Summary
Background: Abramson technique is a worldwide technique used for minimally invasive treatment of pectus carinatum. We have performed this surgery since 2012. This article presents our experience about Abramson surgery.Materials and Methods: Between June 2012 and December 2019 64 patients with pectus carinatum underwent minimally invasive surgery.
Results: Mean age of the patients were 14.4 years (range 8-25 years). 47 were male, 17 were female. All patients referred to our clinic with cosmetic complaints. 14 (21.8%) patients also had clinical symptoms in preoperative period. Mean duration of operation was 61 minutes. Mean blood loss was 30 ml and death wasn’t seen in any patient. Complication was seen in 15 (10.7%) patients in postoperative period. Splitting of cables was seen in 7 (10.9%) patients as the most common complication in the long term follow-up. Duration of hospitalization ranged from 3 to 15 days (average 5.1 ± 2.9 days). Reoperation was performed in 17 (26.5%) patients.
Conclusions: Minimally invasive surgery is successful for the treatment of pectus carinatum.
Introduction
Pectus carinatum (PC) is the second most common morphological disorder of the chest wall [1]. PC is generally noticed in childhood, but becomes more severe during puberty. There are two types of PC. The chondrogladiolar type presents with protrusion of the gladiolus and inferior costal cartilages along the most prominent area of the sternum; kinetic, orthotic and surgical treatments are available [2]. The first surgical technique was reported by Mark Ravitch in 1952. However, this technique involves both resection of cartilaginous rib regions and sternal osteotomy. Postoperative scarring is extensive, despite the basic aim of aesthetic improvement [2]. Nuss developed minimally invasive surgery for patients with pectus excavatum. The widespread acceptance of this technique encouraged minimally invasive repair of PC, initially introduced by Abramson in 2005 [3,4]. In this approach, the chest wall is not opened. A metal bar of defined composition is used to depress the sternum to an appropriate position, in accordance with the Nuss method. Importantly, this approach is effective [4].Here, we describe the clinical features and outcomes of 64 patients treated with the Abramson technique from 2012 to 2019.
Methods
Sixty-four patients (47 male patients, 17 female patients; mean age, 14.4 years [range, 8-25 years]) underwent Abramson surgery in our Thoracic Surgery Clinic between June 2012 and December 2019. Their data were retrospectively analysed in this study. Written informed consent was obtained from all adult patients and the parents of young patients. Our institutional ethics committee approved the study (No: 19/2020).All patients were referred to our clinic because of cosmetic complaints. Fourteen (21.8%) patients exhibited preoperative clinical symptoms: 11 (17.1%) had chest pain and three (4.6%) had dyspnea on exertion. Six (9.2%) patients had comorbidities. Three had asthma, two had atrial septal defects, and one had scoliosis (Table 1).
Table 1: Clinical data of the pectus carinatum patients before surgery.
All patients exhibited chondrogladiolar deformities, which were symmetric in 20 patients and asymmetric in 44. Sternal compression tests were performed and sternal flexibility was checked while patients stood with their backs to a wall.
Patients were hospitalized 1 day preoperatively; a complete blood count, a chest X-ray, and routine biochemical tests were performed before surgery. All patients underwent computed tomography, as well as preoperative cardiac and pulmonary tests.
Surgical technique
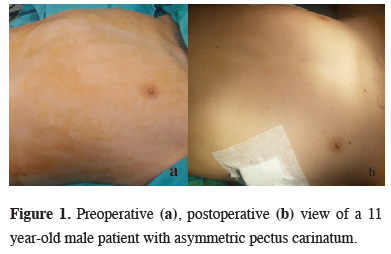
The chest was measured preoperatively and appropriately sized bars were chosen. Surgery was performed with all patients under general anesthesia. All operations were performed by the same surgical team. The bars reached both midaxillary lines and were compatible with the chest wall. Three-centimeter-long incisions were created on both sides of the chest wall in the midaxillary line, at the level of the highest sternal protrusion evident in the supine position. A Kelly clamp (an introducer) was used to enter the chest wall. The introducer was inserted horizontally over the sternum to reach the contralateral side of the chest wall. A submuscular tunnel was created in the region over the highest sternal protrusion. One bar and two stabilizers were placed in accordance with the method described by Abramson. The bars were made of surgical steel, they were 13 mm wide and 2 mm thick (Hipokrat, Izmir, Turkey). The bars extended from the right side of the chest wall, with the concavities facing anteriorly. They were confined to the tunnel formed in the submuscular area. As the tip of a bar emerged from the presternal tunnel, it was directed to the left side of the chest wall. Two adjacent ribs lying under the midaxillary line incision were rotated through 90° and sternal cables were then placed (Pioneer Surgical, Marquette, MI, USA). The cables were passed through the holes of the stabilizers. The bars were thus bilaterally applied to the chest wall as shown in Figure 1 and 2 [5-6]. We didn’t bend the pectus bar after putting it through stabilizers while performing Nuss procedure, because in some cases we encountered with bending of the bar in the medial aspect during bar removal.
 Click Here to Zoom |
Figure 1: Preoperative (a), postoperative (b) view of a 11 year-old male patient with asymmetric pectus carinatum. |
 Click Here to Zoom |
Figure 2: Preoperative posteroanterior (a), right lateral (b), left lateral (c), postoperative (d) view of a 14 year-old male patient with asymmetric pectus carinatum. |
Results
Bar length ranged from 11 to 40.6 cm and stabilizers were placed on both bar ends. The mean operation duration was 61 minutes. The mean blood loss was 30 mL. A chest radiograph was obtained for each patient in the early postoperative period. Systemic analgesia and antibiotics were prescribed.All patients achieved their desired aesthetic outcomes. The duration of hospitalization ranged from 3 to 15 days (mean: 5.1 ± 2.9 days). Patients were advised to return to normal activities in 2-3 weeks.
Complications developed in 15 (10.7%) patients (Table 2). Early complications included pneumothorax (n = 3), wound infection (n = 2), and hematoma (n = 1). Cable splitting was the most common long-term complication; it developed in seven (10.9%) patients. Other long-term complications included allergy-induced bar exposure (n = 3), bar dislocation (n = 3), and costal fracture (n = 1). Recurrences developed in two (3.1%) patients. Re-operations were required in 17 (26.5%) patients (Table 3); split cables were repaired in seven (10.9%) patients, while dislocated bars were replaced in three (4.6%). Bars were replaced in two (3.1%) patients with recurrent disorder. The bar was removed because of dyspnea in one (1.5%) patient; the bar was replaced with a short bar in one (1.5%) patient because of severe pain. The Nuss operation was performed during bar extraction in two patients who exhibited overcorrection. There were no mortalities.
Table 2: Clinical data of surgery and complications.
Table 3: Clinical data of reoperations.
The mean follow-up time was 34.2 months after the first operation. The last Abramson operation was performed in December 2019. Bars were removed from 93.7% of patients. The mean follow-up time after removal was 37.4 months in 60 patients, with one bar per patient. All results were satisfactory after bar removal.
Discussion
PC is a deformity caused by abnormal growth of cartilaginous rib regions. Chondrogladiolar type patients exhibit protruding upper sternum. Chondromanubrial type type patients exhibit protrusion of the entire sternum. Ravitch developed the classical surgical technique in 1952 and it was used worldwide for decades [7]. Sternal osteotomy and resection of costal cartilages is performed in some patients, while other patients require sternal and subperichondrial resection, or sternal osteotomy and subperichondrial resection of deformed cartilage. However, the classical surgical technique is very invasive and painful, scarring is extensive and aesthetic issues occur. Surgery is lengthy, as is postoperative hospitalization. The recurrence rates are higher than those of patients treated using the Abramson technique. Notably, the Abramson technique is less invasive and incisions are small. Sternal osteotomy and resection are not required [5]. The chondromanubrial type chest wall is overly rigid to allow bar placement and open surgery is indicated. However, chondrogladiolar type PC can be treated using the Abramson technique. Abramson et al. reported that, it is preferable to operate during puberty. However, the procedure can be performed at any age. In the present study, we did not consider age when treating our patients. The youngest patient was 8 years of age, while the oldest was 25 years of age. We performed a preoperative sternum compression test. Each patient stood with their back to a wall and received manual compression of the sternum. If this compression temporarily corrected the deformity, surgery was scheduled [4].All patients exhibited chondrogladiolar type deformities. Those with chondromanubrial type deformities were excluded as their chest wall rigidity did not allow presternal bar insertion. Patients with asymmetry were treated by application of compressive pressure to the sternum and this transferred the protruding chondrosternal junctions to the vertebrae [8]. The chest wall must be flexible if this minimally invasive technique is used i.e. patient age is important. Yuksel et al. reported that, 12-18 years of age was optimal because the chest wall is more flexible in puberty. In our present study, 10 patients were 18-25 years of age. The sternum compression test and surgical results were successful in these patients [4].
Non-surgical methods are also available. Bracing is the most common, non-surgical, external compression method. Surgical methods may be preferred if braces do not provide conformity. Lee et al. reported that pain, discomfort, and distress led to poor conformity [9]. We surgically treated patients who were not indicated for bracing and for whom bracing was unsuccessful.
The most common, early postoperative complications were pneumothorax and allergy-induced bar exposure. All instances of pneumothorax resolved spontaneously and there was no need for tube thoracostomy. Yuksel et al. and Ozkaya et al. also reported that pneumothorax was the most common, early postoperative complication [8,10,11]. Abramson et al. reported bar allergies in 2% and 4% of patients in two different series [11]. Implant removal was not required for those patients, as they responded to medical treatment. Yuksel et al. reported bar allergy in five of 172 patients [8]. In this study the bar allergy rate was 4.6% and surgical revision was performed for these patients.
Abramson et al. and Yuksel et al. attached stabilizers to the tips of the bars and placed screws within holes in the tips. These bars were then bilaterally secured using four cables [11-12]. Here, we used bar and stabilizer system, as well as four sternal cables, to supply the rigidity of the chest wall. Lee et al. reported that the cables split in all of their patients [9]. In our study, the cables split in seven (10.9%) patients, which constituted the most common, late follow-up complication; we repaired the split cables. Yuksel et al. reported cable breakdown in six of 172 patients [8]. Because the re-operation rate was high, we preferred to avoid excessive cable tightening during surgery.
Our hypothesis is that, ratio of cable breakdown can be decreased with refrainment from tightening the cables so much during surgery. Furthermore, a preoperative skin test for bar allergy should be routine, to reduce the need for re-operations caused by bar allergy. In the 2005 study by Abramson et al. (40 patients), the most common complication was adherence of skin to the bar in the first eight patients because of subcutaneous placement. Subpectoral bar placement eliminated this complication [2].
We prefer to maintain the bar on the chest wall for 3 years. An early bar removal may increase the possibility of recurrence. Yuksel et al. also preferred to maintain the bar in place for at least 2 years [11]. In our study, bars were removed from 15 patients after a mean duration of 23.5 ± 6.4 months (range, 19-27 months). Ozkaya et al. reported bar removal from 44 of 101 patients after a median of 24.8 ± 4.5 months [10].We removed bars early from nine adults because of poor bar compliance caused by chest wall rigidity. Sliding bars were removed early from four patients. Furthermore, pectus excavatum developed in two patients from whom bars were removed early.
The limitations of this study included its single-centre design and lack of a control group.
In conclusion, the Abramson technique is a rapid and simple treatment of chondromanubrial type PC. The incisions are small, surgery is brief, blood loss is minimal, hospitalization time is short, and pain is minimal. The technique should be preferred to open surgery, because of minimal complications and better cosmetic results.
Declaration of conflicting interests
The authors declared no conflicts of interest with respect to the authorship and/or publication of this article.
Funding
The authors received no financial support for the research and/or authorship of this article.
Ethics approval
The study was approved by the Ethics Committee of Health Sciences University (No: 19/2020).
Authors’ contributions
TA, MA; Conceived and designed the analysis, collected the data, contributed data and analysis tools, performed the analysis, co-wrote the paper.
Reference
1) Suh J, Joo S, Lee GD, Haam SJ, Lee S. Minimally Invasive Repair of Pectus Carinatum in Patients Unsuited to Bracing Therapy. Korean J Thorac Cardiovasc Surg 2016; 49: 92-8.
2) Özkaya M, Bilgin M. Minimally invasive repair of pectus carinatum by modification of the Abramson technique. Wideochirurgia Tec M 2018; 13: 383-7.
3) Kálmán A. Initial results with minimally invasive repair of pectus carinatum. J Thorac Cardiovasc Surg 2009; 138: 434-8.
4) Bilgin M, Oral A. Early results of minimal invasive surgery in patients with pectus carinatum. Turk Gogus Kalp Dama 2012; 20: 307-11.
5) Abramson H, D’Agostino J, Wuscovi S. A 5-year experience with a minimally invasive technique for pectus carinatum repair. J Pediatr Surg 2009; 44: 118-23.
6) Yuksel M, Bostanci K, Evman S. Minimally invasive repair of pectus carinatum using a newly designed bar and stabilizer: a single-institution experience. Eur J Cardiothorac Surg 2011; 40: 339-42.
7) Katrancioglu Ö, Akkas Y, Karadayi S, Sahin E, Kaptanoğlu M. Is the Abramson technique effective in pectus carinatum repair? Asian J Surg 2018; 41: 73-6.
8) Yuksel M, Lacin T, Ermerak NO, Sirzai EY, Sayan B. Minimally Invasive Repair of Pectus Carinatum. Ann Thorac Surg 2018; 105: 915-23.
9) Lee SY, Song IH, Lee SJ. Minimal invasive extrathoracic presternal compression using a metal bar for correction of pectus carinatum. Pediatr Surg Int 2014; 30: 25-30.
10) Özkaya M, Bilgin M. Minimally invasive repair of pectus carinatum: a retrospective analysis based on a single surgeon’s 10 years of experience. Gen Thorac Cardiovasc Surg 2018; 66: 653-7.






