2Department of Pediatric Hematology and Oncology, Dr. Sami Ulus Woman’s Health and Children Education and Research Hospital, Ankara, Turkey DOI : 10.26663/cts.2018.00018
Summary
Primary malignant mediastinal germ cell tumors are rare in childhood. Despite the metastasis to lung, liver, brain and bone is possible but sternal metastasis is unusual. Both tumor and its metastases treated with surgical resection, if possible followed by chemotherapy. We present a case primary malignant germ cell tumor, which has metastasis to lung and to sternum. We performed complete tumor resection, metastasectomy, sternal resection and then reconstructed by titanium plate and polypropylene graft.Introduction
Mediastinal germ cell tumors (GCTs) are rare in childhood. Primary malignant mediastinal GCT (PMMGCT) is exceedingly rare and representing 0.32-2% of all childhood cancers [1]. They can metastasize to lung, liver, bone and brain but sternal metastasis is unusual [2]. They treatment is with multidisciplinary approach that includes surgery, chemotherapy (CT) with or without radiotherapy (RT) [1].We present a case primary malignant germ cell tumor, which has metastasis to lung and sternum. After resection of the sternum totally, a sternal reconstruction with a tough prosthesis should be performed to protect intrathoracic organs from injuries and infection which will also help to prevent the paradoxical respiration. Recently, polypropylene mesh with moldable titanium plates and costal clips combination were used in chest wall reconstruction [3]. According to our knowledge, there was no report in the English literature about a PMMGHT case which metastasized to sternum and due reconstructed by polypropylene mesh with titanium plates and costal clips after a total sternal resection. Here, we intent to present this case and our clinical experience.
Case Presentation
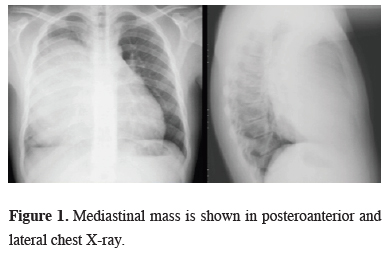
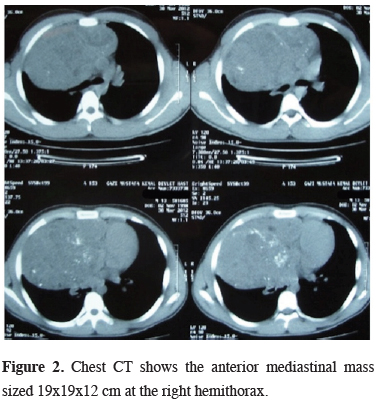
A 13-years-old male who was suffering from persistent cough and chest pain for a month were examined in pediatric clinic. The posteroanterior chest x-ray showed a mediastinal enlargement and lateral x-ray revealed an anterior mediastinal mass (Figure 1). Computed tomographic scan of the chest (CT) showed a 19 x 19 x 12 cm size mediastinal mass that placed in anterior mediastinum (Figure 2).
 Click Here to Zoom |
Figure 1: Mediastinal mass is shown in posteroanterior and lateral chest X-ray. |
 Click Here to Zoom |
Figure 2: Chest CT shows the anterior mediastinal mass sized 19x19x12 cm at the right hemithorax. |
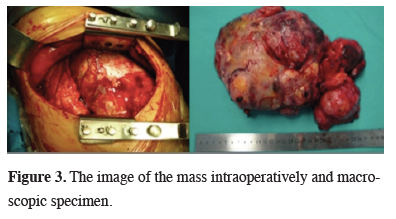
Routine blood tests were normal except the liver function test that were higher at the border. The serum level of alpha-fetoprotein (AFP) and beta-human chorionic gonadotropin (b-HCG) of this patient were elevated. (AFP > 3000 ng/mL (normal range = 0-20 ng/mL) B-HCG=178.42 mIU/mL (normal range = 0-10 mIU/mL)). Carcinoembryonic antigen (CEA) level was 2.76 ng/mL which was slightly higher (normal range = 0-2.5 ng/mL). His scrotal ultrasonography and whole body bone scintigraphy were normal. The patient was referred to our clinic with the prediagnosis of mediastinal mass. While the patient was hospitalized, an informed consent was taken from his parents. After essential preoperative preparation, we performed biopsy from the mass by right anterior mediastinotomy as a small specimen via a needle biopsy might not be sufficient for an immunohistochemical study and which might lead to a dignostic confusion. Furthermore, heterogeneity of the tumor and areas of necrosis might decrease the reliability of a needle biopsy. Frozen section was reported as mature cystic teratoma. Whereat, in the same session, we performed right posterolateral thoracotomy. A capsuled mass that is filling almost all hemithorax was determined in the exploration and excised totally (Figure 3). Postoperative pathological result was reported as, mixed germ cell tumor that included immature and mature components (yolc-sac-tumor + choriocarcinoma + seminoma). The chemotherapy protocol that included gemcitabine, docetaxel and paclitaxel in pediatric oncology clinic was started and the patient was followed periodically. The AFP values decreased to 13.4 ng/mL with the effect of chemotherapy.
 Click Here to Zoom |
Figure 3: The image of the mass intraoperatively and macroscopic specimen. |
After the third cure at postoperative eighth month, chest CT showed a 12 x 19 mm lobule nodule at the right lower lobe of the lung, a 12 mm nodule at adjacent the major fissure and 17 mm hypodense area at anterior mediastinum. AFP values were progressively increased and reached to a level of 13.309 ng/mL. Whereupon, mediastinal mass excision, multiple wedge resection and lymphatic node excision was performed by right re-thoracotomy. Pathological results verified the mediastinal mass was a mixed germ cell tumor (yolc-sac-tumor + embryonal carcinoma), all wedge resections were yolc-sac-tumor metastasis and the number 11 lymph node was mature cystic teratoma metastasis. A 13-cure chemotherapy protocol that including Vincristine, Actinomycin-D, Cyclophosphamide and Adriamycin (VACA) was started. Again, AFP levels were declined to 10.5 ng/mL with chemotherapy.
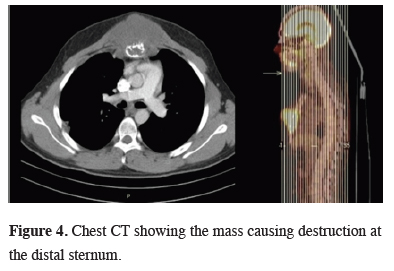
During the chemotherapy protocol, chest CT scan that was performed after recognizing a swelling at the front side of the chest wall releaved a 4.3 x 3.9 x 4.5 cm size mass which destructed the distal part of the sternum (Figure 4).
 Click Here to Zoom |
Figure 4: Chest CT showing the mass causing destruction at the distal sternum. |
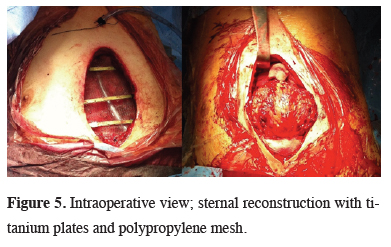
Therefore, screening for whole body positron emission tomography (PET-CT) showed an 7.4 x 6.4 x 8.0 cm size mass which destructed middle and distal part of the sternum and also invaded the medial part of the pectoralis major muscle and showed exophytic elongation to subcutaneous tissue. The level of AFP, which was reduced by about 3 months in the follow-up, increased progressively to a level of 33.591 ng/mL. Based on the increase in AFP levels and the findings of PET-CT, the tumor was decided to be chemotherapy-resistant. In consequence of resistance to chemotherapy, with the decision of the pediatric oncology council, we performed a total sternal resection. The defective area was reconstructed with 10 x 9 cm size polypropylene mesh and titanium rib clips were placed onto 3rd to 5th ribs bilaterally over the polypropylene mesh. Titanium plates were fixed to the rib clips transversely for the stability of the chest wall (Figure 5).
 Click Here to Zoom |
Figure 5: Intraoperative view; sternal reconstruction with titanium plates and polypropylene mesh. |
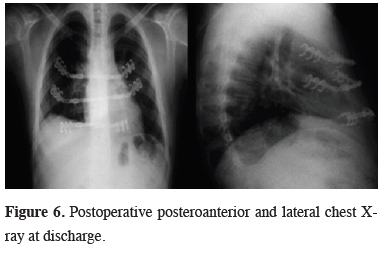
The surface was covered by a pectoralis major flap and skin. Postoperative pathological examination showed destruction in one area of the sternum macroscopically and the malign mixed germ cell tumor invasion microscopically. The patient was discharged at 7th day postoperatively (Figure 6).
 Click Here to Zoom |
Figure 6: Postoperative posteroanterior and lateral chest X-ray at discharge. |
Chemotherapy protocol was continued with Vinblastine, Adriamycin and Sorafenib. Unfortunately, the patient died by virtue of showing multiple metastasis after 31 months from the first operation.
Discussion
Primary mediastinal GCTs was reported to account 6-24% of mediastinal tumors and 3-4% of all GCTs. PMMGCT is more rare and representing 0.32-2% of all childhood cancers [1,4]. PMMGCTs divided into two groups: seminomas and nonseminomatous germ cell tumors (NSGCT). NSGCT group includes yolk-sac-tumor, embryonal carcinoma, choriocarcinoma, immature teratoma, teratocarcinoma and mixed tumor [5]. Mixed GCT is representing 8.5-9.3% of PMMGCTs [5,6]. Mixed GCT is mostly seen at mediastinum [1,4]. There is bimodal age distribution in PMMGCT. First peak is before age 3 and the second is in adolescent age like our case [6].GCTs metastasis to lung, liver, bone and brain [2]. Necchi et al. reported 25 (29.1% of all) lung metastasis and 8 (9.3% of all) liver, bone and brain metastasis cases [2]. They suggested chemotherapy after surgery in lung metastasis and performed metastasectomy to 20 patient of lung metastasis cases. They also reported poor prognosis in lung metastatic group [2]. In our case, lung metastasis was seen after 8 month of first diagnosis and metastasectomy was performed.
Due to poor prognosis, a multidisciplinary approach that includes surgery, chemotherapy with or without radiotherapy is advised. Cisplatin-based chemotherapy regimens recommended as the first line therapy. The most commonly used one is VIP (Etoposide, Ifosfamide and Cisplatin) protocol. The Pediatric Oncology Group (POG) and The Children’s Cancer Study Group (CCG) are recommending BEP (Bleomycin, Etoposide, Platin) protocol as an alternative treatment. However, when a surgical intervention is necessary for residual tumor, due to lung toxicity of bleomycin, oxygen requirement of the patient could increase [2,5,7]. In case of progression, low response and recurrence second-line chemotherapy is indicated. Commonly cisplatin, etoposide and ifosfamide combinations are used. However, TIP (paclitaxel, ifosfamide, cisplatin), TOG (paclitaxel, oxaliplatin, gemcitabine) and TPG (paclitaxel, cisplatin, gemcitabine) protocols are used in cases which are resistant to therapy [2]. Nevertheless, successful treatment of GCT in childhood required complete resection of the mass, if possible [1,4]. Despite different chemotherapy protocols, there were lung, lymph node and sternal metastasis in our case.
The treatment of the sternal tumors is en-bloc surgical resection [3]. It is also indicated in chemoresistance GCT so we performed metastasectomy for lung lesions and a sternal resection in this case. Wide resection of the sternum will result with a defect. Therefore, sternal reconstruction with a tough prosthesis should be performed to prevent paradoxical respiration and to protect lungs, heart and great vessels from trauma and infection [3,8]. Until today, various of materials including homolog bone, muscle, fascia lata, omental or metallic meshes, polypropylene mesh, polyglycolic mesh, methyl methacrylate and silicon that replaced into two polypropylene or polyglactine patches are used in alone or combined way for sternal reconstruction [3,9]. The most commonly used and the firm one is the “sandwich” method which was formed by methyl methacrylate and silicon that replaced into two polypropylene or polyglactine patches. However, the preparation technique is hard and needs to be experienced. Complications like early breakage, infection and tissue damage with perioperative heat were reported in literature [10]. Recently, the use of titanium plates as a new method for the chest wall reconstruction was reported. Titanium is a non-corrosive material that could be applied by reserving chest wall anatomy and physiology. In addition, it is reported to cause no local infection. Briccoli et al. reported their cases maintains their daily activities after sternal reconstruction with titanium plates [3]. But metallic plates could cause lung injuries because of their affinities to tissue [3,8,9]. To prevent lung injury, Berthet et al. reported their technique by placing polytetraflouroetylene (PTFE) under the plates, otherwise Briccoli et al. achieved it by placing polypropylene mesh [3,9]. Thus, they could prevent tissue affinity of the plates to preserve lungs. Titanium does not disturb the visualization, both for magnetic resonance imaging (MRI) and for CT, without interrupting the oncologic patient’s follow up so it could be used in these patients safely [8,9]. We performed sternal reconstruction with titanium plate and polypropylene mesh after sternum resection. The patient maintained daily activities seamlessly in postoperative period.
Presence of lung metastasis and surgical resection are factors that influence survival in NSGCT [2]. The median survival rates for 3 and 5 years were 47.4% and 23%, respectively [5]. In NSGCTs, the diseases free survival and median survival rates were 59.5% and 71.4%, respectively [6]. Marina et al. reported the mortality risk as 6 times higher in patients who are older than 12 years, in thoracic GCTs [6]. Billmire et al. reported a higher mortality depending on tumor progression in male patients older than 15 years [7]. Our case was 13 years old, the disease showed a rapid progression and was lost at 31 month, postoperatively.
Despite the metastasis to lung, liver, brain and bone, sternal metastasis is rare in PMMGCT. The treatment of PMMGCT and its metastasis are surgical resection, if possible. In case of metastasis to sternum of PMMGCT sternal resection could be performed safely. To obtain an ideal rigidity and biocompatibility, titanium plate and polypropylene mesh can used in sternal reconstructions. Multiple surgical resections to mediastinal germ cell tumors and its metastasis could contribute survival time, if they are resistant to other therapies.
Declaration of conflicting interests
The authors declared no conflicts of interest with respect to the authorship and/or publication of this article.
Funding
The authors received no financial support.
Reference
1) Yalçın B, Demir HA, Tanyel FC, Akçören Z, Varan A, Akyüz C, et al. Mediastinal germ cell tumors in childhood. Pediatr Hematol Oncol 2012; 29: 633-42.
2) Necchi A, Giannatempo P, Lo Vullo S, Farè E, Raggi D, Marongiu M, et al. A prognostic model including pre- and postsurgical variables to enhance risk stratification of primary mediastinal nonseminomatous germ cell tumors: the 27-year experience of a referral center. Clin Genitourin Cancer 2015; 13: 87-93.
3) Briccoli A, Manfrini M, Rocca M, Lari S, Giacomini S, Mercuri M. Sternal reconstruction with synthetic mesh and metalic plates for high grade tumors of the chest wall. Eur J Surg 2002; 168: 494-9.
4) Lack EE, Weinstein HJ, Welch KJ. Mediastinal germ cell tumors in childhood. A clinical and pathological study of 21 cases. J Thorac Cardiovasc Surg1985; 89: 826-35.
5) Liu Y, Wang Z, Peng ZM, Yu Y. Management of the primary malignant mediastinal germ cell tumors: experience with 54 patients. Diagn Pathol 2014; 9: 33.
6) Marina N, London WB, Frazier AL, Lauer S, Rescorla F, Cushing B, et al. Prognostic factors in children with extragonadal malignite germ cell tumors: a pediatric intergroup study. J Clin Oncol 2006; 24: 2544-8.
7) Billmire D, Vinocur C, Rescorla F, Colombani P, Cushing B, Hawkins E, et al. Malignant mediastinal germ cell tumors: an intergroupstudy. J Pediatr Surg 2001; 36: 18-24.
8) Berthet JP, Canaud L, D’Annoville T, Alric P, Marty-Ane CH. Titanium plates and Dualmesh: a modern combination for reconstructing very large chest wall defects. Ann Thorac Surg 2011; 91: 1709-16.






