) Martinez-Ferro M. Indexes for Pectus Deformities. In: Kolvekar SK, Pilegaard HK, eds. Chest Wall Deformities and Corrective Procedures. Switzerland: Springer International Publishing; 2016:35-60.
6) Nuss D, Obermeyer RJ, Kelly RE. Nuss bar procedure: past, present and future. Ann Cardiothorac Surg 2016;5:422-33.
7) Kuru P, Cakiroglu A, Er A, Ozbakir H, Cinel AE, Cangut B, et al. Pectus Excavatum and Pectus Carinatum: Associated Conditions, Family History, and Postoperative Patient Satisfaction. Korean J Thorac Cardiovasc Surg 2016;49:29-34.
8) Alexander J. Traumatic pectus excavatum. Ann Surg 1931;93:489.
9) Archer JE, Gardner A, Berryman F, Pynsent P. The measurement of the normal thorax using the Haller index methodology at multiple vertebral levels. J Anat 2016;229:577-81.
10) Kelly RE Jr. Pectus excavatum: historical background, clinical picture, preoperative evaluation and criteria for operation. Semin Pediatr Surg 2008;17:181-93.
11) Yavuzer Ş, Yüksel M, Öncel M, Sunam GS. Issaka A. Chest Wall Deformities and Surgical Treatment. In: Yüksel M, ed. Thoracic Surgery. Second edition. İstanbul: Nobel Tip Kitabevi; 2015:625-44.
12) Swanson JW, Avansino JR, Phillips GS, Yung D, Whitlock KB, Redding GJ, Sawin RS. Correlating Haller Index and cardiopulmonary disease in pectus excavatum. Am J Surg 2012;203:660-4.
13) Glinkowski W, Sitnik R, Witkowski M, Kocoń H, Bolewicki P, Górecki A. Method of pectus excavatum measurement based on structured light technique. J Biomed Opt 2009;14:044041.
14) Štefánková E, Omaník P, Neščáková E, Stanová B, Cingel V. Metrical evaluation of Slovak patients with pectus excavatum. Surg Radiol Anat 2016;38:663-74.
15) Rebeis EB, Campos JR, Fernandez A, Moreira LF, Jatene FB. Anthropometric index for Pectus excavatum. Clinics (Sao Paulo) 2007;62:599-606.
16) Daunt SW, Cohen JH, Miller SF. Age-related normal ranges for the Haller index in children. Pediatr Radiol 2004;34:326-30.



