2Department of Radiology, School of Medicine, Ondokuz Mayıs University, Samsun, Turkey
3Department of Pathology, School of Medicine, Ondokuz Mayıs University, Samsun, Turkey DOI : 10.26663/cts.2017.0015
Summary
Thymic cysts are rarely seen pathologies among mediastinum. They are benign lesions and constitute 1-2% of all tumors in mediastinum. Seventy nine-year-old patient admits to neurology specialist with nausea and dizziness. In left anterior of mediastinum of the patient, smooth margin, cystic lesion with homogenous liquid density in dimensions of 160x130x83 mm is seen in thorax CT. Video assisted thoracoscopic surgery is applied to the patient with diagnosis of intrathoracic, extrapulmonary cystic lesion and lesion is totally excised. Patient is discharged on third day postoperatively with full recovery. Histopathologic examination of the excised lesion reports that it was thymic cyst. Thymic cysts, rarely seen lesions in mediastinum, can be in large sizes and be asymptomatic. They can be treated surgically using video assisted thoracoscopic surgery.Introduction
Thymic cysts are rare seen pathologies among benign lesions and constitute 1-2% of all mediastinal tumors [1-4]. Thymic cysts can be localized at any part of servico-diaphramatic region and can be seen most frequently in the anterior mediastinum or in the neck. They originate from fetal thymopharyngeal canal residual and categorized as congenital and acquired according to their etiologies. Congenital thymic cysts are typically have thymic tissue on the walls, they composed of flat epithelium and they are unilocular body that include serous liquid [3,4].In this case report an asymptomatic huge thymic cyst diagnosed at elderly age is presented under the light of the literature.
Case Presentation
79-year-old female patient admitted to a neurology specialist with nausea and dizziness. PA chest radiography revealed a mass lesion which completely fills left middle and lower zone of the left hemithorax and obliterates the left boundary of the heart (Figure 1).
 Click Here to Zoom |
Figure 1: PA chest radiography shows a lesion at left middle and lower zone in paracardiac zone and obliterating the left boundary of the heart. |
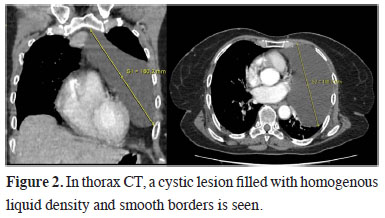
Thorax CT revealed a cystic lesion located between arcus aorta and diaphragm, 160x130x83 mm in size, with homogenous liquid density and smooth borders (Figure 2). In physical examination, breath sounds were decreased in lower left zone. Routine laboratory results were normal.
 Click Here to Zoom |
Figure 2: In thorax CT, a cystic lesion filled with homogenous liquid density and smooth borders is seen. |
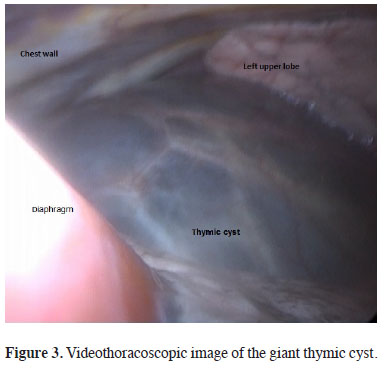
Video assisted thoracoscopic surgery was performed for this intrathoracic extrapulmonary cystic lesion. During the exploration of the left hemithorax, in the paracardiac area a giant lesion that goes through mediastinum and reaches cervical area was seen (Figure 3).
 Click Here to Zoom |
Figure 3: Videothoracoscopic image of the giant thymic cyst. |
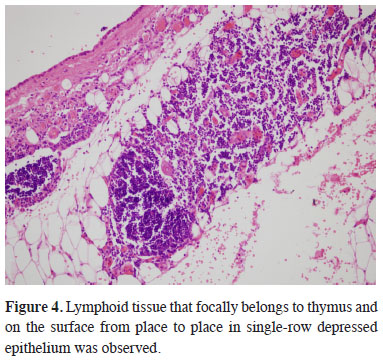
Lesion was unilocular and filled with a serous liquid. Approximately 800 mL of liquid was aspirated and the lesion was excised totally. Patient was discharged in the third day post-operatively without any problem. The histopathological examination of 14x11 cm lesion revealed lymphoid tissue that focally belongs to thymus. On the surface a single-row depressed epithelium was observed on different sections and reported as (Figure 4).
 Click Here to Zoom |
Figure 4: Lymphoid tissue that focally belongs to thymus and on the surface from place to place in single-row depressed epithelium was observed. |
The patient was discharged uneventfully and in the second year follow-up no recurrence was observed.
Discussion
Thymic cyst was first defined by Lieutaud in 1982 and it constitutes less than 1% of all mediastinal lesions. Thymic cysts can be congenital or acquired. Congenital ones develop through persistent thymopharyngeal canal. Trauma, inflammatory diseases, operative attempts and radiation were reported in the etiology of acquired thymic cysts. They are mostly seen between 20 and 50 years of age and they can be unilocular or multilocular. Unilocular cysts have thin walls, containing a serous liquid and mostly congenital. Multilocular cysts have thicker walls, containing a blurry, gelatinous liquid. In this type of cysts, similar etiological factors may play a role in the development like acquired ones [1-5].Thymic cysts are generally asymptomatic and are detected in random chest radiographies. In symptomatic patients, dyspnea, cough, chest pain, dysphagia, hoarseness and Horner syndrome may be seen. Symptoms depend on the location/size of the cyst and its relation to the neighboring organs [4,5]. Thymic cysts may develop anywhere between the neck and diaphragm. They are mostly localized in the anterior mediastinum and their diameter is between 5 and 30 cm [1,6]. In the differential diagnosis mediastinal located mesothelial cysts, bronchogenic cyst, cystic teratoma, cystic lymphangioma and germ cell tumors should be considered [4,5].
Thymic cysts are generally diagnosed radiological methods and become definite diagnosis was achieved via histopathological examination. In thymic cysts although low, there is a potential to develop malignancy. Additionally, when they reach large diameters due to compression of adjacent structures surgical removal of the cyst is the most preferred treatment. Thoracotomy, sternotomy and video assisted thoracoscopic surgery are other approaches in treatment [2,4,5]. For elderly patients when operative treatment cannot be performed, it is reported that sclerosing with ethanol can be an option [7]. Following an operative treatment 2% relapse rate is reported in the literature [8].
In this case, thymic cyst filled almost all of the left hemithorax and although it had been compressing the neighboring organs it was asymptomatic. In pre-operative evaluation lesion thought to be a pleuropericardial cyst and video assisted thoracoscopic surgery was decided. In exploration, cyst reaches from front mediastinum to left hemithorax and diaphragm. After the removal of the liquid inside the cyst, excision with video assisted thoracoscopic surgery became easier and totally excised. Patient was discharged shortly after the operation and in the follow up no relapse was seen.
In conclusion, thymic cysts, can reach huge sizes without causing any symptoms. Operative excision via video assisted thoracoscopic surgery would provide both final diagnosis and treatment. Although it is unlikely, thymic cysts should be followed for relapse.
Declaration of conflicting interests
The author declared no conflicts of interest with respect to the authorship and/or publication of this article.
Funding
The author received no financial support
Reference
1) Brown LR, Aughenbaugh GL. Masses of the anterior mediastinum: CT and MR imaging. AJR Am J Roentgenol 1991; 157: 1171-80.
2) Suster S, Rosai J. Multilocular thymic cyst: an acquired reactive process. Study of 18 cases. Am J Surg Pathol 1991;15: 388-98.
3) Bruno VD, Mariscalco G, Franzi F, Miceli A, Piffaretti G, Sala A. Ectopic congenital thymic cyst in the right pleural cavity. Asian Cardiovasc Thorac Ann 2010; 18: 486-488.
4) Rocco G, Shields TW. Mesothelial and other less common cysts of the mediastinum. In: Shields TW, Lo Cicero J, Reed CE, Feins RH, editors. General Thoracic Surgery. Volume 2. 7th ed. Philadelphia: Lippincott Williams and Wilkins, 2009: 2539-50.
5) Takeda S, Miyoshi S, Minami M, Ohto M, Masaoka A, Matsuda H. Clinical spectrum of mediastinal cysts. Chest 2003; 124: 125-32.
6) Gönüllü U, Güngör A, Savas I, Özdemir Ö, Mogulkoc G, Alper D,et al. Huge thymic cysts. J Thorac Cardiovasc Surg 1996; 112: 835-6.






