Summary
Thymolipoma is one of the benign pathologies of the mediastinum that may reach large sizes over time and even become a giant mass that fills the hemithorax. It may cause respiratory distress and even failure, and may be accompanied by myasthenia gravis or other clinical conditions. Surgical excision of the mass provides both diagnosis and treatment.Introduction
Thymolipoma is one of the rare benign neoplasms of endodermal and mesodermal origin, which contain mediastinal fat tissue and thymic elements in different proportions. The term thymolipoma was first defined in the literature by Hall in 1949 [1]. Since then, it has also been called lipothymoma, thymic tissue residue mediastinal lipoma, benign thymoma and lipomatous hamartoma.Thymolipoma is generally asymptomatic [2,3]. However, when the thymolipoma reaches a large size, it may cause respiratory distress and even respiratory failure. It may also be associated with clinical conditions such as myasthenia gravis and aplastic anemia [1,4,5]. It is difficult to differentiate small thymolipomas from other anterior mediastinal masses on chest x-ray. Large-sized lesions of thymolipoma may mimic cardiomegaly by erasing the contours of the heart [1].
Thymolipoma has been reported in the literature as single case presentations or small case series. Therefore, we aimed to present this case due to its rarity, discussing the diagnosis and treatment with the help of relevant literature.
Case Presentation
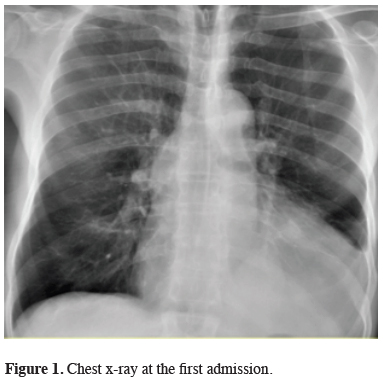
A 52-year-old male patient was admitted to our clinic with bloody sputum and dyspnea. The patient was diagnosed with chronic obstructive pulmonary disease (COPD) three years ago and medical treatment was started. At patient’s first admission to our hospital, he was first evaluated by chest x-ray and Morgagni hernia was considered as a preliminary diagnosis (Figure 1).
 Click Here to Zoom |
Figure 1: Chest x-ray at the first admission. |
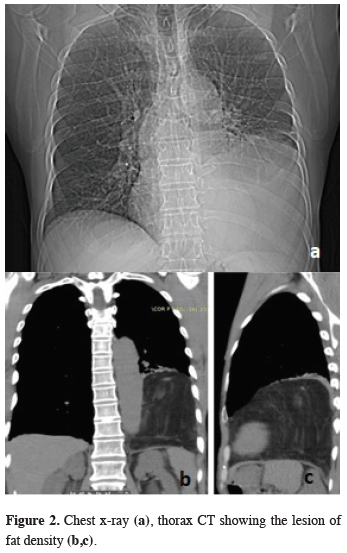
Unfortunately, the patient refused furter examination and treatment. At the second admission nine months later, he had only dyspnea. The patient was reevaluated by chest x-ray and thorax computed tomography (CT) scan. Thorax CT scan revealed a 16x12.5x8.5 cm lesion containing largely fat-density and prominent vascular structures in the middle lower mediastinum (Figure 2).
 Click Here to Zoom |
Figure 2: Chest x-ray (a), thorax CT showing the lesion of fat density (b,c). |
Lipoma was suspected as the radiological preliminary diagnosis. The forced exhalation volume in one second (FEV1) value was 1.90 L (57%) and the FEV1/ forced vital capacity (FVC) was 78%. The differential diagnosis included lipoma and diaphragmatic eventration.
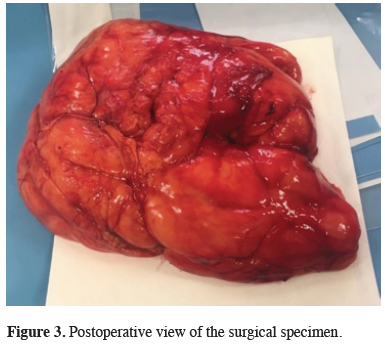
VATS was planned for exploration. The patient was intubated with double-lumen endotracheal tube and placed in the lateral decubitus position. The diaphragm was intact during exploration, and an extrapulmonary lipomatous mass associated with mediastinum was detected on the diaphragm. The operation was converted from video-assisted thoracoscopic surgery (VATS) to open thoracotomy because of the large size of the lesion. The mass was totally excised via left thoracotomy (Figure 3).
 Click Here to Zoom |
Figure 3: Postoperative view of the surgical specimen. |
In the pathological and immunohistochemical examination, macroscopically 22x18x9 cm encapsulated fatty tissue was reported as thymolipoma. No postoperative complications were observed and the patient was discharged uneventfully. Besides, dyspnea symptom resolved completely after surgery. During the asymptomatic 9-month follow-up period, no recurrence was encountered.
Discussion
Thymolipoma is a very rare, slow-growing benign anterior mediastinal neoplasm that accounts for 2-9% of all thymic neoplasms. It is a well-circumscribed, and encapsulated lesion composed of mature adipose tissue containing islands of non-neoplastic thymic tissue. These tumors usually consist of adipose tissue, but also contain a small amount of thymic structure [2]. The amount of thymic tissue is in excess of what would be considered normal for patient’s age. It is difficult to distinguish between lipoma and thymolipoma having fat component excess. High power view of a thymolipoma showing thymic elements within mature adipose tissue. Most consider it to be a benign neoplasm; however, there is some controversy regarding its pathogenesis. In thymolipoma, thymic epithelial elements can be detected by serial sectioning and immunohistochemical staining with cytokeratin [5].Very slowly growing thymolipoma can sometimes reach very large and giant sizes. It can be seen as a mass image that fills a hemithorax and extends to the opposite side [1-5]. The symptoms are usually caused by compression of adjacent intrathoracic organs and structures such as the heart, large vessels, lungs and bronchus. Dyspnea, chest pain, cyanosis, tachypnea are the most common symptoms [3]. Our patient with COPD was admitted to the hospital with complaints of bloody sputum and worsening dyspnea. On his second admission, he presented with increased dyspnea.
Due to body temperature and gravity, the mass of thymolipoma grows into the anterior and inferior mediastinal area. It can mimic diaphragm eventration by erasing diaphragm contours on side radiographs [2,5]. Therefore, diaphragmatic eventration was also considered in our case and the surgery was started via VATS. Detection of adipose tissue on thorax CT may be helpful in diagnosis. Operation planning can be performed with magnetic resonance imaging and digital subtraction angiography. In this way, the feeding arteries and venous return associated with large vessels can be determined before the operation [1]. Lipoma, liposarcoma, mediastinal lipomatosis, and congenital diaphragmatic hernia can be considered as a differential diagnosis [2]. In our case, Morgagni hernia was considered as a preliminary diagnosis in the evaluation by chest x-ray, but this diagnosis was excluded according to the results of advanced radiological examinations and left-sided localization of the lesion. We considered the mass was benign, so positron emission tomography (PET-CT) was not obtained.
Needle biopsy is not appropriate for diagnosis. Radiological methods for diagnosis often give an idea about the lesion, but surgical excision is necessary for both definitive diagnosis and treatment. Total excision is easy because the lesion is encapsulated and does not invade surrounding tissues [5].
Thoracotomy, sternotomy and VATS can be chosen according to the nature of the lesion. VATS can be performed for small lesions. Thoracotomy is preferred for lesions that fill almost all of the hemithorax, even though the mediastinal component is present. Although we started with VATS, conversion to thoracotomy was necessary for safe and complete removal of the lesion. No recurrence is expected after a complete resection of thymolipoma. Long-term follow-up is not necessary for these patients due to the good prognosis.
In conclusion, although rare, thymolipoma should be considered in the differential diagnosis of fat-containing lesions filling the thorax.
Declaration of conflicting interests
The authors declared no conflicts of interest with respect to the authorship and/or publication of this article.
Funding
The authors received no financial support
Reference
1) Sancak T, Özdemir N, Bilgiç S. Giant thymolipoma case. Diagn Interv Radiol 2001;7:366-9.
2) Alban ŞT, Tekin M, Yurttaş M. Asemptomatik dev timolipoma (olgu sunumu). Tuberk Toraks 2000;48:70-2.
3) Çelik A, Aydın E, Karaoğlanoğlu N. Dev mediastinal timolipoma. Eurasian J Pulmonol 2013;15:120-2.






