

Summary
Pulmonary hypoplasia is a bronchopulmonary foregut anomaly characterized by complete or partial aplasia and hypoplasia /or of pulmonary parenchyma, bronchus, and vessels. "Pulmonary hypoplasia" is typically detected in newborns and infants, while it is rare in adults. In this paper, we present a case of pulmonary hypoplasia in a 47-year-old female patient who had hemoptysis and refractory pulmonary infection.Introduction
Pulmonary hypoplasia (PH) is a rare congenital anomaly caused by incomplete development of lung tissue, leading to a decrease in the number of airways and alveoli. This impairment results in respiratory insufficiency and/or various complications [1]. Initially classified by Schneider into three types in 1912 and later modified by Boyden in 1955. PH is rare in adults and patients described in the literature were newborns and infants [2,3]. The types of hypoplasia and their characteristics are outlined in table 1 [4].Table 1.Types of hypoplasia and characteristics in pulmonary hypoplasia [4].
This case presents a patient diagnosed with bilateral pulmonary lower lobe hypoplasia during surgery, who subsequently underwent bilateral lower lobectomy.
Case Presentation
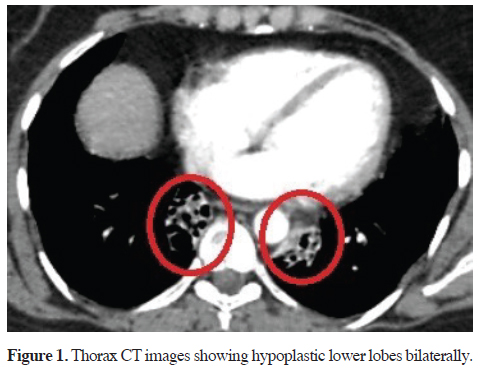
A 47-year-old female patient presented to our clinic with complaints of productive cough, dyspnea, and hemoptysis, along with a history of recurrent pulmonary infections since childhood. The patient reported a history of continuous antibiotic use due to frequent pulmonary infections. Thorax CT revealed atelectasis in bilateral lower lobes, attributed to chronic cystic bronchiectasis (Figure 1). Surgery was scheduled for the patient with a preliminary diagnosis of bilateral bronchiectasis/sequestration.
 Click Here to Zoom |
Figure 1: Thorax CT images showing hypoplastic lower lobes bilaterally. |
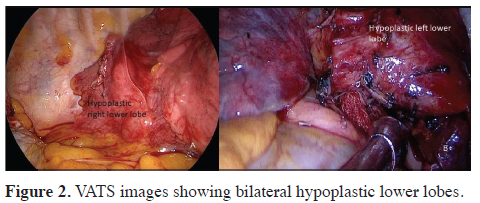
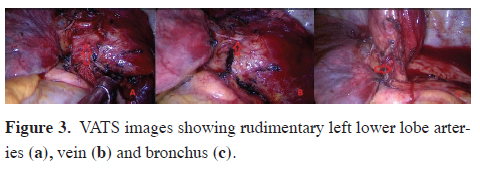
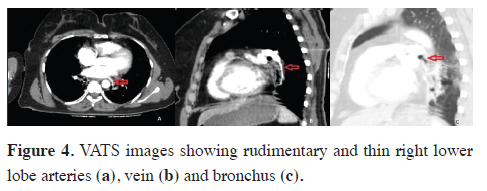
During exploration (first left, then right lower lobectomy via uniportal VATS, with one month between the two surgeries), both bilateral lower lobes were found to be completely rudimentary (Figure 2). The left lower lobe vein and bronchus were hypoplastic. The left lower lobe common basal segment artery was thin, and the superior segment artery was not visible (Figure 3). The right lower lobe vein was also hypoplastic, and the common basal and superior pulmonary artery branches were not visible. The right lower lobe bronchus was extremely narrow and rudimentary, similar to the left lower lobe bronchus (Figure 4).
 Click Here to Zoom |
Figure 2: VATS images showing bilateral hypoplastic lower lobes. |
 Click Here to Zoom |
Figure 3: VATS images showing rudimentary left lower lobe arteries (a), vein (b) and bronchus (c). |
 Click Here to Zoom |
Figure 4: VATS images showing rudimentary and thin right lower lobe arteries (a), vein (b) and bronchus (c). |
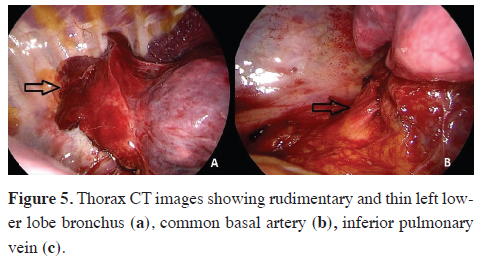
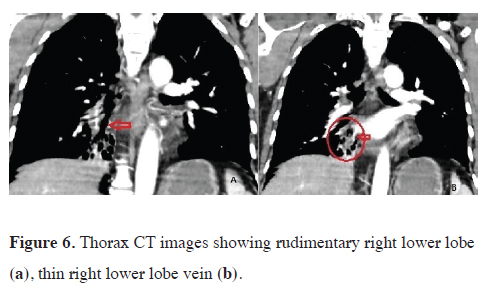
Postoperatively, detailed evaluation of pulmonary CT angiography revealed rudimentary continuation of the lower lobe branches of the venous, arterial, and bronchial systems toward the rudimentary lower lobes (Figures 5,6). The patient was discharged at day 3 uneventfully. Written informed consent was obtained from the patient for the publication of her data.
 Click Here to Zoom |
Figure 5: Thorax CT images showing rudimentary and thin left lower lobe bronchus (a), common basal artery (b), inferior pulmonary vein (c). |
 Click Here to Zoom |
Figure 6: Thorax CT images showing rudimentary right lower lobe (a), thin right lower lobe vein (b). |
Discussion
Disruptions in lung development during the intrauterine period can result in clinically significant lung hypoplasia, which may manifest as unilateral, bilateral, or total/ lobar hypoplasia. Severe respiratory distress typically occurs immediately after birth, although less severe forms, such as lobar hypoplasia, may remain undiagnosed until adulthood [5]. Hypoplasia is often diagnosed during investigations into the cause of recurrent lung infections or incidentally through chest CT scans taken for other reasons [6].Congenital anomalies affecting other systems, such as cardiovascular, gastrointestinal, and genitourinary anomalies, may accompany pulmonary hypoplasia, leading to childhood diagnoses. In the absence of accompanying anomalies, patients may remain asymptomatic [7,8]. Diagnosis is usually incidental on chest radiographs, with the left side more commonly affected in adults. Complications like pneumothorax, pulmonary arterial hypertension, hemoptysis, or recurrent infections with bronchiectasis affecting the hypoplastic lung may necessitate hospital admission [9-11].
Radiological imaging typically reveals volume loss in the affected lobe or lung, mediastinal shift towards the hypoplastic side, volume increase in the contralateral lung or adjacent lobes, and elevation of the adjacent diaphragm [11,12]. CT scans are particularly effective for evaluating the diameter of tracheobronchial and major vascular structures, as well as extensive lung tissue damage, including damage to alveolar and bronchial structures. Hypoplastic bronchi can also be visualized on bronchoscopy [3].
Treatment in adults often involves conservative approaches such as managing infections, symptomatic relief with bronchodilators or expectorants, and prophylactic vaccination if necessary. However, in some patients, recurrent infections and cystic degeneration of the airways may necessitate surgical intervention, particularly if complications such as hemoptysis develop [5]. Minimally invasive surgical methods are preferred, with thoracotomy reserved for cases where thoracoscopic exposure is not feasible due to excessive adhesions [13]. In this patient, recurrent pulmonary infections and recent onset hemoptysis were the primary indications for surgical treatment, and bilateral thoracoscopic lower lobectomy was performed.
In conclusion, pulmonary hypoplasia is rare in adults and typically presents with recurrent lower respiratory tract infections and associated complications. Anatomical surgical resection is recommended using minimally invasive methods and/or thoracotomy
Declaration of conflicting interests
The authors declared no conflicts of interest with respect
to the authorship and/or publication of this article.
Funding
The authors received no financial support.
Authors’ contributions
MGP,VI,YB: conceived and designed the current case
report, co-wrote the paper, collected the clinical data.
The authors discussed the case under the literature data
together and constituted the final manuscript.
Reference
1) Tisekar OR, Hypoplastic Lung Disease. 2023 Jul 24. In: Stat-
Pearls [Internet]. Treasure Island (FL): StatPearls Publishing;
2024. PMID: 32965810.
2) Schneider P. Die Missbildungen der Atmungsorgane. In:
Schwalbe E, Editor.Die Morphologie der Missbildungen des
Menschen und der Tiere, vo1. 3: Die Einzelmissbildungen,
Abt. 2: Missbildungen der einzelnen Organe und Organsysteme.
Jena: Gustav Fischer; 1912. pp.763-857.
3) Boyden EA. Segmental anatomy of the lungs. New York, NY:
McGraw-Hill, 1955.
4) Chassagnon G, Morel B, Carpentier E, Ducou Le Pointe H,
Sirinelli D. Tracheobronchial Branching Abnormalities: Lobebased
Classification Scheme. Radiographics 2016; 36: 358-73.
5) Papadopoulos D, Misthos P, Chorti M, Skopas V, Nakou A,
Karagianidis N et al. Unilateral pulmonary hypoplasia in an
adult patient. Monaldi Arch Chest Dis 2018; 88: 829.
6) Cherian SV, Kumar A, Ocazionez D, Estrada-Y-Martin RM,
Restrepo CS. Developmental lung anomalies in adults: A pictorial
review. Respir Med 2019; 155: 86-96.
7) Dos Santos VM. Unilateral pulmonary hypoplasia. Respir Med
2019; 160: 105818.
8) Katsenos S, Antonogiannaki EM, Tsintiris K. Unilateral primary
lung hypoplasia diagnosed in adulthood, Respir. Care 2014;
59: e47–50.
9) Kumar P, Tansir G, Sasmal G, Dixit J, Sahoo R. Left pulmonary
agenesis with right lung bronchiectasis in an adult, J. Clin. Diagn.
Res 2018; 10: Od15-od7.
10) Sherer DM, Davis JM, Woods JR Jr. Pulmonary hypoplasia: a
review. Obstet Gynecol Surv 1990; 45: 792-803.
11) Thacker PG, Rao AG, Hill JG, Lee EY. Congenital lung anomalies
in children and adults: current concepts and imaging findings.
Radiol Clin N. Am.2014: 52: 155-81.



