

Summary
Sur Coil stands out as one of the most widely utilized agents for vascular embolization. While the occurrence of coil migration into the pulmonary artery is an infrequent event, the approach to treatment varies based on the duration between the procedure and the appearance of symptoms, as well as the specific symptoms exhibited. In this particular case, we share an instance where surgical intervention was conducted at the age of 41 due to coil migration, emphasizing the preservation of lung parenchyma. It is noteworthy that, even in the later stages, the secure removal of the coil can be achieved through surgical procedures designed to safeguard the lung tissue. I am confident that this lung-preserving approach represents a commendable strategy for such cases.Introduction
Vascular malformations are primarily addressed through interventional radiological procedures, benefitting from their diminished invasiveness and lower complication rates, attributed to advancements in angiography and associated technologies. Nevertheless, the infrequent event of migration of the commonly utilized embolic agent, the coil, may be encountered during the procedure. The approach to follow-up and treatment can vary, considering the patient's symptoms, findings, and the duration elapsed since the intervention [1,2].In this context, we present a case where coil embolization was initially applied for an external iliac vein aneurysm. Subsequently, surgical intervention became necessary due to the migration of the coil into the pulmonary artery.
Case Presentation
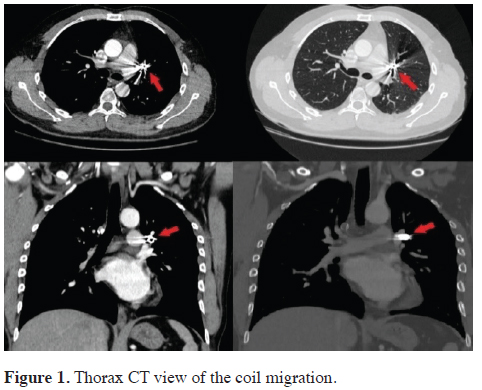
A male patient, aged 41, underwent coil embolization six years ago for a 5 cm aneurysm in the left external iliac vein, performed by interventional radiology. The patient remained symptom-free until a year ago when he started experiencing cough and shortness of breath. Diagnostic tests revealed a foreign object resembling a coil in the anterior branch of the left pulmonary artery trunk (Figure 1). Subsequently, the patient was referred to our clinic. During the patient's history, it was mentioned that five coils were used for the iliac vein, but post-procedural images were unavailable. As a result, the existing image was assumed to represent the coil.
 Click Here to Zoom |
Figure 1: Thorax CT view of the coil migration. |
The patient was initially referred to the interventional radiology clinic, and due to the six-year interval since the procedure, the anticipation of epithelialization and the high risk of complications led to the decision to forgo further interventional procedure. A surgical approach was chosen, and entry into the thoracic cavity was achieved through a left lateral thoracotomy incision. Complete dissection of the pulmonary artery allowed for the visualization of the anterior trunk. Irregular and rigid characteristics were noted along the wall of the anterior trunk from its origin in the pulmonary artery. Palpation revealed an object consistent with a foreign body along a 2cm length of the anterior trunk. Vascular clamps were applied proximally and distally to control the pulmonary artery. The anterior trunk was longitudinally opened, exposing the foreign body. Using forceps, the foreign body was successfully extracted (Figure 3). Intraoperative fluoroscopy revealed the presence of a residual coil within the anterior trunk artery. Consequently, the dissection of the anterior trunk was extended to locate and remove a second coil. Subsequently, the anterior trunk was primarily sutured and closed longitudinally. The lengths of the coils were measured as 1.5 meters for the first segment and 4.5 meters for the second segment (Figure 4).
 Click Here to Zoom |
Figure 2: Intraoperative view of coil removal. |
 Click Here to Zoom |
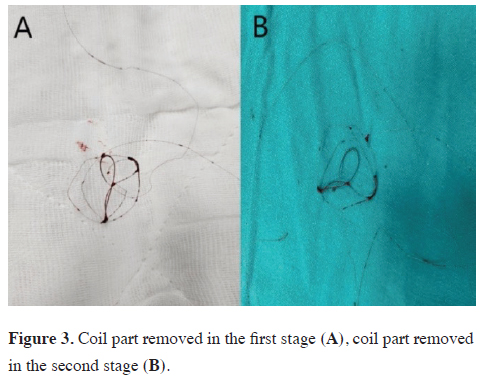
Figure 3: Coil part removed in the first stage (A), coil part removed in the second stage (B). |
 Click Here to Zoom |
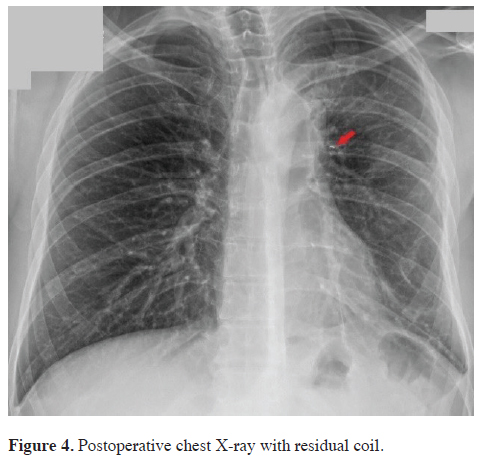
Figure 4: Postoperative chest X-ray with residual coil. |
During intraoperative assessment, an epithelized coil fragment of up to 5 mm was observed within the vascular structure, and no additional intervention was deemed necessary. Follow-up chest X-rays did not reveal any additional findings aside from the 5 mm linear coil along the vessel wall (Figure 4). The patient, who underwent intraoperative heparinization and continued anticoagulant therapy postoperatively, was monitored with a drainage tube for 10 days due to hemorrhagic drainage. Afterward, the drainage tube was removed, and the patient was discharged in a healed condition. Subsequent follow-ups at the 6th month showed a complete resolution of symptoms, with no additional complaints observed. Furthermore, when the patient's respiratory function test was evaluated comparatively preoperatively and postoperatively, an increase in respiratory capacity was noticeable despite the thoracotomy. Written informed consent was obtained from the patient for the publication of his data.
Discussion
The use of coil embolization has been actively employed since its efficacy was proven in 1975. The primary advantage of this procedure is its less invasive nature compared to surgical interventions, resulting in fewer complications. A coil is a material created by interweaving two wires, and its shape and covering can vary depending on the materials used. With its shape memory, it fills the structure from the moment it is withdrawn from the catheter, leading to vascular occlusion [1].One of the significant complications of coil embolization is coil migration. The most crucial risk factor for incorrect placement is reported to be the mismatch between the aneurysm area to be embolized and the coil diameter. Although the migration rate is reported in the literature as 0.7-4%, and misplaced coils have been shown to reach various target organs, placement in the pulmonary artery is emphasized to be quite rare. Since most cases do not result in end-organ damage and remain asymptomatic in different organ placements, additional interventional procedures are generally not required [1].
Reviewing cases of coil misplacement in the pulmonary artery in the literature, it is observed that different principles were adopted in almost all cases. In two cases where a coil misplaced immediately after the procedure was detected, the decision for follow-up was made due to the absence of active complaints, no decrease in saturation, and no development of hypotension. The patient was successfully monitored without the need for additional interventions [1,3].
In another case, a patient who underwent coil embolization for pelvic congestion syndrome three months ago developed sudden pleuritic pain, dyspnea, and orthopnea. After excluding diseases such as pneumothorax and pulmonary thromboembolism through differential diagnosis, coil misplacement in the pulmonary artery branch was detected. Due to the patient's active complaints and the short time elapsed since the procedure, a less invasive intervention was performed to remove the coil through interventional vascular procedures. Although a residual small coil fragment was reported, the procedure was terminated due to the regression of active symptoms and the increased risk of complications. The patient was successfully monitored [2].
In yet another case, coil embolization was performed three years ago, and in a patient with a cough complaint for two months, coil misplacement in the pulmonary artery was detected. The coil was removed along with a lower lobectomy, and surgical resection was primarily chosen because the procedure had taken place for an extended period, making epithelialization and invasion into the vessel wall highly probable [4].
In our case, the decision for surgical intervention instead of follow-up was primarily due to the patient's newly developed dyspnea, with no additional pathology detected apart from coil migration explaining the existing complaint. Opting for a less invasive procedure, such as interventional radiological procedures, over surgery aligns with the literature, correlating with the time elapsed since the procedure and the increased risk of coil invasion into the vessel wall and complications. Similar to the case presentation, a residual coil fragment remained in our study, but due to the regression of active symptoms and the potential for increased complications, the procedure was terminated, and the patient was successfully monitored.
Coil migration is a rare occurrence. Especially the performance of coil removal with interventional vascular procedures in the early period and the combined procedure with lung resection in the late period are much rarer. In our case, as observed in the literature, lung-preserving surgical procedures can be successfully performed even in a chronic process. In cases with coil migration, according to the literature, additional interventions are not planned for asymptomatic cases during follow-ups. However, as in our case, it can lead to additional symptoms years later, so one should remain vigilant.
In conclusion, although pulmonary artery coil migration can rarely be observed after interventional vascular embolization, the general approach in the early period is removal through vascular interventional methods, and in the late period, surgical resection is considered if it causes symptoms and signs. As in our case, lung-preserving surgical procedures can be successfully applied even in a chronic process.
Declaration of conficting interests
The authors declared no conficts of interest with respect
to the authorship and/or publication of this article.
Funding
The authors received no financial support.
Authors’ contributions
MÇ;MB;FS;KA: conceived and designed the current
case report, co-wrote the paper, collected the clinical
data. The authors discussed the case under the literature
data together and constituted the final manuscript.
Reference
1) Su L, Wang D, Han Y, Fan X. Coil Migration to the Pulmonary
Artery during Endovascular Embolization Treatment in a Patient
with Arteriovenous Malformation in the Right Ear. Intern
Med 2015; 54: 2873-5.
2) Guerrero A, Theophanous RG. A Case Report of a Migrated
Pelvic Coil Causing Pulmonary Infarct in an Adult Female.
Clin Pract Cases Emerg Med 2020; 4: 436-9.



