2Department of Thoracic Surgery, Kartal Dr. Lutfi Kirdar Hospital, Istanbul, Turkey
3Clinics of Thoracic Surgery, Liv Hospital, Istanbul, Turkey DOI : 10.26663/cts.2024.013
Summary
Background: Re-do surgery may be necessary for recurrent primary lung carcinoma or a different indication. However, some difficulties such as adhesions may be encountered during re-do surgeries. We hypothesized that people with hypertrophic incision scars have severe adhesions during intuitive surgery. Therefore, this study aimed to share our experience with postoperative incision scars and the amount of pleural adhesions.Materials and Methods: Patients who underwent reoperation (with thoracoscopy and / or thoracotomy) and who had a previous operation on the same side were retrospectively evaluated. The indications of the first and second operations, degree of adhesions, need to perform thoracotomy, and keloid and scar formations of the first incision were analyzed.
Results: A total of 22 patients (mean age, 60.1 ± 9.8; range, 19-83 years) who underwent reoperation on the same side were evaluated; 18 of them underwent reoperation due to the recurrence of the first tumor. Hypertrophic scars were observed at the incision site in six (one of them was with keloid formation), advanced pleural adhesions were found in five, and thoracotomy was required in three patients due to severe adhesions. Severe pleural adhesions were observed in 7 of 16 patients without hypertrophic scar.
Conclusions: Postoperative adhesion is a major cause of difficulties and complications during repeat surgeries. More severe pleural adhesions were observed in patients who had hypertrophic scar formation in the previous incision scar, and this observation influenced the clinical approaches.
Introduction
Locoregional recurrence in patients who underwent nonsmall cell lung cancer resection has been reported in the literature with varying ranges of rates [1]. Although the treatment for locoregional recurrence is described as chemotherapy or radiotherapy in most publications, re-resection is the preferred and most beneficial treatment option in many patients, especially those with good health and without distant metastasis [2,3]. Iterative surgery is a treatment option in second primary lung cancers [2]. Campione et al argued that the second operation is a good alternative in both patients (with recurrences or second primary tumors) if the lesions are solitary and intrapulmonary localized and if patients have good cardiac and respiratory reserves [4]. As in other surgical branches, reoperations in thoracic surgery are more difficult than the first operation especially in patients with adhesions [5]. However, postoperative adhesion formation does not occur at the same level in all patients with similar surgical procedures. While planning any operation, surgeons should consider the specific and potentially problematic features of the case and take necessary precautions. For this reason, surgeons usually wonder about the extent of adhesions before reoperations. Predictive clues that can be detected during preoperative evaluation are an interesting subject. Keloid and hypertrophic scars are described as increased fibroblast density and reactivity post-injury. Therefore, this extraordinary healing could also be seen in the thoracic cavity postoperatively. Similarly, Salim et al defined a correlation between abdominal scar and intra-abdominal adhesion in patients undergoing repeated cesarean section [6].This study aimed to evaluate whether the previous surgical incision scar has predictive value for postoperative adhesion in the thorax.
Methods
Patients who underwent reoperation (with thoracoscopic and/or thoracotomy) and who had a previous operation on the same side were retrospectively reviewed. The indications of the first and second operations, the procedure used at the first operation, the degree of adhesions, and the need to perform thoracotomy due to adhesions were noted. Then, keloid and scar formations during the first incision were recorded. This study was approved by the Kartal Lufu Kirdar Training Hospital Institutional Review Board.Between January 2017 and October 2022, a total of 22 patients (14 males, 8 females; mean age 60.1 ± 9.8 years; range, 19 to 83 years) who underwent reoperation on the same side were evaluated.
Results
While four of them were previously operated on for different reasons, 18 of them underwent reoperation due to the recurrence of the first tumor. Six patients had hypertrophic scars at the incision site (one with keloid formation), five had advanced pleural adhesions, and three had to undergo thoracotomy due to severe adhesions. Seven of 16 patients without hypertrophic scar had severe pleural adhesions (Table 1).Table 1. Patient demographics and clinical characteristics.
We report our experience with two patients with different indications and features.
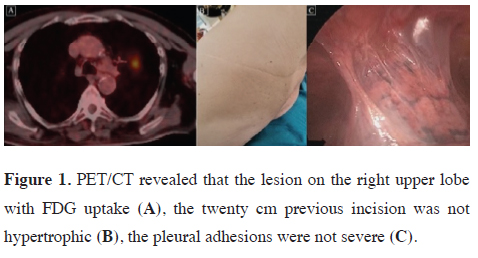
Case 1: A 78-year-old man presented with symptoms of chronic obstructive pulmonary disease (COPD). A 4.6 cm nodule at the left upper lobe was detected with thoracic computed tomography (CT) during the evaluation due to COPD. The 18F-fluorodeoxyglucose (FDG) uptake was 5.3 at positron emission computed tomography (PET-CT) (Figure 1A). The patient had a history of renal cell carcinoma and nephrectomy in 2014. He also had thoracotomy and pleurectomy due to pneumothorax and prolonged air leak on the left side 20 years ago. The incision of the previous thoracotomy was about 20 cm, but the scar was mild without hypertrophy keloid formation on the scar tissue even after the thoracotomy (Figure 1B). Fiberoptic bronchoscopy failed to reveal a final diagnosis. However, we planned to perform a resection (lobectomy) due to suspicion of malignancy. In this patient, we prefer to start the operation with thoracoscopy and then switch to thoracotomy if adhesions associated with the previous operation are severe. Although adhesions are expected to be severe after pleurectomy surgery, adhesions were mild in this patient. The operation could be completed thoracoscopically because of the absence of additional difficulties related to adhesions and previous surgery (Figure 1C). A left upper lobectomy was performed due to tumor localization. Because the lesion was reported as malignant with a frozen section, mediastinal lymph node dissection was added. Postoperatively, no complications occurred, and he was hospitalized for 5 days.
 Click Here to Zoom |
Figure 1: PET/CT revealed that the lesion on the right upper lobe with FDG uptake (A), the twenty cm previous incision was not hypertrophic (B), the pleural adhesions were not severe (C). |
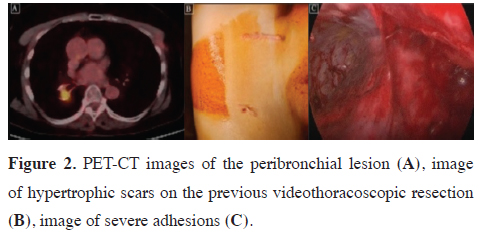
Case 2: A 65-year-old woman was admitted to our clinic from the oncology department because a soft tissue density was detected during follow-up. This right lower lobe peribronchial lesion had a high SUVmax and no suspicion of metastasis in other areas (Figure 2A). The patient had a history of right lower lobe superior segmentectomy for adenocarcinoma by video thoracoscopy 2 years ago. Therefore, the high FDG uptake area was considered as a local recurrence of the first carcinoma. Completion lobectomy was suggested due to no distant metastasis, and her respiratory parameters were good. A severe hypertrophic scar on the previous operation incision was observed during the physical examination (Figure 2B). The operation was started with previous incisions. The Harmonic scalpel (Ethicon Endo-Surgery, Inc., USA) was used for dissection and coagulation of adhesions. Because of severe adhesions, hilar dissection could be started approximately 2h after the initial incision (Figure 2C). The operation was completed with two incisions in a uniportal fashion but took 3h postoperatively, she had an air leak for 2 days and was discharged on postoperative day 4.
 Click Here to Zoom |
Figure 2: PET-CT images of the peribronchial lesion (A), image of hypertrophic scars on the previous videothoracoscopic resection (B), image of severe adhesions (C). |
Discussion
Ucvet et al confirmed that patients who underwent resection for lung cancer have a risk of iterative operation due to local recurrence and developed new lung cancer [7]. Postoperative adhesions are a major cause of difficulties and complications during repeat surgery. Severe adhesions may manifest several years after the initial surgical procedure [8]. The balance between fibrin deposition and degradation is important during normal healing or adhesion formation. These postoperative adhesions are the result of irritation due to infection or surgical trauma and can be considered a pathologic part of healing, especially following any surgical injury [9].Systemic factors (including the female hormone estrogen, hypertension, and hypercytokinemic diseases) were shown to greatly worsen hypertrophic scars and keloid parameters in Ogawa’s meta-analysis [10]. Histologically, localized inflammation has an important role in the formation of hypertrophic skin scars and keloids. Due to inflammation, hypertrophic scars contain inflammatory cells, increased numbers of fibroblasts, newly formed blood vessels, and collagen deposits. Proinflammatory factors, such as interleukin (IL)-1α, IL-1β, IL-6, and tumor necrosis factor-α are upregulated in hypertrophic tissues. Although many agents can be used to prevent postoperative adhesions, most of them are avoided due to side effects. However, corticosteroids and nonsteroidal anti-inflammatory drugs are often used during the postoperative period [11].
Although the relationship between hypertrophic scars and keloids and postoperative abdominal adhesions and their overlapping pathways have not been fully elucidated, Tulandi et al reported that patients with keloids at the wound site had more abdominal adhesions between the uterus and bladder and between the uterus and abdominal wall in repeated cesarean sections [12].
More severe pleural adhesions were observed in patients who had hypertrophic scar formation in the previous incision scar. This observation slightly influenced our clinical approach. Repeat operations were preferred to start with thoracoscopy, and if a problem occurred due to adhesions, then we switched to thoracotomy.
If hypertrophic scar formation is observed at the site of the previous incision in the physical examination of patients, preparations were increased for thoracotomy and the patient was informed about the higher possibility of open surgery. Although surgeries were started with minimal procedures on our patients with or without hypertrophic scar tissue, the conversion rate in open surgery was 2/6 in our patients with hypertrophic scar tissue, whereas this rate was 1/16 in those without hypertrophic scar tissue.
Our study is limited due to the low number of patients and being a retrospective evaluation. Another limitation is that keloids are more prone to occur in some races. However, our study population is not suitable for analyzing the effects of race on adhesions due to geographical reasons.
In conclusion, minimally invasive treatment should be started in patients with previous hypertrophic scar tissue. More caution should be taken in these patients in terms of informing the patients and their relatives preoperatively and preparations for the operating room and surgery. We believe that a prospective multicentric study should strengthen our hypothesis. Another factor that should be considered in a future prospective study is to classify the degree of scar formation and the amount of adhesions based on objective criteria.
Declaration of conflicting interests
The authors declared no conflicts of interest with respect
to the authorship and/or publication of this article.
Funding
The authors received no financial support for the research
and/or authorship of this article.
Ethics approval
This study was approved by the Kartal Lufu Kirdar
Training Hospital Institutional Review Board (May 27,
2024, No: 2024/010.99/4/7).
Authors’ contribution
CT; collected, analyzed and interpreted the patient data,
CT,TC; conceptualized and designed the study, TC;
wrote the paper, collected the literature data, TD; revised
the final version of the manuscript, and co-wrote the paper.
All authors read and approved the final manuscript.
Reference
1) Yano T, Hara N, IchinosenY, Asoh H, Yokoyama H, Ohta M et
al. Local recurrence after complete resection for non-smaIl-cell
carcinoma of the lung. J Thorac Cardiovasc Surg 1994; 107: 8-12.
2) Voltolini L, Paladini P, Luzzi L, Ghiribelli C, Bisceglie MD,
Gotti G. Iterative surgical resections for local recurrent and second
primary bronchogenic carcinoma Eur J Cardiothorac Surg
2000; 18: 529-34.
3) Pikin O, Vasuikevich A, Alexandrov O, Toneev E. Bronchial
stump re-resection for lung cancer recurrence after left pneumonectomy.
Indian J Thorac Cardiovasc Surg 2021; 37: 105-7.
4) Campione A, Ligabue T, Luzzi L, Ghiribelli C, Paladini P,
Voltolini L et al. Late outcome and perioperative complications
for surgery of locally recurrent bronchogenic carcinoma. J Cardiovasc
Surg 2005; 46: 515-8.
5) van Goor H. Consequences and complications of peritoneal adhesions.
Colorectal Dis 2007; 2: 25-34.
6) Salim R, Kadan Y, Nachum Z, Edelstein S, Shalev E. Abdominal
scar characteristics as a predictor of intra-abdominal adhesions
at repeat cesarean delivery. Fertil Steril 2008; 90: 2324-7.
7) Ucvet A, Yazgan S, Samancilar O, Gursoy S, Erbaycu AE,
Komurcuoglu B. Iterative surgical resections in non-small cell
lung cancer. Kardiochir Torakochirurgia Pol 2021; 18: 221-6.
8) Arung W, Meurisse M, Detry O. Pathophysiology and prevention
of postoperative peritoneal adhesions. World J Gastroenterol
2011; 17: 4545-53.
9) Risberg B. Adhesions: preventive strategies. Eur J Surg Suppl
1997; 577: 32-9.
10) Ogawa R. The Most Current Algorithms for the Treatment and
Prevention of Hypertrophic Scars and Keloids: A 2020 Update
of the Algorithms Published 10 Years Ago. Plast Reconstr Surg
2022; 149 79-94.






