

2Department of Pathology, Atatürk Chest Diseases and Thoracic Surgery Training and Research Hospital, Ankara, Turkey
3Department of Thoracic Surgery, Gazi University Faculty of Medicine, Ankara, Turkey DOI : 10.26663/cts.2019.0001
Summary
Background: Large-cell lung carcinoma (LCLC) is a relatively aggressive tumor and constitutes a small proportion of non-small-cell lung carcinoma (NSCLC). The purpose of this study was to investigate the clinicopathological characteristics of LCLC and reclassify patients according to the 2015 World Health Organization (WHO) criteria to improve the diagnosis rate of LCLC.Materials and Methods: The clinicopathological data of 32 patients who were diagnosed as LCLC in our clinic between January 1999 and December 2016 and underwent surgery were retrospectively investigated. The 32 patients with LCLC accounted for 1.6% of the total 1935 patients who were diagnosed as having pulmonary cancer during the corresponding time period at our institution.
Results: There were 30 males and 2 females with a mean age of 56.4 (range, 39-76) years. The ratio of smoking / non-smoking patients was 22/32 (68.7%). Based on the new definition of LCLC, a total of 32 patients with LCLC were detected. 16 patients with null immunohistochemical features, 12 with no stains available, and 4 with unclear immunohistochemical features. Our 1, 3, and 5-year survival rates were 65.6%, 53.1%, and 46.9%, respectively.
Conclusions: According to the new classification, formerly diagnosed LCLCs were mostly reclassified as adenocarcinoma and non-keratinizing squamous cell carcinoma. LCLC, which became a more homogeneous group with the 2015 WHO classification, may significantly benefit from multimodal treatment with surgery.
Introduction
Large-cell carcinoma is a malignant tumor that was classified as two variants: large-cell neuroendocrine carcinoma (LCNEC) and basaloid carcinoma. LCNEC was described in 1991 by Travis et al. [1], and basaloid carcinoma was first described in 1992 [2]. Both variants were recognized as distinct clinicopathological entities with a dismal prognosis by the WHO classification in 1999 [3].In the WHO Classification of 2015, there have been numerous important changes in terms of LCLC according to the 2004 WHO classification. LCLC is one of topics that has had the most specific and greatest changes from the 2015 WHO classification. For example, rare specific cell types: large cell neuroendocrine carcinoma, basaloid carcinoma, lymphoepithelioma-like carcinoma, clear cell carcinoma, and rhabdoid tumor have been removed from the large cell carcinoma group and are no longer considered histologic subtypes [3-6]. In this study, the clinicopathological data from 32 patients with LCLC were retrospectively analyzed, with the aim of summarizing the specific clinicopathological features of LCLC, reclassifying the patients according to the 2015 WHO criteria, thereby improving the definite diagnosis rate of LCLC and showing the results of surgical resection as a treatment, and the postoperative follow-up.
Methods
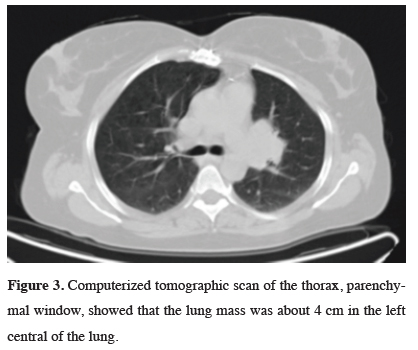
The hospital records of 1935 consecutive patients with non-small-cell lung cancer (NSCLC) who underwent surgery between 1999 and 2016 were reviewed. The preoperative assessments included chest X-ray, and computed tomography (CT) of the chest and upper abdomen (Figures 1-3).
 Click Here to Zoom |
Figure 1: Chest X-ray of the thorax showed that the lung cavitation was about 9 cm in the right lower lung. |
 Click Here to Zoom |
Figure 2: Computerized tomographic scan of the thorax, mediastinal window, showed that the lung cavitation was about 9 cm in the right lower lung. |
 Click Here to Zoom |
Figure 3: Computerized tomographic scan of the thorax, parenchymal window, showed that the lung mass was about 4 cm in the left central of the lung. |
Clinical N2 status was defined by the presence of a lymph node more than 1 cm in a short axis diameter. Positron emission tomography (PET/CT) was routinely used after 2009 (Figure 4).
 Click Here to Zoom |
Figure 4: Positron emission tomography scan of the thorax, showed that the lung mass was about 4 cm in the left central of the lung. |
Spirometry tests were routinely conducted in all patients and preoperative fiberoptic bronchoscopy (FOB) was also performed. Various types of thoracotomies were performed on these patients based on the location of the tumor and we planned pulmonary resection under single-lung anesthesia. We also performed either an anatomic or non-anatomic complete resection while preserving most of the functioning lung tissue. During the operation, undiagnosed tumors were confirmed using frozen section (FS) examinations. For centrally located lesions, FS examination of bronchial margins was performed routinely, with the hope of finding a tumor-free margin. In addition, systematic mediastinal and hilar lymph node sampling was conducted, and mediastinal lymph node dissection was performed if lymph node metastasis was confirmed by FS after sampling. All resected specimens, including the primary tumor and resected hilar and mediastinal lymph nodes, were examined to determine both the tumor histology and the extent of lymph node metastases. All tissues were sent for routine histopathologic examination after the surgery.
Adenocarcinoma, squamous cell carcinoma, and neuroendocrine differentiation were investigated in routine hematoxylin eosin (H&E) preparations of all cases. Immunohistochemical-studied cases were stained with P63, P40, Napsin A, and TTF1. Intracytoplasmic mucin was investigated using the mucin carmine technique. All specimens were reviewed by an experienced pathologist from our institution’s department of pathology according to the revised histologic classification standards of lung cancer for the diagnosis and classification of LCLCs established by the WHO classification (4th edition).
The following parameters were investigated from the medical records: patient sex, age, smoking history, tumor size, tumor location, surgical procedure, pathologic TNM stage, adjuvant chemotherapy, time of recurrence, site of recurrence, response to treatment, and patient outcome. During the follow-up period, these data were prospectively recorded in the database, and then all patients were contacted either in person or by telephone. We performed routine follow-ups 4 times per year, checking symptoms and chest X-rays. We also performed chest CT at least once per year. If abnormal findings were observed, we used PET/CT to evaluate the hilar-mediastinal and extrathoracic lymph nodes, the lung field, and the abdomen.
The data were evaluated using the statistical package program IBM SPSS Statistics 22.0 (IBM Corp., Armonk, New York, USA). The descriptive statistics were as follows: unit number (n), percent (%), mean ± standard deviation (SD), Median (Q1-Q3). The survival curve was calculated by the Kaplan–Meier method and compared using the Log-rank test for the univariate analysis. Categorical variables were compared by Pearson’s Chi-square and Fisher’s exact test. The differences were considered to be significant if the p value was less than 0.05. The normal distribution of the numerical variables was assessed using the Shapiro-Wilk normality test and Q-Q graphs.
Results
At our institution from January 1999 to December 2016, there were 32 LCLCs out of 1935 surgically resected primary lung cancers (1.6%). The mean age of the patients was 56.4 (range, 39-76) years; the male to female ratio was 30:2. Twenty-two patients (68.75%) had a history of smoking. The clinical symptoms were cough and expectoration (n = 10, 31.25%), bloody sputum or hemoptysis (n = 7, 21.87%), chest pain (n = 8, 25%), dyspnea and shortness of breath (n = 7, 21.87%), and fever (n = 3, 9.37%). Before the surgery, 32 patients underwent a sputum exfoliative cytopathology examination. A malignant tumor was confirmed in 5 patients (15.6%) in bronchoscopy, and in 15 patients (46.87%) in CT-guided transthoracic needle biopsy (TTNBx), and a definitive diagnosis was achieved in FS examinations in 11 (34.37%) patients, and postoperatively with mediastinoscopy in one patient.In the CT findings, the maximum diameter of the tumors ranged between 2 and 20 cm, with an average of 4.8 cm. The majority of the tumors were peripherally located (81.25%, 26/32), only 18.75% (6/31) of tumors were centrally located. Twenty-one tumors were located in the right lung (11 superior lobe, 1 middle lobe, 5 lower lobe, 4 near the hilum of the lung) and 11 were located in the left lung (5 superior lobe, 2 lower lobe, 4 near the hilum of the lung). The imaging examination revealed lobulation in 18 cases (56.25%), cavitation in 5 cases (15.62%), atelectasis in 5 cases (15.62%), and mediastinal lymphadenopathy in 7 cases (21.87%). Routine immunohistochemical analysis was performed on 20 specimens.
All 32 patients (including one patient who underwent the mediastinal lymph node biopsy) were diagnosed as have LCLC (Figures 5,6). The tumors were classified as LCLC with unclear immunohistochemical features (12.5%, 4/32), with null immunohistochemical features (LCC-N) (50%, 16/32), and with no available staining (37.5%, 12/32). Left posterolateral thoracotomy was performed in 11 patients, and right posterolateral thoracotomy in 20 patients. Mediastinoscopy was performed in 7 patients and endobronchial ultrasound (EBUS) biopsy in 4. Thirty-one patients received surgical treatment including regional wedge excision (n = 1), lobectomy (n = 17), bilobectomy inferior (n = 3), lobectomy with chest wall resection (n = 2), and pneumonectomy (n = 8). No further surgical resection was applied in one patient because mediastinal lymph node metastasis (N2) was diagnosed with mediastinoscopy. The 7th Tumor, Node, Metastasis (TNM) classification of cancer tissues revealed 3 cases of stage IA, 6 cases of stage IB, one case of stage IIA, 13 cases of stage IIB, 8 cases of stage IIIA, and one case of stage IV. Among them, two patients received neoadjuvant chemotherapy, 17 patients received adjuvant chemotherapy, and 4 patients received postoperative radiotherapy. A total of 3 patients had palliative radiotherapy. One patient gave up chemoradiotherapy after confirmation of the LCLC diagnosis through biopsy of the lymph nodes. Among the 32 patients with LCLC, 21 were followed up for one year; however, 11 patients did not complete the follow-up period.
 Click Here to Zoom |
Figure 5: Large cell carcinoma consists of sheets of large polygonal cells (HEx200). |
 Click Here to Zoom |
Figure 6: Large polygonal cells with vesicular nuclei, prominent nucleoli (HEx400). |
The one-year survival rate of the patients was 65.6%. The three-year survival rate of the patients was 53.1%; 15 patients did not complete the follow-up period. The five-year survival rate of the patients was 46.9%; 17 patients did not complete the follow-up period. At the time of writing, the longest patient follow-up had reached the 125th month, and the patient is still alive. There have been 17 cases of mortality. As seen in our survival curve according to the stage of disease (Table 1 and Graph 1), our results showed the mean 1, 3 and 5-year survival rates were 88.2%, 76.5% and 64.7% in patients who received adjuvant chemotherapy, and 40%, 26.7%, and 26.7% in patients without adjuvant chemotherapy, respectively (Table 2 and Graph 2). Hereby 1, 3, and 5-year survival of patients with adjuvant chemotherapy better then patients without adjuvant chemotherapy (p = 0.05, p = 0.03, p = 0.03). There was no significant difference in survival in patients receiving adjuvant chemotherapy and radiotherapy together (p = 0.594). In addition, there was no significant difference in survival (p = 0.773) among patients who had neoadjuvant chemotherapy. Survival was longer in patients without metastasis (p = 0.029).
Table 1: Survival curve according to the stage.
 Click Here to Zoom |
Graph 1: Survival curve according to the stage. |
 Click Here to Zoom |
Graph 2: Comparison between patients who recieved adjuvant chemotherapy and without adjuvant chemotherapy. |
Discussion
The 2015 WHO classification of lung tumors significantly alters the LCC category of the 2004 WHO classification. Many LCCs are now reassigned to either adenocarcinoma with solid pattern or non-keratinizing squamous cell carcinoma based on immunopositivity for adenocarcinoma markers or squamous cell carcinoma markers, respectively. NSCLC with negative immunomarkers that cannot be classified as adenocarcinoma with solid pattern (ADC-S) or non-keratinizing squamous cell carcinoma (NKSQCC) are now classified as LCC with null immunohistochemical features (LCC-N), a new WHO-defined category. The study group was reclassified according to WHO 2015 criteria [3-6]. LCCs with ambiguous immunostaining (LCC with unclear immunohistochemical features) or with no immunostaining available (LCC with no staining available) are also distinguished.At our institution, 32 patients comprised 4 cases of LCLC with unclear immunohistochemical features, 16 cases of LCLC with null immunohistochemical features, and 12 cases of LCLC with no staining available. The other LCC subtypes from the 2004 WHO classification are reclassified as follows. Basaloid carcinoma has been moved to a subtype of squamous cell carcinoma. Lymphoepithelioma-like carcinoma has been moved to a group of “other and unclassified carcinomas.” Clear cell carcinoma and rhabdoid phenotype are now regarded as cytological features rather than a specific histologic subtype because these can occur in a variety of histologic types including adenocarcinoma or squamous cell carcinoma. LCNEC is now grouped with the other neuroendocrine tumors [4].
LCLC of the lung is a relatively uncommon and aggressive subset of NSCLC. More than 70% of patients have a history of smoking [7]. Therefore, smoking appears to be the primary cause in LCLC development. The mean age of patients ranges between 61.4 and 65 years [7,8]. Monica et al. found the male to female ratio as 33:9 in their study [8]. In our study, the ratio was 30:2, 93.75% of our patients were male. Twenty-two (68.75%) patients had a history of smoking and none of the female patients were smokers. As recognition and reporting of LCLC increases, the epidemiology of this neoplasm will be better defined, including possible associated environmental and genetic risk factors.
The true incidence of LCLC is low in all probability, although it has not been well defined. The incidence of LCLC through surgically resected patients appears to be between 3% and 9% based on the available literature [9,10]. Liang et al. presented a study of 174 cases of LCLC, which accounted for 5.7% of their total lung cancer cases. In the study, there were 80 cases of classic LCLC, 64 cases of LCNEC, six cases of combined LCNEC, 19 cases of basaloid carcinoma, three cases of clear cell carcinoma, and two cases of lymphoepithelioma-like carcinoma. Their true incidence of classic LCLC was 2.6%, although it was 5.7% with the 2004 WHO classification. With preliminary statistics, 32 patients were diagnosed as having LCLC at our institution between 1999 and 2016, accounting for 1.6% of the total lung cancer cases (1935 cases) during the corresponding time period. Though according to WHO 2015, the incidence of LCLC will decrease because tumors such as basaloid carcinoma, lymphoepithelioma-like carcinoma, clear cell carcinoma, and rhabdoid phenotype carcinomas have been excluded from LCLC classification. Seven cases of lymphoepithelioma-like carcinoma cases, three clear cell variants cases, one rhabdoid variant case, two basaloid carcinoma cases, 27 cases of LCNEC, and 3 cases of combined LCNEC from our institution were excluded because of these new classifications.
Regarding tumor location, LCLCs mostly present as peripheral tumors, although they may be centrally located. In gross examination they frequently appear as large necrotic tumors [7,9,10,12]. In our study, tumors were centrally located in 6 (18.75%) patients, 26 (81.25%) patients had peripheral lesions.
The diagnosis of LCC can only be made on a sampled resected tumor and it is nearly impossible to diagnose LCLC from preoperative biopsies. In preoperative small biopsies, in the setting of a tumor with a negative adenocarcinoma marker (i.e., TTF-1) and only weak or focal staining for a squamous marker, it is best to classify the tumor as ‘NSCLC, not otherwise specified (NOS). In our study, a malignant tumor was confirmed in 5 (15.6%) patients via bronchoscopic biopsy, and in 15 (46.87%) patients using CT-guided transthoracic needle biopsy, and diagnosis of a malignant tumor was achieved by FS examination in 12 (37.5%) patients during the operation.
The treatment of LCLC is comprehensive, primarily with complete tumor resection with systematic nodal dissection [13]. In Liang et al.’s study, the radical resection rate of LCLC was 73.5%, of which the majority underwent a lobectomy and the patients with classic LCLC had a significantly higher one-year survival rate (74.4%). Whether adjuvant chemotherapy is required following surgery remains controversial [7,13]. We performed complete tumor resection with systematic nodal dissection in our 29 patients because of LCLC over the 15 years. In the other 3 patients, one had N2 lymph node metastasis, which was confirmed with mediastinoscopy, and no further surgical resection was applied. The patient gave up curative chemoradiotherapy. One patient who had lobectomy with chest wall resection with positive surgical margins had adjuvant chemoradiotherapy, and the remaining patient had stage IV disease and underwent surgery for diagnostic reasons and prolonged air leakage after transthoracic needle biopsy. Pneumonectomy, bilobectomy inferior, lobectomy and lobectomy with resection of the chest wall was performed for patients with complete tumor resection. There was a recurrence in a patient with pleural invasion, 2 months after surgery on the diaphragm, anterior of the thoracotomy incision, in the posterolateral and retrosternal areas. In spite of chemoradiotherapy, the patient died in the postoperative 3rd month. In one patient who underwent lobectomy and chest wall resection after neoadjuvant chemotherapy, metastasis on the both two adrenal glands, pancreas, liver, anterior wall of the abdomen, abdominal lymph nodes, and intestinal segments was determined and the patient died four months later. However, the other patients had no distant organ metastasis or local recurrences.
The 1, 3, and 5-year survival rates of our study were 65.6%, 53.1%, and 46.9%, respectively. The 5-year survival rates were reported in the literature as between 46.7% and 61.5%, but these studies were based on the 2004 WHO classification. In our current study, we present our survival rates and survival curves for the 2015 WHO classification with a more homogeneous LCLC group (Table 3 and Graph 3). Furthermore, 23 of the 32 patients with advanced-stage LCLC underwent oncologic therapy, two received neoadjuvant chemotherapy, 17 received adjuvant chemotherapy, and 4 had chemoradiotherapy. A total of 3 patients had palliative radiotherapy.
The role of adjuvant therapy for LCLC should be examined in large-center prospective, randomized trials. LCLCs were characterized by extensive local and distant tumor spread, particularly to extrathoracic organs such as the kidneys, adrenal glands, liver, gastrointestinal tract and mesentery, and extremely short survival. Despite surgery and adjuvant chemoradiotherapy, LCLCs are aggressive with a poorer prognosis compared with other pulmonary cancers. Our study showed that if the LCLC is treated with a multimodal approach and metastasis is not observed, survival is promising.
As a conclusion the diagnosis of LCLC is primarily based on the pathologic diagnosis. Several changes have occurred that increase the clinical significance of LCLC histopathologic classification. We compared our findings with the literature published before the 2015 WHO Classification of Tumors of the Lung. Thanks to the 2015 WHO classification, the definite diagnosis rate of LCLC has improved, and developments in epidemiologic, biologic, and therapeutic trials are promising.
Declaration of conflicting interests
The authors declared no conflicts of interest with respect to the authorship and/or publication of this article.
Funding
The authors received no financial support.
Reference
1) Travis WD, Linnoila RI, Tsokos MG, Hitchcock CL, Cutler GB Jr, Nieman L, et al. Neuroendocrine tumors of the lung with proposed criteria for large-cell neuroendocrine carcinoma. An ultrastructural, immunohistochemical, and flow cytometric study of 35 cases. Am J Surg Pathol 1991; 15: 529-53.
2) Brambilla E, Moro D, Veale D, Brichon PY, Stoebner P, Paramelle B, et al. Basal cell (basaloid) carcinoma of the lung: a new morphologic and phenotypic entity with separate prognostic significance. Hum Pathol 1992; 23: 993-1003.
3) Travis WD, Colby TV, Corrin B, Shimosato Y, Brambilla E. WHO histological classification of tumours. Histological typing of lung and pleural tumours, 3rd Edn. Berlin, Springer-Verlag, 1999.
4) Travis WD, Brambilla E, Nicholson AG, Yatabe Y, Austin JHM, Beasley MB, et al. The 2015 World Health Organization classification of lung tumors: Impact of genetic, clinical and radiologic advances since the 2004 classification. J Thorac Oncol 2015; 10: 1243-60.
5) Driver BR, Portier BP, Mody DR, Deavers M, Bernicker EH, Kim MP, et al. Next-generation sequencing of a cohort of pulmonary large cell carcinomas reclassified by World Health Organization 2015 criteria. Arch Pathol Lab Med 2015; doi: 10.5858/arpa.
6) Travis WD, Brambilla E, Muller-Hermelink HK and Harris CC (eds): World Health Organization classification of tumours. Pathology and genetics of tumours of the lung, pleura, thymus and heart. IARC Press, Lyon, 2004.
7) Liang R, Chen TX, Wang ZQ, Jin KW, Zhang LY, Yan QN, et al. A retrospective analysis of the clinicopathological characteristics of large cell carcinoma of the lung. Experimental and Therapeutic Medicine 2015; 9: 197-202.
8) Monica V, Scagliotti GV, Ceppi P, Righi L, Cambieri A, Iacono ML, et al. Differential thymidylate synthase expression in different variants of large-cell carcinoma of the lung. Clin Cancer Res 2009; 15: 7547-52.
9) Travis WD. Pathology of lung cancer. Clin Chest Med 2011; 32: 669-92.
10) Shields TW. Pathology of carcinoma of the lung. Shields TW, editor. General thoracic surgery. 7th ed. Philadelphia: Lippincott Williams & Wilkins; 2009. p. 1311-41.
11) Sun Z, Aubry MC, Deschamps C, Marks RS, Okuno SH, Williams BA, et al. Histologic grade is an independent prognostic factor for survival in non-small cell lung cancer: an analysis of 5018 hospital- and 712 population based cases. J Thorac Cardiovasc Surg 2006; 131: 1014-20.



