Summary
Approximately 25% of the patients have an ectopic location of the parathyroid gland. In some cases, hyperfunctional parathyroid glands may extend into the mediastinum that requires mediastinal surgical exploration. A 66 years old woman presented with fatigue and raised serum calcium and parathormone levels. Thorax computed tomography revealed a mediastinal mass and an aberrant right subclavian artery (ARSA) which is the most common vascular anomaly of the aortic arch was demonstrated. The mediastinal mass was evaluated in favor of parathyroid adenoma by parathyroid scintigraphy. Videothoracoscopic resection of the adenoma was performed safely.Introduction
Primary hyperparathyroidism (PHPT) is an endocrine disorder characterized by elevated serum calcium and parathormone levels. Although parathyroid adenoma, which is the most common cause of PHPT, is mostly located in the parathyroid gland, it has an ectopic location in approximately 25% of the cases [1]. Due to the rare possibility of ectopic parathyroid adenoma, diagnosis may be a challenge which delays management. Locating ectopic adenoma is another difficulty for surgery. Therefore, keeping a high index of suspicion of patients with raised serum calcium and parathormone (PTH) levels are the key point for diagnosis.Here, we aimed to present a patient with the coexistence of mediastinal parathyroid adenoma and aberrant right subclavian artery, which is the most common intrathoracic major arterial anomaly.
Case Presentation
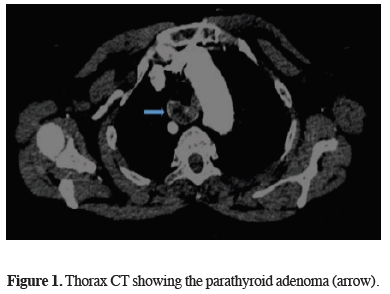
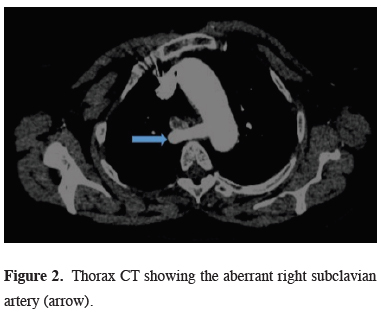
A 66 years old woman was referred to our department with fatigue and raised serum calcium and PTH levels. The patient had no comorbid disease except hypertension. There was no family history of any endocrine disorder. Thorax computed tomography (CT) revealed a heterogeneous density solid mass of 35x20 mm between the anterior of the right aberrant subclavian artery and posterior trachea (Figures 1,2)
 Click Here to Zoom |
Figure 1: Thorax CT showing the parathyroid adenoma (arrow). |
 Click Here to Zoom |
Figure 2: Thorax CT showing the aberrant right subclavian artery (arrow). |
PTH level was 1225 pg/mL , serum calcium level was 11.4 mg/dL, and serum thyroid-stimulating hormone (TSH) value was 6.56 mIU/L. (The normal values for PTH, calcium and TSH is 15-65 pg/mL, 8.5- 10.5 mg/dL and 0.4-4 mIU/L respectively).
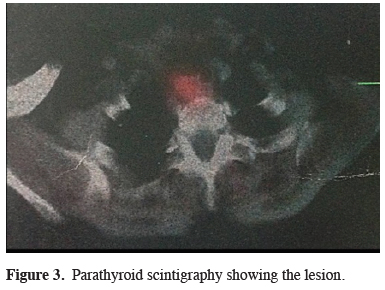
Parathyroid scintigraphy was performed with technetium 99, and the mass was evaluated in favor of parathyroid adenoma (Figure 3).
 Click Here to Zoom |
Figure 3: Parathyroid scintigraphy showing the lesion. |
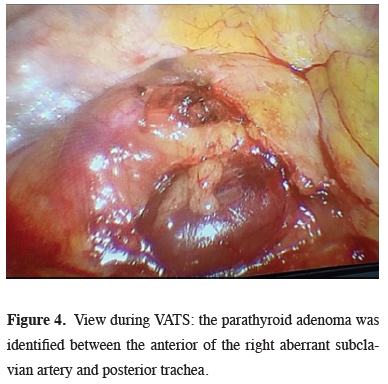
Based on these findings, mediastinal mass excision was performed via right videothoracoscopic approach. A utility port of 3 cm was placed at the fourth intercostal space at the anterior axillary line. One additional 1.5 cm port was then placed at the midaxillary line. After exploring the mediastinum, the parathyroid adenoma was identified between the anterior of the right aberrant subclavian artery and posterior trachea. Using a harmonic scalpel, the parietal pleura was dissected while carefully avoiding the ARSA (Figure 4).
 Click Here to Zoom |
Figure 4: View during VATS: the parathyroid adenoma was identified between the anterior of the right aberrant subclavian artery and posterior trachea. |
The parathyroid adenoma was then dissected free from the surrounding tissue. At the histopathological examination, the lesion with lobular appearance, dirty - yellow color and bleeding, was reported to be compatible with parathyroid adenoma. PTH level was 53.16 pg / mL and serum calcium level was 8.9 mg / dL on the first of postoperative day. The patient was discharged uneventfully at postoperative day 4.
Discussion
The most common cause of PHPT (80-85%), characterized by hypercalcemia and hypophosphatemia, is parathyroid adenoma [1]. It is generally seen in women around the age of 60 years old. As well as it may be asymptomatic, in some patients, osteoporosis, urinary stone, polyuria, vomiting can be seen.It should be kept in mind that hyperparathyroidism may be a component of multiple endocrine neoplasia type 1 (MEN), pituitary tumor, and pancreatic islet tumor [2]. Although it is mostly located in the parathyroid gland, approximately 25% of the patients have an ectopic location [1]. Thymus (38%), retro / paraesophageal space (31%), thyroid (18%), mediastinum (6%), and carotid sheath (3%) are the most common sites of ectopic localization [3]. Ectopic inferior parathyroid glands are usually located in the anterior mediastinum within the thymus, while superior parathyroid glands are located in the posterosuperior mediastinum. Since the size is generally small, it is crucial to use preoperative technetium 99 (99mTc) scintigraphy for the localization.
Aberrant right subclavian artery (ARSA) or Lusoria artery is the most common vascular anomaly of the aortic arch with a rate of 0.5-2.5% [4]. It is a rare anatomical variation in which ARSA originates directly from the distal part of the aortic arch instead of brachiocephalic artery. Although it is mostly localized in the retroesophageal site, it may be located in anterior of the trachea or between the esophagus and trachea. The majority of cases with ARSA are asymptomatic. Retroesophageal form is the most commonly seen form that patients may complain of dysphagia due to compression of the esophagus. Anterior tracheal localization may be the cause of dyspnea. Surgery for ASA is offered in just case of being symptomatic.
99TC-MIBI scintigraphy is not a definite method but has a sensitivity of 80-90% [5]. False positivity may be detected in patients with lung cancer metastasis or patients with mediastinal tumors such as thymoma, seminoma, and lymphoma. False negativity may be seen in patients with multiple adenomas or hyperplasia [6]. Also, thoracic computed tomography (CT) and magnetic resonance imaging are helpful to determine the anatomic localization and the relationship of mediastinal parathyroid adenoma with the other structures.
CT can detect lesions over 1.5 cm in size. Although reviews are reporting that intraoperative gamma probes can be used for small-sized lesions [7], some surgeons suggest that this method will not be beneficial due to large vessels and heart activities [8]. Intravenous methylene blue is another option to localize ectopic glands. In some cases, intraoperative parathyroid hormone assay is used to be sure that the excised mass is a parathyroid adenoma or not.
The definitive treatment of parathyroid adenoma is surgery. Surgical methods such as cervical approach, video-assisted mediastinoscopy, sternotomy, thoracotomy, video thoracoscopy should be chosen according to the location of the mass. The cervical approach is the preferred method for adenomas located at or above the aortic arch level. Thoracotomy, sternotomy, mediastinotomy, or video thoracoscopy (VATS) is more appropriate for lesions located under the aortic arch or deeper in the mediastinum [9]. Parathyroid adenoma excision using video thoracoscopy was first reported in 1994 by Prinz et al. Subsequently, it is reported that VATS is a feasible and safe approach for mediastinal parathyroid adenoma [10]. Since then, video thoracoscopy has been used more widely. VATS offers more advantages over both thoracotomy and sternotomy. It allows better visualization of the tumor and exposure of the mediastinum, excellent access, shorter operative time, shorter tube dwell time, shorter hospital stay and reduced postoperative pain. Also it is superior in the cosmetic way when compared to sternotomy and thoracotomy scars [11]. Complications such as pleural effusion, hematoma, pneumothorax, wound site infection, mediastinitis, and sternal dehiscence are more likely to be seen in conventional methods like sternotomy and thoracotomy.
In conclusion, videothoracoscopic resection of mediastinal masses can be performed safely even in patients with aberrant vascular structure.
Declaration of conflicting interests
The authors declared no conflicts of interest with respect to the authorship and/or publication of this article.
Funding
The authors received no financial support.
Reference
1) Sagan D, Goz´dziuk K. Surgical treatment of mediastinal parathyroid adenoma: rationale for intraoperative parathyroid hormone monitoring. Ann Thorac Surg 2010;89:1750-5.
2) Lassen T, Friis-Hansen L, Rasmussen AK, Knigge U, Feldt-Rasmussen U. Primary hyperparathyroidism in young people. When should we perform genetic testing for multiple endocrine neoplasia 1 (MEN-1) J Clin Endocrinol Metab 2014;99:3983-7.
3) Spear C, Geraci T, Bizekis C, Zervos M. Resection of an ectopic parathyroid adenoma via Video-Assisted Mediastinoscopy. Semin Thorac Cardiovasc Surg 2019;31:323-5.
4) Patel HM., Banerjee S, Bulsara S, Sahu T, Sheorain VK, Grover T et al. A rare entity: traumatic thoracic aortic injury in a patient with aberrant right subclavian artery. Ann Vasc Surg 2017;41: 280.
5) Wei B, Inabnet W, Lee JA, Sonett JR. Optimizing the minimally invasive approach to mediastinal parathyroid adenomas. Ann Thorac Surg 2011;92:1012-17.
6) Hu J, Ngiam KY, Parameswaran R. Mediastinal parathyroid adenomas and their surgical implications. Ann R Coll Surg Engl 2015;97:259-61.
7) Mehrabibahar M, Mousavi Z, Sadeghi R, Layegh P, Nouri M, Asadi M. Feasibility and safety of minimally invasive radioguided parathyroidectomy using very low intraoperative dose of Tc-99m MIBI. Int J Surg 2017;39:229-33.
8) Liu RC, Hill ME, Ryan JA. One-gland exploration for mediastinal parathyroid adenomas: cervical and thoracoscopic approaches. Am J Surg 2005;189: 601-5.
9) Lihara M, Suzuki R, Kawamata A, Horiuchi K, Okamoto T. Thoracoscopic removal of mediastinal parathyroid lesions: selection of surgical approach and pitfalls of preoperative and intraoperative localization. World J Surg 2011;36:1327-34.






