2Department of Thoracic Surgery, Fatih Sultan Mehmet Education and Research Hospital, University of Health Sciences, Istanbul, Turkey
3Department of Emergency Medicine, Göztepe Education and Research Hospital, Medeniyet University, Istanbul, Turkey DOI : 10.26663/cts.2017.0011
Summary
Background: Spontaneous pneumomediastinum is a rare and usually benign finding in young male patient without a history. When subcutaneous emphysema occurs, the patient and medical physicians feel uneasy about the view of face and neck. We review our clinical experience with spontaneous pneumomediastinum in this study.Materials and Methods: We performed a retrospective analysis of demographic features, complaints, precipitating factors and length of hospital stay of patients with spontaneous pneumomediastinum.
Results: Fourteen patients with spontaneous mediastinum were identified, included 10 males. Mean age was 25.4 ± 8.9. Chest pain was the most common complaint. All patients underwent chest-x ray and thoracic computed tomography. Only one esophagogram was done. The patients were discharged uneventfully between 3 and 6 days (mean 3.5 ± 1.25). A 12-month follow-up revealed no recurrence of pneumomediastinum in any of the patients.
Conclusions: Spontaneous pneumomediastinum is a benign entity and generally treated with conservative management. Chest-x ray and thoracic computed tomography are useful tools for diagnosis of the pneumomediastinum. Additional investigation procedures should be performed selectively.
Introduction
Spontaneous pneumomediastinum (SPM) is described as the presence of free air in the mediastinum without any identifiable diseases or precipitating factor such as invasive procedure, mechanical ventilation and trauma [1]. The origin of air is not clear. The first case series of spontaneous pneumomediastinum was published by Louis Hamman in 1939 [2].Subcutaneous emphysema in neck and face is the most alarming symptoms and finding in the emergency department. SPM is a benign and generally self-limiting condition but when subcutaneous emphysema is excessive, it is life-threatened. In the etiology of spontaneous pneumomediastinum, there is no trauma, surgery, iatrogenic injuries or organ perforation. SPM is uncommon, primarily affecting healthy young men due to excessive physical exercise due to the increase of intra-abdominal pressure. Diagnosis is frequently made through physical examination, chest roentgenogram and tomography. Usually SPM does not require extensive workup [3].
The aim of this study was to discuss our clinical experience in the diagnosis and management of SPM and discuss the optimal management strategy.
Methods
In our hospital"s electronic database, we retrospectively analyzed patients in who were diagnosed as spontaneous pneumomediastinum between January 2012 and December 2014. All of the patients who were treated in our clinic provided informed consent by signing a statement allowing the use of their data for clinical trials.We recorded the age, sex, and primary symptom when they admitted to the emergency department, also drug abuse or underlying disease was investigated. The initial chest-x ray, computed chest tomography, performed bronchoscopy and/or endoscopy, length of hospital stay, complications, and treatment were studied.
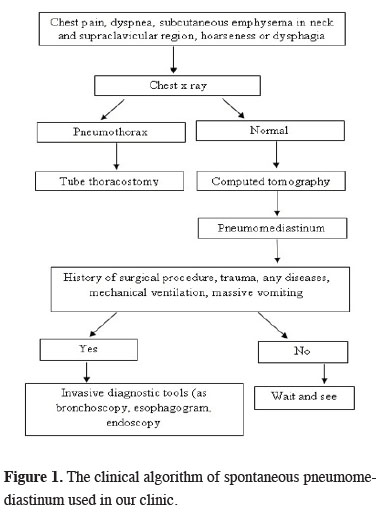
The clinical treatment protocol of SPM was "wait and see" for spontaneous pneumomediastinum in our department. Patients check was done by daily physical examination and chest x-ray. If the patient was stabile clinically and with no extra symptoms, we did not perform any invasive methods (Figure 1). We continued to the conservative treatment until the regression of subcutaneous emphysema achieved.
 Click Here to Zoom |
Figure 1: The clinical algorithm of spontaneous pneumomediastinum used in our clinic. |
Patients had administered O2 (5 Lt/minute) via a nasal cannula continuously. Oral nutrition was stopped for few hours in all patients. Prophylactic antibiotic treatment (cefazolin sodium, 1gr twice per day) was given for acute mediastinitis. The paracetamol was used as analgesia if they chest pain.
Continuous data are summarized by mean ± SD and categorical data by frequencies and percentage.
Results
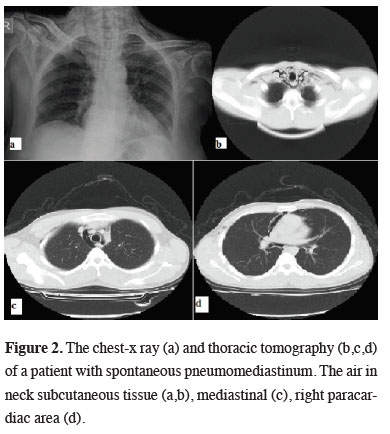
Among 14 patients included in this study, 10 patients (71.4%) were men and four were woman. The ages were between 16 and 48 years (mean 25.4 ± 8.9). First clinical symptoms and signs were chest pain (n= 10, 71%), dyspnea (n= 7, 50%), subcutaneous emphysema in neck (n= 4, 28.5%), hoarseness (n= 3, 21%) and dysphagia (n=1, 7%). Eleven patients had smoking history (78.5%) and two of them had drug abuse (marihuana). The predisposing disease such as asthma, respiratory tract infection, foreign body aspiration was not present. In nine cases symptoms started suddenly, in two after heavy lifting and in two after intensive coughing. When patients arrived at hospital, all of them had subcutaneous emphysema in neck and chest wall. There was no severe respiratory distress leading to an indication for endotracheal intubation.In the emergency department, physical examination"s findings and blood pressure, heart rate, electrocardiogram, blood oxygen saturation and gas values were normal. Routine biochemistry and count blood cells were normal at all cases. Radiological evaluation was done with chest-x ray, computerized thorax tomography. The pathology as pneumothorax, mass, bleb or bulla on lungs was not seen on patients radiologically except mediastinal air and subcutaneous emphysema on chest wall (Figure 2).
 Click Here to Zoom |
Figure 2: The chest-x ray (a) and thoracic tomography (b,c,d) of a patient with spontaneous pneumomediastinum. The air in neck subcutaneous tissue (a,b), mediastinal (c), right paracardiac area (d). |
Fiber optic bronchoscopy and/or endoscopy were performed to selected patients. Only one esophagogram was done. All of 14 patients were discharged uneventfully between 3 and 6 days (mean 3.5 ± 1.25). No morbidity or complication of treatment was seen during hospital stay. A 12-month follow-up revealed no recurrence of pneumomediastinum in any of the patients.
Discussion
Spontaneous pneumomediastinum is a rare entity usually caused by alveolar rupture and air tracking along the tracheo-bronchial tree. There are case reports in the literature, so that there is no consensus on investigation parameters and for treatment of SPM [4,5]. Pneumomediastinum is frequently over-evaluated because of the clinical suspicion of an esophageal or tracheal injury. Spontaneous pneumomediastinum has known to be associated with forceful exercise or situations reproducing the Valsalva maneuver, asthma, respiratory infections, severe cough and vomiting, childbirth, smoking and inhalation of drugs, such as marijuana and cocaine [4]. SPM is mostly seen in young, thin male patients. Patients usually present with subcutaneous emphysema, chest pain, dyspnea, tachypnea, cough, neck pain, and Hamman"s crunch [6-8]. The most common symptom was reported as chest pain similar as our study.Many mechanisms have been suggested to explain the pathogenesis of pneumomediastinum, as (1) gas-producing microorganisms present in an infection of the mediastinum, (2) rupture of the cutaneous or mucosal barriers perforation of the esophagus or tracheo-bronchial tree, allowing air to enter the mediastinum, (3) the existence of a decreasing pressure gradient between the alveoli and the lung interstitium that can result in alveolar rupture, (3) a sudden increase in intrathoracic pressure results in an increased intra-alveolar pressure, leading to alveolar rupture and (5) after thoracic surgery, the air can be seen in mediastinum [1,4,9]. The third and fourth mechanism is known as spontaneous pneumomediastinum. The mechanism of marijuana and cocaine-induced pneumomediastinum is hypothesized to be secondary to barotraumas, resulting from inhalation techniques from severe cough triggered by the drug or the direct toxic effect of drug-causing vasoconstriction and lung damage. In our series, one of the patients was using marijuana.
Chest-x ray, thorax computed tomography, esophagography are radiological imaging tools to detect air in the mediastinum. Endoscopy and bronchoscopy may be needed to rule out esophageal and trachea-bronchial perforation. Usually invasive diagnostic studies are not required. Fiber optic bronchoscopy and/or endoscopy were not used in this series. The esophagogram was performed on one patient and there was not pathological finding on esophagus. The key point of diagnosis is to detailed the medical history of each patient to decide further investigations. The invasive studies should be performed depending on findings of each individual case.
There is no specifically treatment of SPM either on adults or children [10-13]. After diagnostic studies, hospitalization is necessary, oxygen support, bed rest, pain control and/or antibiotic administration is essential. In our study, the range of hospital stay was 3 to 6 days similar to the literature [4,7,8]. Other studies have shown that in the majority of cases, patients with spontaneous pneumomediastinum require only a short inpatient or simple out-patient observation [13-15].
As a conclusion the prognosis of SPM is excellent with conservative management and the risk for recurrence is low. Additional investigation such as esophagography, bronchoscopy or endoscopy should be performed on selected patient.
Declaration of conflicting interests
The author declared no conflicts of interest with respect to the authorship and/or publication of this article.
Funding
The author received no financial support.
Reference
1) Macia I, Moya J, Ramos R, Morera R, Escobar I, Saumench J, et al. Spontaneous pneumomediastinum: 41 cases. Eur J Cardiothorac Surg 2007; 31: 1110-4.
2) Kelly S, Hughes S, Nixon S, Brown SP. Spontaneous pneumomediastinum (Hamman"s syndrome). Surgeon 2010; 8: 63-6.
3) AbolnikI, LossosI S, Breuer R. Spontaneous pneumomediastinum: A report of 25 cases. Chest 1991; 100: 93-5.
4) Banki F, Estrera AL, Harrison RG, Miller CC, Leake SS, Mitchell KG, et al. Pneumomediastinum: etiology and a guide to diagnosis and treatment. Am J Surg 2013; 206: 1001-6.
5) Akdemir HU, Türköz B, Katı C, Duran L, Kayhan S, Çalışkan F. Spontaneous pneumomediastinum: coexistence of shortness of breath and hoarseness. J Clin Anal Med 2013; 4(suppl 3): 229-31.
6) Campillo-Soto A, Coll-Salinas A, Soria-Aledo V, Blanco-Barrio A, Flores-Pastor B, Candel-Arenas M, et al. Spontaneous pneumomediastinum: descriptive study of our experience with 36 cases. Arch Bronconeumol 2005; 41: 528-31.
7) Macia I, Moya J, Ramos R, Morera R, Escobar I, Saumench J, et al. Spontaneous pneumomediastinum: 41 cases. Eur J Cardiothorac Surg 2007; 31: 1110-4.
8) Al-Mufarrej F, Badar J, Gharagozloo F, Tempesta B, Strother E, Margolis M. Spontaneous pneumomediastinum: diagnostic and therapeutic interventions. J Cardiothorac Surg 2008; 3: 59-62.
9) Chen C, Tseng CM, Hsu JH, Wu JR, Dai ZK. Spontaneous pneumomediastinum in adolescent and children. Kaohsiung J Med Sci 2010; 26: 84-8.
10) Abbas PI, Akinkuotu AC, Peterson ML, Mazziotti MV. Spontaneous pneumomediastinum in the pediatric patient. Am J Surg 2015; 210: 1031-5.
11) Fitzwater JW, Silva NN, Knight CG, Malvezzi L, Ramos-Irizarry C, Burnweit CA. Management of spontaneous pneumomediastinum in children. J Ped Surg 2015; 50: 983-6.
12) Takada K, Matsumoto S, Hiramatsu T, Kojima E, Shizu M, Okachi S, et al. Spontaneous pneumomediastinum: an algorithm for diagnosis and management. Ther Adv Respir Dis 2009; 3: 301-7.
13) Freixinet J, Garcia F, Rodriguez PM, Santana NB, Quintero CO, Hussein M. Spontaneous pneumomediastinum long-term follow-up. Respir Med 2005; 99: 1160-3.






