2Department of Pathology, University of Health Sciences, Yedikule Chest Diseases and Thoracic Surgery Education and Research Center, Istanbul, Turkey DOI : 10.26663/cts.2020.0006
Summary
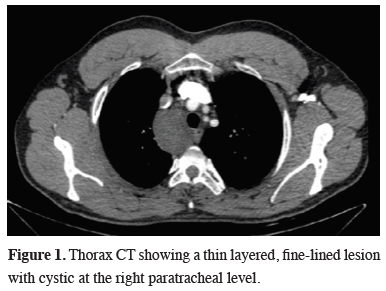
Lymphangiomas are often congenital benign tumors that are formed by abnormal proliferation and development of lymphatic tissues. Although it may be localized in all lymphatic chain regions, intrathoracic localization has been reported rarely. Here we present a case of a 24-year-old non-smoker male patient admitted to our clinic with an incidentally found well-circumscribed radioopacity located in the right upper zone of the mediastinal region detected on routine chest x-ray. The computerized thorax tomography revealed a thin layered, fine-lined lesion with cystic content of 8x6 cm, located at the right paratracheal level. The patient underwent a video-assisted thoracoscopic excision of the cyst, and lymphangioma was confirmed based on the histopathologic examination. Although various alternative treatment methods such as chemotherapy, radiotherapy, sclerosing therapy, and laser therapy are used in the treatment of lymphangioma However, their effects on the treatment vary widely in the reported publications.Introduction
Lymphangiomas are often congenital, benign tumors that are formed by abnormal proliferation and development of lymphatic tissues. Three pathological types defined were; simple, cavernous and cystic forms. Cystic lymphangiomas are surrounded by a fibrous pseudocapsule that are large and commonly multiloculated. Although they might be localized in all lymphatic chain regions, intrathoracic localization has been reported rarely and the superior mediastinum is the site that the lesion resides in the intrathoracic region. It may cause symptoms such as cough, dyspnea, stridor, dysphagia and hemoptysis due to compression of the neighboring structures such as superior vena cava, trachea, ductus thoracic, esophagus, left and right brachiocephalic vein. Thereto patients might present with vena cava superior syndrome, chylothorax, Horner’s syndrome, constrictive pericarditis, and secondary infections. Mostly they are diagnosed at the first two years of age, however, because of their slow growth and deep settlements, they can be detected in adulthood, either incidentally or when became symptomatic [1].We here present an incidentally diagnosed giant cystic lymphangioma, which was located in the right paratracheal area and excised via video-assisted thoracoscopic surgery (VATS).
Case Presentation
A 24-year-old non-smoker male patient admitted to our clinic with an incidentally found well-circumscribed radioopacity located in the right upper zone of the mediastinum during a pre-marital routine chest x-ray examination. Computerized thorax tomography (CT) revealed a thin-layered, fine-lined 8x6 cm cystic lesion located at the right paratracheal level (Figure 1).
 Click Here to Zoom |
Figure 1: Thorax CT showing a thin layered, fine-lined lesion with cystic at the right paratracheal level. |
The physical examination was normal. He described a decrease in his exercise capacity during the last 3 years, without causing a problem to his daily routines. There were no abnormalities in the routine blood tests, EKG and pulmonary function test (FEV1: 4.61 L, %105.8, FVC: 4.62, %89.8)
Surgery was planned with the initial diagnosis of a bronchogenic cyst and considering the deep mediastinal localization, vascular surroundings and the abundance of cystic nature, no preoperative invasive diagnostic procedure was done.
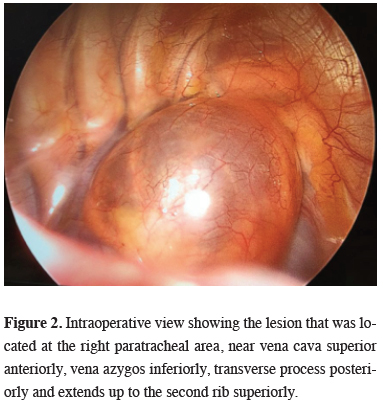
The exploration was done via two-port VATS, under general anesthesia with double-lumen endotracheal tube intubation. An uninoculated cystic mass, which was located in the right paratracheal area, in close relation to vena cava superior anteriorly, vena azygos inferiorly, transverse process posteriorly and extending up to second rib level superiorly was observed (Figure 2). After excision of the mediastinal pleura, the deep extension of the cyst between vena azygos, vena cava superior, and the brachiocephalic vein was seen. The cyst was aspirated which was clear and straw-like colored, to reach the root for complete dissection to prevent injury to vessels. After the root of the lesion was released from the posterior side of superior vena cava, it was separated from the mediastinal fatty tissue by using an endolinear stapler. After inserting one apicobasal chest tube, the operation was terminated without any complication.
 Click Here to Zoom |
Figure 2: Intraoperative view showing the lesion that was located at the right paratracheal area, near vena cava superior anteriorly, vena azygos inferiorly, transverse process posteriorly and extends up to the second rib superiorly. |
The patient was uneventfully discharged on postoperative day 3. In the histopathological examination of the lesion, CD31 and D2-40 antibodies were stained positive which was compatible with cystic lymphangioma (Figure 3).
 Click Here to Zoom |
Figure 3: The lesion stained immunohistochemically with D2-40 (x200). |
Physical examination was normal at three month follow-ups, and CT scan revealed no recurrences at the first-year control.
Discussion
Lymphangiomas often described as congenital malformations that are accused by lymphoid tissue insufficiency, lymphoid-venous junction problems, gemmation abnormalities, and/or sequestration of embryonic lymphoid tissue [2]. These lesions are typically thin-walled and mostly multilocular but may also be unilocular, as in our case. The content may be serous or chylous fluid [2,3]. Although mediastinal cystic lymphangiomas are rare, some cases exist in the literature [4-12]. Cystic lymphangioma was diagnosed in only 5 (1.8%) of 279 patients who underwent excision for the mediastinal cyst [6].Mediastinal cystic lymphangiomas are rarely seen lesions that are typically located in the superior mediastinum and at the right hemithorax. Bronchogenic cysts, thymic cysts or thymomas, coelomic cysts, enteric cysts, and ductus thoracicus cysts should be considered at the differential diagnosis. Most of the lymphangiomas detected in adulthood are asymptomatic. However, patients can be presented with symptoms such as chest pain, cough, dyspnea, stridor, dysphagia due to compression of intrathoracic structures. Hoarseness due to vocal cord paralysis and swelling of the neck due to venous compression may be observed.
The recommended radiological imaging methods for the diagnosis of the cystic lesion are x-ray and thorax CT. In our case, the chest x-ray showed a mediastinal widening and the thorax CT imaging revealed a cystic, well-circumscribed and homogenous soft tissue lesion. Three-dimensional ultrasound imaging is also useful for detecting fine septations compatible with lymphangioma. MRI scanning helps to accurately predict relations between the lymphatic chain and other mediastinal organs [1]. Cystic lymphangiomas characteristically immunohistochemically stained positive with CD31 and D2-40 [13].
The standard treatment modality is complete surgical excision via thoracotomy or VATS, as performed in our case. Surgical resection is necessary both to confirm the diagnosis and to prevent complications that may occur due to the compression effect on vital organs. Surgical removal of the cyst wall should be achieved completely. The success of totally excised cases is quite high. As we have performed, cysts in larger sizes can be completely resected after aspirating its content, to reveal the borders in the full sense and not to injure vascular structures.
Some authors predicted that cystic lesions might be in communication with the ductus thoracicus. Thus, in the preoperative period, the administration of olive oil from a nasogastric catheter was suggested. However, we did not prefer this method in this particular case [2].
Some authors suggest that these cysts can be excised by enucleation. Whichever the method is, it should be kept in mind that, there is a risk of recurrence in incomplete resections. We have not found any sign of recurrence after a one-year follow-up in our patient. Esme et al. reported significantly lower morbidity, mortality, and recurrence rate in patients undergoing surgery for mediastinal cysts, compared to conservative approaches [14]. Nowadays, surgical excision with VATS is used safely for curative treatment of many mediastinal cystic lesions in experienced centers. In the study of Ulaş et al. [15], VATS and conventional thoracotomy methods were compared in the surgical approach to mediastinal cysts, and it was statistically significant that the patients of the VATS group had lower hospitalization length and operation duration. Moreover, VATS patients had no increase in the means of intraoperative bleeding, postoperative complications, and incomplete resection risk. In that vein, we did not encounter any kind of intraoperative or postoperative complications, and the patient was discharged from the hospital three days after surgery with complete recovery. In our center, the first choice for the approach to mediastinal cystic lesions has been excisional intervention with VATS.
In conclusion, the surgical approach is the curative treatment method for mediastinal cystic lymphangioma cases, and nowadays, the VATS procedure should be preferred primarily as it significantly reduces the operation time and postoperative hospital stay.
Declaration of conflicting interests
The authors declared no conflicts of interest with respect to the authorship and/or publication of this article.
Funding
The authors received no financial support.
Reference
1) Faul JL, Berry GJ, Colby T V, Ruoss SJ, Walter MB, Rosen GD, et al. Thoracic lymphangiomas, lymphangiectasis, lymphangiomatosis, and lymphatic dysplasia syndrome. Am J Respir Crit Care Med 2000;161:1037-46.
2) Brown LR, Reiman HM, Rosenow III EC, Glovıczkı PM, Divertıe MB. Intrathoracic lymphangioma. In: Mayo Clinic Proceedings. Elsevier; 1986. p. 882–92.
3) Limmer S, Krokowski M, Kujath P. Pulmonary lymphangioma. Ann Thorac Surg 2008;85:336-9.
4) Murayama S. Retrocrural cystic lymphangioma. Chest 1985;88:930-1.
5) Çangır AK, Kutlay H, Şahin A, Hadi A, Yavuzer Ş. Lenfanjioma Mediastinal ve Mediastinai-Splenik Yerleşimli İki Lenfanjioma Olgusu. Ankara Üniversitesi Tıp Fakültesi Mecmuası 1998;51:43-8.
6) Payne WS, Clagett OT, Wollner LB. Surgical treatment of mediastinal tumors: a 40 year experience. J Thorac Cardiovasc Surg 1971;62:379-92.
7) Blumenthal EZ, Gottehrer NP, Dollberg M, Halevy J. A giant tuberculous lymphangioma extending from the mediastinum to the inguinal region. Chest 1994;105:1279-80.
8) Morgenstern L, Bello JM, Fisher BL, Verham RP. The clinical spectrum of lymphangiomas and lymphangiomatosis of the spleen. Am Surg 1992;58:599-604.
9) Panich V. Splenic cystic lymphangiomatosis: an unusual cause of massive splenomegaly: report of a case. J Med Assoc Thailand1994;77:165-8.
10) Bhatti MAK, Ferrante JW, Gielchinsky I, Norman JC. Pleuropulmonary and skeletal lymphangiomatosis with chylothorax and chylopericardium. Ann Thorac Surg 1985;40:398-401.
11) Johnson DW, Klazynski PT, Gordon WH, Russell DA. Mediastinal lymphangioma and chylothorax: the role of radiotherapy. Ann Thorac Surg 1986;41:325-8.
12) Moore TC, Cobo JC. Massive symptomatic cystic hygroma confined to the thorax in early childhood. J Thorac Cardiovasc Surg 1985;89:459-62.
13) Kitami A, Suzuki T, Usuda R, Masuda M, Suzuki S. Diagnostic and therapeutic thoracoscopy for mediastinal disease. Ann Thorac Cardiovasc Surg 2004;10:14-8.






