2Thoracic Surgery Clinic, Kastamonu State Hospital, Kastamonu, Turkey
3Department of Pathology, University of Health Sciences, İzmir Dr. Suat Seren Chest Diseases and Thoracic Surgery Health Application and Research Center, İzmir, Turkey DOI : 10.26663/cts.2020.0008
Summary
Castleman’s disease is angiofollicular lymph node hyperplasia that occurs as a result of abnormal proliferation of plasma cells and B lymphocytes in lymphoid tissues. It has been shown to be associated with HHV-8 and HIV infections and may be unicentric or multicentric. This case is presented due to its rareness, good prognosis after complete surgery for unicentric type, and dramatically improved symptoms.Introduction
Castleman’s disease is a rare, non-clonal, lymphoproliferative disorder of unknown etiology, first described by Benjamin Castleman in 1954 [1-3]. It is categorized into two clinical subtypes as unicentric (localized) and multicentric [4]. Variable clinical findings may be observed. Thorax is affected in 70% of the cases. It has been shown to be associated with human herpes virus 8 (HHV-8) and human immunodeficiency virus (HIV) infections [4-6]. Unicentric type has been reported to have a good prognosis following complete resection [7]. This case is presented due to the rarity of intrathoracic unicentric Castleman’s disease diagnosed through surgery.Case Presentation
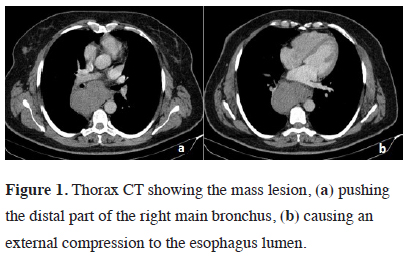
A 46-year-old female patient presented with cough, dyspnea, and dysphagia. Physical examination was normal. Chest x-ray revealed an enlarged mediastinum. Computed tomography of the thorax showed an 8x5x11 cm mass lesion located in the subcarinal area, pushing the distal part of the right main bronchus and trachea forward and causing external compression of the esophagus lumen (Figure 1).
 Click Here to Zoom |
Figure 1: Thorax CT showing the mass lesion, (a) pushing the distal part of the right main bronchus, (b) causing an external compression to the esophagus lumen. |
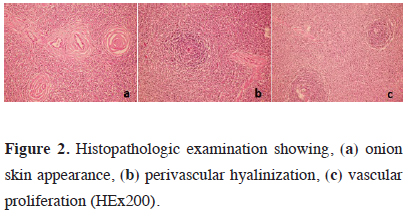
The right posterolateral thoracotomy incision revealed a mass lesion of approximately 14 cm located in the posterior mediastinum extending into the subcarinal area and azygos vein. The lesion was resected with the capsule. Invasion into the surrounding tissues was not observed. Final pathology was reported as Castleman’s disease (Figure 2). All symptoms of the patient, particularly dysphagia, regressed. The patient is still being followed up uneventfully in the 26th month.
 Click Here to Zoom |
Figure 2: Histopathologic examination showing, (a) onion skin appearance, (b) perivascular hyalinization, (c) vascular proliferation (HEx200). |
Discussion
Castleman’s disease, also known as angiofollicular lymph node hyperplasia, is a rare lymphoproliferative disease [8]. It was first described by Benjamin Castleman in a patient with localized mediastinal mass in 1954 [1]. The generalized type of the disease was described by Gaba et. al in 1978 [9]. The disease can arise anywhere lymphoid tissue is present, as well as in the thoracic cavity especially in mediastinum and hilum. It is thought that various infectious agents (EBV, human herpes virus-8), inflammatory reactions (interleukin-6, vascular endothelial growth factor) and hamartomatous development play a role in the etiology [10-12].It has two types as multicentric and unicentric [3,7]. Unicentric type is often asymptomatic, more common in women than in men, and no etiological factor has been identified [4,8,13]. It is seen in the 3rd or 4th decade of life and malignancy potential is low. It is mostly located in mediastinal lymph nodes. It may also be observed in the neck, axilla, retroperitoneal region, mesentery and pelvis [14]. Surgical treatment is curative and the symptoms regress after surgery [15,16]. Five-year survival has been reported to be 100% [2]. Our case was also diagnosed in the fourth decade, being consistent with the literature, and her symptoms improved after surgery. No etiological factor was identified. The lymph node was completely resected with the capsule and there was no invasion outwards.
Multicentric type is more common than unicentric and it is associated with HIV and HHV-8 more frequently [4,8,17]. Fever, night sweats, weakness and massive lymphadenopathy are the most common symptoms [18]. Surgical excision is the best method for diagnosis. However, it is not always possible to excise due to invasion into the surrounding tissue and hypervascularization. Systemic chemotherapy, antiretroviral agents, interferon alpha, immunomodulatory drugs, rituximab and corticosteroids are recommended for treatment [4]. Multicentric type has a worse prognosis than unicentric type [7]. Patients should be followed closely.
In conclusion, Castleman’s disease is a rare lymphoproliferative disease. It is mostly located in the mediastinum. Surgical excision is curative for localized type, dramatically improving the symptoms and the prognosis is excellent.
Declaration of conflicting interests
The authors declared no conflicts of interest with respect to the authorship and/or publication of this article.
Funding
The authors received no financial support.
Reference
1) Castleman B. Case records of the Massachusetts General Hospital Weekly clinicopathological exercises, case 40011. New Eng J Med 1954;9: 26-30.
2) Şengül AT, Süllü Y, Ünsal M, Başoğlu A. Castleman Hastalığı: Nadir interlober yerleşim nedeniyle. Solunum 2012;14:109-12.
3) Çobanoğlu U, Kırgın H, Uğurluer G. Dev Lenf Nodu Hiperplazisi: Castleman Hastalığı (Bir Olgu Nedeniyle). Van Tıp Dergisi 2009;16:78-80.
4) Gündüz E. Nadir Bir Lenfoproliferatif Hastalık: Castleman Hastalığı. Osmangazi Tıp Dergisi 2016;38: 6-16.
5) http://www.uptodate.com/contents/unicentric-castlemans-disease.
6) Oksenhendler E, Boutboul D, Fajgenbaum D, et al. The full spectrum of Castleman disease: 273 patients studied over 20 years. Br J Haematol 2018;180:206.
7) Bowne WB, Lewis JJ, Filippa DA, Niesvizky R, Brooks AD, Burt ME et al. The management of unicentric and multicentric Castleman’s Disease. A report of 16 cases and a review of the literature. Cancer 1999;85:706.
8) Soumerai JD, Sohani AR, Abramson JS. Diagnosis and management of Castleman disease. Cancer Control 2014;21:266-78.
9) Gaba AR, Stein RS, Sweet DL, Variakojis D. Multicentric giantlymph node hyperplasia. Am J Clin Pathol 1978;69:86-90.
10) Soulier J, Grollet L, Oksenhendler E, Cacoub P, Cazals-Hatem D, Babinet P, et al. Kaposi’s sarcoma-associated herpesvirus-like DNA sequences in multicentric Castleman’s disease. Blood 1995;86:1276-80.
11) An J, Sun Y, Sun R, Rettig MB. The Kaposi sarcoma–associated herpesvirus (KSHV) induces cellular interleukin 6 expression: role of the KSHV latency-associated nuclear antigen and the AP1 response element. Blood 2003;99:649-54.
12) Polizzotto MN, Uldrick TS, Wang V, Aleman K, Wyvill KM, Marshall V et al. Human and viral interleukin-6 and other cytokines in Kaposi sarcoma herpesvirus-associated multicentric Castleman disease. Blood 2013;122:4189-98.
13) Talat N, Belgaumkar, AP, Schulte, KM. Surgery in Castleman’s disease: a systematic review of 404 published cases. Ann Surg 2012;255:677-84.
14) Mishra A, ElHousieni EA, Ehtuish EF. Retropharyngeal Castleman’s disease: US, CT and MR imaging findings: Case report and review of literature. Eur J Rad Extra 2008;67:e53–e57.
15) Yeh CM, Chou CM, Wong LC. Castleman’s disease mimicking intrapulmonary malignancy. Ann Thorac Surg 2007; 84: e6–7.
16) Jemi Olak. Benign lymph node disease involving the mediastinum.In: General thoracic surgery. 5.th. ed. Philadelphia:Lippincott Williams and Wilkins; 2000 p. 2254–2255.






