2Thoracic Surgery, Medicana International Istanbul Hospital, Istanbul, Turkey
3Department of Pulmonology, Istanbul Arel University Medical Faculty and Medicana International Istanbul Hospital, Istanbul, Turkey
4Department of Thoracic Surgery, Istanbul Sisli Hamidiye Etfal Research and Training Hospital, Istanbul, Turkey DOI : 10.26663/cts.2018.00016
Summary
Congenital cystic adenomatoid malformation (CCAM) is mostly recognized in children and adult presentation is rare. Here, a 42-year-old male patient was presented. He had a previous history of pneumothorax, and radiologically there were multiple bullous lesions in the right upper lobe, as well as a nodular lesion of 2 cm. He underwent right upper lobectomy and middle lobe wedge resection which revealed CCAM type I and hamartoma of the lung. Less than 70 adult cases of CCAM have been reported in the literature. Lung cancer accompanying CCAM or malignant transformation in adult are rarely described. But to our knowledge, this is the first adult case of CCAM with hamartoma. CCAM should be considered in the differential diagnosis of multicycstic lesions in adults with a history of pneumothorax, and the surgical resection is the treatment of choice.Introduction
Congenital cystic adenomatoid malformation (CCAM) of the lungs are rare congenital cystic lesions with an incidence of 1 in 25,000 to 35,000 pregnancies [1]. CCAM is firstly defined as a distinct disease by Chin and Tang in 1949 [2]. The disease was classified into 3 groups, then expanded into 5 types with a new name as congenital pulmonary airway malformation [3,4]. Most cases (80 to 85%) are recognized in the first 2 years of life, and adult presentation of CCAM is uncommon [5,6]. CCAM in adults may be complicated by pulmonary bacterial infections and accompanied by adenocarcinoma of the lung [5-7]. Here we described an adult CCAM case accompanied by hamartoma and treated with lobectomy.Case Presentation
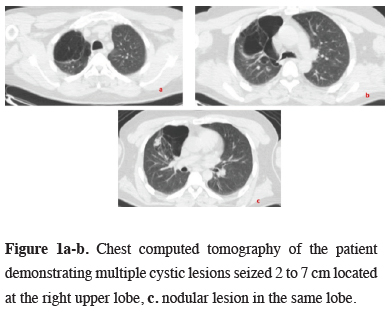
A 42-year-old non-smoker male patient presented with progressing dyspnea and dry cough. Dyspnea was mostly seen on exertion, and the patient reported that this affected his work and quality of life during the last two years. He had a history of a right pneumothorax treated with chest tube 19 years ago. On admission, the patient had normal vital signs, no fever. The laboratory test results did not show any abnormalities. Pulmonary and cardiac physical examination were unremarkable. Chest X-ray showed increased hyperlucency in the right upper zone. High resolution computed tomography (CT) of the chest demonstrated multiple bullous lesions of several diameters (2 to 7 cm), and a nodular lesion seized 2.0 x 1.4 cm in the right upper lobe (Figures 1a-c). PET-CT scan revealed a SUVmax value of 0.4 for the nodular lesion. Bronchoscopy was negative for any bronchial lesions. Since the patient had a previous history of pneumothorax, and multiple bullous lesions accompanied by a nodule of unknown pathology, a surgical resection was planned. The patient underwent a right upper lobectomy and middle lobe wedge resection without complication via a right posterolateral thoracotomy, since the videothoracoscopic approach was found unsuitable due to dense and heavy adhesions. The patient developed prolonged air leak and discharged with a Heimlich valve on the in the postoperative 9th day. The air leak dissolved and the valve was removed on the 14th postoperative day. The patient had an uneventful follow-up of 10 months without further complaints. He reported that the dyspnea resolved and he could return to his normal daily activities.
 Click Here to Zoom |
Figure 1a-b: Chest computed tomography of the patient demonstrating multiple cystic lesions seized 2 to 7 cm located at the right upper lobe, c. nodular lesion in the same lobe. |
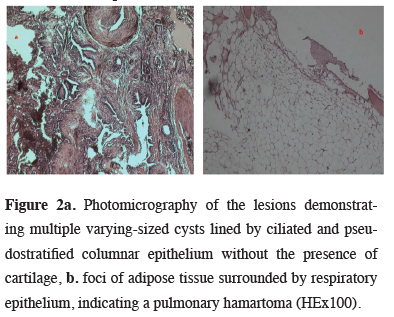
The pathological examination of bullous right upper lobe revealed multiple cystic lesions with adenomatous changes. Most cysts were lined by ciliated and some by pseudostratified columnar epithelium. The stroma around the cysts was mostly infiltrated by lymphocytes, and nearby capillaries were dilated which demonstrated chronic inflammation. There was no cartilage in the cyst walls (Figure 2a). These findings were consistent with type I CCAM. The pathological examination of the nodular lesion located nearby the bullous parts of the upper lobe demonstrated hyaline cartilage and foci of adipose tissue surrounded by cleft-like spaces lined by respiratory epithelium, indicating a pulmonary hamartoma (Figure 2b). There was no evidence of malignancy in the resected specimens.
 Click Here to Zoom |
Figure 2a: Photomicrography of the lesions demonstrating multiple varying-sized cysts lined by ciliated and pseudostratified columnar epithelium without the presence of cartilage, b. foci of adipose tissue surrounded by respiratory epithelium, indicating a pulmonary hamartoma (HEx100). |
Discussion
We reported an adult case with type I CCAM based on the radiological and pathological results. Type I CCAM is the commonest type corresponding to 65% of the cases. This type consists of one or multiple cysts measuring 3 to 7 cm and often affecting one lobe. The patient may be asymptomatic or have respiratory distress of several degrees. There are no other associated anomalies. Microscopically the cysts are lined with ciliated columnar epithelium. Mucigenic adenomatous cells are common. The presence of cartilage is extremely rare. Type II CCAM is formed by multiple middle-sized cysts (0.5 to 2 cm) and its incidence is 10 to 15%. Most cases are associated with other anomalies, most of which are incompatible with life. This type has no mucosal cells or cartilage. Type III CCAM is rare (5%) and characterized by clumps of small cysts not exceeding 0.2 cm. This type may involve the whole lung [3]. In 2002, two other types of CCAM were described [4]. Type 0 CCAM has firm and small lungs, and shows bronchiolar type airway with cartilage, smooth muscle and glands. Finally, type IV CCAM has peripheral large cysts of more than 10 cm lined by flattened epithelium.Eighty to 85% of the cases are recognized in the neonatal period, however there are several reports in adults [8,9]. Besides there exist three studies as review of the literature consisting of 11 to 60 patients [5-7]. Overall, less than 70 cases of adult cases with CCAM have been reported. Type I CCAM is more common in adults. Type II CCAM is reported in 17 to 45% [5-7]. The only patients with type III CCAM was reported by Barreiro et al [5]. According to these limited number of patients, CCAM in adults is seen in patient aged between 20 to 80 years, with a slight male predominance, and mostly involves upper lobes. Our patient has 42 years-old and the disease affected mostly right upper lobe and some part of the middle lobe.
In adult patients, CCAM may cause pneumonia, abscess formation, fungal and tuberculous infections, hemoptysis, and air embolism [8]. A history of pneumothorax has been reported in only 8 patients [6,7,9]. As far as we know, our patient has the 9th adult case with previous pneumothorax.
The presences of either accompanying lung cancer or malignant transformation are rare but troublesome problems in adult patient with CCAM. Hamanaka et al [8] reported 8 patient with adenocarcinoma in their review consisting of 60 patients. Pulmonary tumorlets have been reported only once [10]. To our knowledge, our patient is the first case of CCAM accompanied with hamartoma.
The treatment of CCAM in adults, as well as in children, is the complete surgical resection. Lobectomy is the mostly preferred resection type, followed by segmentectomy, pneumonectomy, and wedge resection [5-8]. We performed a right upper lobectomy and middle lobe wedge resection to achieve the complete resection.
In conclusion, CCAM should be considered in the differential diagnosis of multicycstic lesions located in one lobe in adults with a history of pneumothorax, although adult cases of CCAM are very rare. The surgical resection is the treatment of choice in all cases of CCAM to perform a histological examination of the lesion and to prevent potential neoplastic transformation.
Declaration of conflicting interests
The authors declared no conflicts of interest with respect to the authorship and/or publication of this article.
Funding
The authors received no financial support.
Reference
1) Sahu S, Muthuvel S, Naware SS, Dhavala SS. Congenital cystic adenomatoid malformation of lung. Med J Armed Forces India 2008: 64: 268-9.
2) Chin KY, Tang MY. Congenital adenomatoid malformation of one lobe of a lung with general anasarca. Arch Pathol (Chic) 1949; 48: 221-9.
3) Stocker JT, Madewell JE, Drake RM. Congenital cystic adenomatoid malformation of the lung: classification and morphologic spectrum. Hum Pathol 1977; 8: 155-71.
4) Stocker JT. Congenital pulmonary airway malformation: a new name and an expanded classification of congenital cystic adenomatoid malformation of the lung. Histopathology 2002; 41: 424-31.
5) Barreiro TJ, Henn L, Ingham S, Sypert M. Congenital pulmonary airway malformation in a 36 year-old female. Respir Med Case Rep 2016; 17: 34-6.
6) Hamanaka R, Yagasaki H, Kohno M, Masuda R, Iwazaki M. Congenital cystic adenomatoid malformation in adults: report of a case presenting with a recurrent pneumothorax and a literature review of 60 cases. Respir Med Case Rep 2018, https://doi.org/10.1016/j.mcr.2018.02.002
7) Hellmuth D, Glerant JC, Sevestre H, Remond A, Jouneaux V. Pulmonary adenomatoid malformation presenting as unilobar cysts in an adult. Respir Med 1998; 92: 1364-72.
8) Feng A, Hourong C, Sun Q, Zhang Y, Chen L, Meng F. Congenital cystic adenomatoid malformation of lung in adults: 2 rare case report and review of the literature. Diagn Pathol 2012; 7: 37.






