

2Department of Thoracic Surgery, University of Health Sciences, Şişli Hamidiye Etfal Health Application and Research Center, Istanbul, Turkey DOI : 10.26663/cts.2020.00028
Summary
Extramedullary hematopoiesis (EMH) is a condition that usually coexists with hematological disorders and rarely causes mass formation. It can occur anywhere in the body, but very rarely becomes a tumorlike mass in the posterior mediastinum and paravertebral region. A 41-year-old female patient presented with respiratory distress. Radiologically, multiple large mass lesions were detected in the posterior mediastinum, localized bilaterally at paravertebral regions. Diagnostic studies with transthoracic biopsy specimen were showed that the mass lesion was consisting of myelocytes, lymphocytes, erythrocytes and megakaryocytes, so the case was reported as EMH. The case was presented to make a differential diagnosis, because it mimics solid neoplasms at unusual localizations, and may accompany hematological disorders.Introduction
Extramedullary hematopoiesis (EMH) is the body’s compensatory response by the bone marrow to erythropoiesis deficiency, or accelerated destruction of erythrocytes, and refers to a deposit of erythroid precursors in other sites more than the bone marrow and peripheral blood. Although it is seen mostly microscopically deposited in various tissues rarely manifests as hepatosplenomegaly or lymphadenopathy [1,2]. It is usually diagnosed incidentally and, presents rarely as a posterior mediastinal mass, mimicking any kind of a mediastinal tumor. Intrathoracic EMH is a rare pathology and only very few case reports have been described in patients with chronic myeloproliferative disorders, especially myelofibrosis with myeloid metaplasia, anemia, thalassemia-sickle-cell anemia, MYH9-related thrombocytopenia, polycythemia and spherocytic anemias [1-9]. The patients with EMH, are most commonly asymptomatic or have symptoms related to anemia such as fatigue and dizziness. Rarely, they occur as a solid mass and the patients have mass related symptoms [10,11]. The posterior mediastinum is an uncommon localization for EMH, except some sporadically reported intrathoracic manifestations. In radiological screening with computed tomography (CT) and/or Magnetic Resonance Imaging (MRI), it is usually identified as bilateral, multiple, and well-circumscribed mass with soft tissue density [12,13].The case was reported to avoid misdiagnosis and unnecessary surgery, due to the unusual location of EMH, by mimicking solid neoplasm in the posterior mediastinum as an unusual location. Besides, it was reported to raise awareness of hematological neoplasms that manifest themselves with anemia and form mass lesions.
Case Presentation
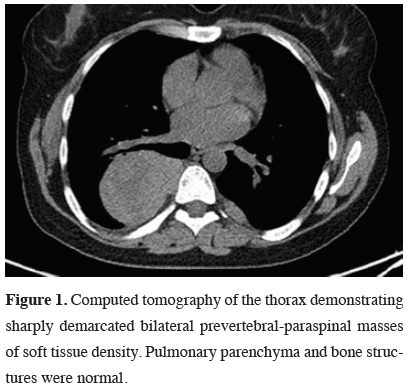
A 41-year-old woman admitted to the hospital with dyspnea. Her physical examination was normal and the laboratory studies revealed mild anemia (Hgb: 9.4 g/dL, RBC: 3.37 x 1012/L, CT: 33.2 %, MCV: 98.5 fL). Abdominal ultrasonography and CT revealed the spleen enlargement with a size of 14 mm in largest axis and 149x91x143 mm respectively. In positron emission tomography (PET)- CT, hematopoietic system activation was detected in spleen and bone marrow. Thorax CT showed a 109x95x64 mm mass lesion lying posteriorly between 6 to 10th thoracic vertebrae at the right side. A second paravertebrally localized lesion was on the left side, sized as 61x47x29 mm, at the level of thoracic 8-10th vertebrae, and a third 24x13x9 mm sized mass lesion at the level of the left costovertebral junction, close to the thoracic 7-8th vertebrae, adjacent to pleura. Mediastinal lymphadenopathies were detected at right paratracheal and left prevascular regions with 11 mm of the largest (Figure 1).
 Click Here to Zoom |
Figure 1: Computed tomography of the thorax demonstrating sharply demarcated bilateral prevertebral-paraspinal masses of soft tissue density. Pulmonary parenchyma and bone structures were normal. |
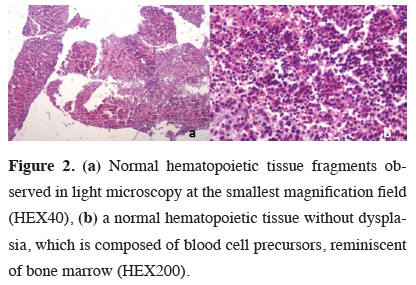
A tru-cut biopsy was performed from the mass that was located in the posterior mediastinum. Microscopically, the composition of cells were lymphocytes, erythrocytes, plasma cells, megakaryocytes and histiocytes (Figures 2a and b) where the structure showed similarity to bone marrow.
 Click Here to Zoom |
Figure 2: (a) Normal hematopoietic tissue fragments observed in light microscopy at the smallest magnification field (HEX40), (b) a normal hematopoietic tissue without dysplasia, which is composed of blood cell precursors, reminiscent of bone marrow (HEX200). |
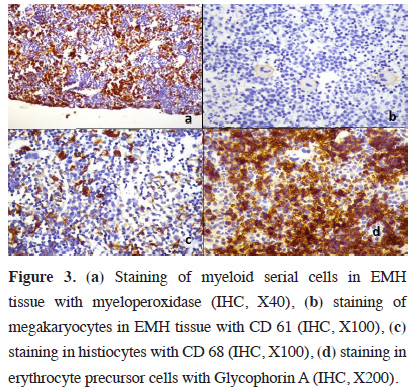
Immunohistochemical stains showed that some lymphocytes were focally stained with CD3, the other lymphocytes were stained with CD20. Megakaryocytes were positive with CD61 (Figure 3a), myelocytes were positive with MPO (Figure 3b). Erythrocyte precursor cells were found to be positive with GLCO A (Figure 3c) and monocytes were positive with CD68 (Figure 3d).
 Click Here to Zoom |
Figure 3: (a) Staining of myeloid serial cells in EMH tissue with myeloperoxidase (IHC, X40), (b) staining of megakaryocytes in EMH tissue with CD 61 (IHC, X100), (c) staining in histiocytes with CD 68 (IHC, X100), (d) staining in erythrocyte precursor cells with Glycophorin A (IHC, X200). |
The cells showed negative immunoreactivity with pancytokeratin, CD34 and CD117. In light of the whole clinical and histological features, this case was diagnosed as extramedullary hematopoiesis. With the final diagnosis, the patient referred to hematology clinic and blood transfusions with symptomatic management were applied. In her 10-months follow up period the whole process was uneventful.
Written informed consent was obtained from the patient for publication of her data.
Discussion
The source of normal hematopoiesis is bone marrow. In particular, the lower skull, vertebrae, shoulder and pelvic girdles, ribs and bone marrow located in the sternum have this function. The hematopoietic active bone marrow continues to its function until late adolescence. EMH is considered as a compensatory mechanism that occurs secondary to inadequate bone marrow function [2]. The exact pathogenesis of EMH is unclear, transforming of embryonal rests of osteogenic tissue may be accused. Besides, it may originate from the extension of hyperplastic bone marrow through the ribs and vertebral bodies. Some lesions are silent and waiting to be discovered by chance. Rare ones have signs of compressing neighboring organs [11,14,15]. EMH may rarely occur in unexpected places and as a lesion mimicking a tumor, forming a mass. For this reason, it is often misdiagnosed [2,8]. As in our case, the posterior mediastinum is among these rare places [2].The causes of EMH may be pathological or physiological. There are wide varieties of pathologic conditions in which disturbance of the normal blood-forming marrow may be associated with the formation of extramedullary hematopoietic tissue. Common causes of EMH include spherocytic anemia, erythroblastosis of newborn, thalassemia, pernicious anemia in the period of relapse, macrocytic anemia of hepatic origin, carcinomas with bone marrow invasion, Hodgkin’s disease, lymphoma, leukemia, osteosclerosis and myeloproliferative syndrome [1-8].
The mechanism of origin of these extramedullary foci is unknown, but there are several theories like embolization, direct extension, myelostimulation or redirected differentiation, which explain the pathogenesis of EMH, but none of them is widely acceptable [15]. EMH is a physiologic compensatory mechanism that is usually associated with hematologic disorders as in our case and most of the other reported cases. EMH cases without hematological disorder have also been described [10].
Symptoms related to mass formation seen in EMH cases are related to the location of the lesion [2,10]. Patients may sometimes be asymptomatic [2,11]. Although the masses those are locating in the posterior mediastinum usually cause no symptoms, the ones with large dimensions might cause respiratory problems related to compression and neurologic deficits related to the level of involvement. The patients have complaints due to spontaneous pneumothorax, hemithorax and rapidly fatal respiratory failure [10,11,15]. Our case also had severe respiratory distress. Also, anemia was found in the patient who had complaints of weakness and fatigue.
It was determined that the case, which was immediately biopsied with the concern of the possibility of advanced neoplastic lesions, was a case of EMH secondary to anemia, forming a solid mass. A population of cells resembling bone marrow was observed in routine preparations obtained from the biopsy. Mesenchymal originated mediastinal neoplasms, especially lymphomas, were also included in the differential diagnosis. However, those were excluded by the presence of precursor cells, same as in the bone marrow, which constitutes blood cells examined in light microscopy. Possible lymphoreticular tissue neoplasms were also excluded from the differential diagnosis due to the absence of features such as atypia, pleomorphism, and disorganization, and determination of cell origin by additional immunohistochemical examinations.
Treatment of EMH diagnosed solid masses, can be variable depending on the patient and the disease. These methods are the use of blood transfusion, radiotherapy, surgical decompression, hydroxyurea and JAK2 inhibitors. JAK2 inhibitors and TGF-β ligand traps that improve the erythropoiesis process are being tested in patients with thalassemia and EMH who do not respond to treatment, and the results look promising. In the absence of severe symptoms and complications, EMH treatment may not be required [2]. Our patient whose symptoms started to regress with blood transfusion treatment is followed up by the clinic.
In conclusion, EMH is a rare pathology, but can be serious with mortal complications and also can be confused clinically and radiologically with other benign or malignant lesions in the posterior mediastinum. It should be kept in mind in the differential diagnosis of resistant anemia cases with radiologically determined mass. Clinician-radiologist-pathologist collaboration is required to avoid misdiagnosis.
Declaration of conflicting interests
The authors declared no conflicts of interest with respect to the authorship and/or publication of this article.
Funding
The authors received no financial support.
Reference
1) Yao WQ, Wang WY, Liu XJ, Gao LM, Wang Z, Xiang CX et al. Mediastinal myelolipoma/extramedullary hematopoiesis presenting as a mass: rare differential diagnosis among mediastinal tumors. Int J Clin Exp Pathol 2018;11:2714-20.
2) AAL-Yaseen H, Marashi M, Al Olama AS, Seliem R. Pancytopenia with Mediastinal Mass: Clinically Challenging at Times. Dubai Med J 2019;2:31-5.
3) An J, Weng Y, He J, Li Y, Huang S, Cai S et al. Intrathoracic extramedullary hematopoiesis presenting as tumor-simulating lesions of the mediastinum in α-thalassemia: A case report. Oncol Lett 2015;10:1993-6.
4) Santini M, Fiorelli A, Vicidomini G, Napolitano F. Intrathoracic extramedullary haematopoiesis manifested as a neoplastic lesion within anterior mediastinum. Ann Thorac Surg 2009;88:2001-4.
5) Bolaman Z, Polatli M, Cildag O, Kadiköylü G, Culhaci N. Intrathoracic extramedullary hematopoiesis resembling posterior mediastinal tumor. Am J Med 2002;112:739-41.
6) Baikoussis NG, Beis JP, Verra C, Siminelakis SN. A mass in the posterior mediastinum; extramedullary haemopoietic tissue. Eur Rev Med Pharmacol Sci 2012;16:691-4.
7) Oermann EK, Coppa ND, Margolis M, Sandhu FA. Extramedullary hematopoietic tumor mimicking a thoracic nerve root schwannoma. J Neurosurg Spine 2010;13:78-81.
8) Kombak FE, Bozkurt SU, Özgümüş T, Atagündüz IK. Mass-forming extramedullary hematopoiesis mimicking Hodgkin’s lymphoma. Marmara Medical Journal 2019;32: 55-7.
9) Zaninetti C, Boveri E, Melazzini F. Massive mediastinal enlargement due to extramedullary haematopoiesis in a patient with MYH9-related thrombocytopenia. Br J Haematol 2017;178:10.
10) Kubokura H, Koizumi K, Yoshino N, Yamagishi S, Mikami I, Hirata T et al. A Case Report: Thoracic Extramedullary Hematopoiesis Found by Occuring Spontaneous Pneumothorax. Ann Thorac Cardiovasc Surg 2008;14:382-5.
11) Takhar R, Bunkar M, Jangid V, Saxena A. Extramedullary hematopoiesis presenting as an asymptomatic posterior mediastinal mass: An unusual presentation. Lung India 2016;33:569-70.
12) Nakazono T, Yamaguchi K, Egashira R, Takase Y, Nojiri J, Mizuguchi M et al. CT-based mediastinal compartment classifications and differential diagnosis of mediastinal tumors. Jpn J Radiol 2019;37:117-34.
13) Marchiori E, Barreto MM, Hochhegger B, Zanetti G. Extramedullary Haematopoiesis: An Uncommon Posterior Mediastinal Mass. S Afr J Rad 2013;17:114-5.



