2Department of Radiology, Kocaeli City Hospital, Kocaeli, Turkey DOI : 10.26663/cts.2024.018
Introduction
Solitary fibrous tumor (SFT) is a rare neoplasm of mesenchymal origin. Its incidence is equal in men and women, and it most often occurs between the ages of 50 and 80 [1]. SFTs constitute less than 5% of thoracic pleural tumors [2] and commonly occur in the visceral pleura. Also, SFTs of the diaphragm are even rarer [3]. In the literature, few cases of giant SFT originating from the diaphragm, feeding on abdominal aortic branches. We aimed to present a rare case with giant peduncle SFT originating from the diaphragm.Case Presentation
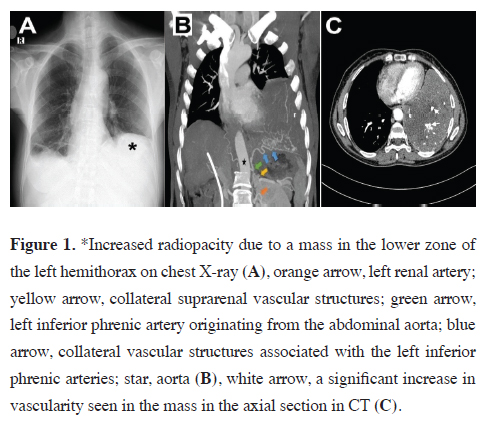
A 51-year-old female patient, who was operated on one year ago for a liver hydatid cyst, was referred to the thoracic surgery clinic. Chest radiography appearance was compatible with a mass filling the middle and lower zones of the left hemithorax (Figure 1a). In contrastenhanced computed tomography (CECT), a solid mass with smooth borders of 11×15×12 cm (TR×AP×CC) in size was detected in the left hemithorax, starting from the level of the upper lobe lingular segment, and filling the lower zone almost totally; the collateral arterial vascular structures associated with the left renal-phrenic artery showed a course and contains calcification and necrotic areas in some places (Figures 1b,c). Contrast-enhanced thoracic MRI was performed to evaluate invasion to neighboring structures more clearly. MRI showed a mass lesion with hypointense cystic and necrotic areas on T1A series, hyperintense cystic and necrotic areas on T2A series, no diffusion restriction on diffusion examination, no extension to the paravertebral area, no destruction of adjacent costae, and heterogeneous contrast uptake except for the cystic and necrotic area in the center.The tru-cut biopsy result was reported as a lesion containing collagenized stroma and spindle cell areas. Patient’s laboratory findings and tumor markers (CEA = 0.79 ng/mL, CA15-3 = 8.8 U/mL; CA19-9 = 14.1 U/ mL; CA125 = 7.6 U/mL).were within the normal limits.
 Click Here to Zoom |
Figure 1: *Increased radiopacity due to a mass in the lower zone of the left hemithorax on chest X-ray (A), orange arrow, left renal artery; yellow arrow, collateral suprarenal vascular structures; green arrow, left inferior phrenic artery originating from the abdominal aorta; blue arrow, collateral vascular structures associated with the left inferior phrenic arteries; star, aorta (B), white arrow, a significant increase in vascularity seen in the mass in the axial section in CT (C). |
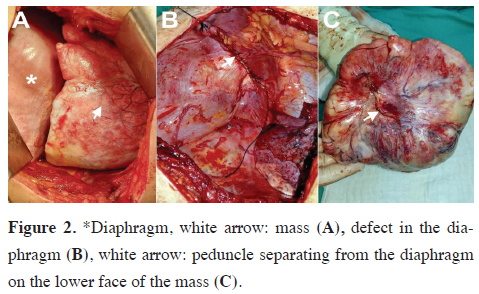
Surgery was performed with posterolateral thoracotomy. A mass was found adherent to the left lower lobe with an approximately 9 cm long peduncle, which was observed intraoperatively to originate from the left hemidiaphragm (Figures 2a,b). The portion of the diaphragm adjacent to the pedicle was resected. The mass was 16×20 cm in size and weighted 1450 gr (Figure 2c). After resection, the left lower lobe was not hypoplastic, filled the lower hemithorax.
 Click Here to Zoom |
Figure 2: *Diaphragm, white arrow: mass (A), defect in the diaphragm (B), white arrow: peduncle separating from the diaphragm on the lower face of the mass (C). |
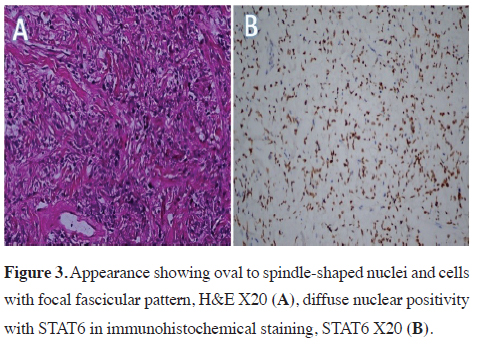
Embolism protocol computed tomography was performed on patient who had complaints of dyspnea on the first postoperative day and pulmonary embolism findings were observed. Low–molecular weight heparin was started. The patient did not show any problems in clinical and radiological follow-ups and hence was discharged. In the postoperative immunohistochemical examination of the patient; neoplastic cells were positive with CD34, bcl2 and diffuse nuclear positive with STAT6 (Figure 3). Pancytokeratin, CD99, DESMIN, CD31, S100 were negative. The findings were reported as compatible with solitary fibrous tumor. Written informed consent was obtained from the patient for the publication of her data.
 Click Here to Zoom |
Figure 3: Appearance showing oval to spindle-shaped nuclei and cells with focal fascicular pattern, H&E X20 (A), diffuse nuclear positivity with STAT6 in immunohistochemical staining, STAT6 X20 (B). |
Discussion
SFTs are rare tumors that grow from mesenchymal connective tissue and originate from spindle cells. Although massive spindle cell tumors have been reported in the pleural space measuring 27×20×15 cm and weighing 2470 gr) [4], only a few comprehensive SFT presentations of the diaphragm origin have been discovered, as in our present case [3,5]. According to the 2015 World Health Organization classification, malignant SFTs are usually larger than 10 cm and comprise more than 4 per 2 mm2 of mitosis, hypercellularity, necrosis/hemorrhage, and nuclear pleomorphism. Mitosis–necrosis ratio is an important indicator of malignancy. Although the tumor, in this case, was 16×20 cm in size and weighed 1450 gr, it was classified as a predominantly diaphragmatic, benign, solitary fibrous tumor with no significant atypia or mitotic pleomorphism. Besides, the capsule was smooth and connected to the diaphragm with a peduncle. Moreover, while tumor marker levels are expected to be high in malignant SFTs(CA 72, 419.9 U/mL; CA 125, 525.6 U/mL) [5], tumor marker levels(CEA, 0.79 ng/mL; CA 15-3, 8.8 U/mL; CA 19-9, 14.1 U/mL; CA 125, 7.6 U/mL) were within normal limits in the current case. According to Karen Harrison-Phipps et al (2009) [6], the probability of malignancy increases as the tumor size grows. Normal tumor markers and wellcircumscribed mass capsules, as in our case, may indicate that SFT, regardless of size, is benign.In the present case, CECT showed that the mass was supplied by diffuse tortuous collateral arterial structures originating from the abdominal aorta, related to the left phrenic artery and left renal artery. Capsular integrity must be preserved and more careful dissection should be performed in cases with aortic blood supply. Also, lung dissection is recommended after separating the peduncle and controlling the arterial feeding in SFTs, whose blood supply comes from the systemic circulation.
In conclusion, to the best of our knowledge, this is one of the few cases of giant peduncle SFT originating from the diaphragm that was feeding on the abdominal aorta in the English literature. In such cases, en-bloc surgical resection is currently accepted as the universal treatment method. Complete resection provides the best survival in malignant and benign cases. Therefore, surgery is recommended without wasting time after the detection of SFTs originating from the diaphragm.
Declaration of conficting interests
The authors declared no conficts of interest with respect
to the authorship and/or publication of this article.
Funding
The authors received no financial support.
Authors’ contributions
HEC,SEA,VAA,RY,ID: conceived and designed the current
case report, co-wrote the paper, collected the clinical
data. The authors discussed the case under the literature
data together and constituted the final manuscript.
Reference
1) Batirel HF, Demirhan R. Solitary fibrous tumors of the pleura.
TTD Plevra Bült 2010; 4: 13-16.
2) de Perrot M, Fischer S, Brundler MA, Sekine Y, Keshavjee S.
Solitary fibrous tumors of the pleura. Ann Thorac Surg 2002;
74: 285-93.
3) Ge W, Yu DC, Jiang CP, Ding YT. Giant solitary fibrous tumor
of the diaphragm: a case report and review of literature. Int J
Clin Exp Pathol 2014; 7: 9044-9.
4) Dongel I, Yazkan R, Duman L, Ozturk O, Kapucuoğlu FN.
Huge inflammatory myofibroblastic tumor of pleura with concomitant
nuchal fibroma. Ann Thorac Surg 2013; 96: 1461-4.






