2Department of Thoracic Surgery, School of Medicine, Cumhuriyet University, Sivas, Turkey DOI : 10.26663/cts.2019.00024
Summary
Background: Foreign body (FB) aspiration is a serious clinical situation due to its life-threatening status and especially common in the childhood period. We aimed to present the diagnosis and treatment of foreign bodies in pediatric age group.Material and Methods: Files of 510 patients aged 16 years and below that underwent rigid bronchoscopy due to suspicion of FB aspiration between June 1994 and November 2017 were retrospectively reviewed. 263 cases were included to the study that underwent foreign body removal. The cases were assessed in terms of gender, age, type and localization of the foreign body, clinical complaint, radiological findings, treatment method, complication and mortality.
Results: Among the patients 45.6% were male and 54.4% were female. The aspirated foreign bodies varied from dried nuts to plastic, from hijab needles to beads. The most aspirated foreign body were dried nuts. 51% of them were removed from the right main bronchus, 31.9% from the left main bronchus, and 17.1% from the trachea. 97.8% of the foreign bodies were removed via bronchoscope. Thoracotomy was performed in 6 cases since the foreign bodies were not extractable with a bronchoscope or due to developing complications. No mortality occurred.
Conclusions: FB aspiration can lead to life-threatening complications in children aged 3 years or below. Bronchoscopy should be performed in all cases of foreign body aspiration, including suspicious cases. Notably, the bronchoscopy procedure should be carried out by a well-trained, experienced anesthesiologist-endoscopy team and with appropriate tools.
Introduction
Foreign body (FB) aspirations are situations that should be treated immediately due to its life-threatening status [1], and are most commonly seen in the pediatric age group [2]. The majority of the cases are children aged 3 years or below, and 7% of these children die due to aspiration [3,4]. The reasons of the high incidence rate in this age group are the fact that the molar teeth does not grind food items properly, speaking or playing while there is food in the mouth [5,6]. The aspirated foreign bodies may vary according to the sociocultural characteristics and nutritional habits of families and societies [7]. Liquids are more frequently seen in infants, organic food and parts of plastic toys are commonly encountered in children [2,8,9]. Golden standard in treatment is rigid bronchoscopy. However, flexible bronchoscopy is also useful in some cases [10]. In cases where rigid bronchoscopy is unsuccessful, foreign bodies are extracted with surgeries, including tracheostomy, bronchotomy and thoracotomy [11-13]. The immediate and reliable extraction of the aspirated foreign bodies is very significant in terms of preventing serious complications, including death [14].In this study, we aimed to present the clinical findings and outcomes of our pediatric patients that underwent FB extraction in our clinic.
Methods
Files of 510 patients aged 16 years and below that underwent rigid bronchoscopy due to suspicion of FB aspiration between June 1994 and November 2017 in our clinic were retrospectively reviewed. Approval of the ethical committee was obtained for the study.For the diagnosis; history of aspiration, clinical findings, physical examination and radiologic methods were used. 263 cases that underwent foreign body extraction were included to the study. In all cases, rigid bronchoscopy was performed under general anesthesia using muscle relaxants. The cases were assessed in terms of gender, age, type and localization of the foreign body, clinical complaints, radiological findings, treatment method, complications and mortality. Patients were also divided into three groups according to their time of diagnosis: in the first 24 hours group, in the first week and after the first week group.
Statistical Analysis
SPSS 22.0 software was used. Mann-Whitney U test was used to compare the differences between two groups. Chi-square test were used to compare the frequency of two or more groups. A p value of < 0.05 was considered significant.
Results
Among the 263 cases that underwent foreign body extraction, 120 (45.6%) were male and 143 (54.4%) were female children. The age of the patients ranged between 5 months and 16 years (mean age: 5 years 4 months). In age-wise patient distribution, it was seen that the 0-3 years age group was listed first with 59.3%, followed by 10 years and above group with 25.9% (Table 1). The most common complaints of the patients were coughing, shortness of breath, wheezing and fever.Table 1: Age distribution of cases that underwent bron-choscopy due to foreign body aspiration.
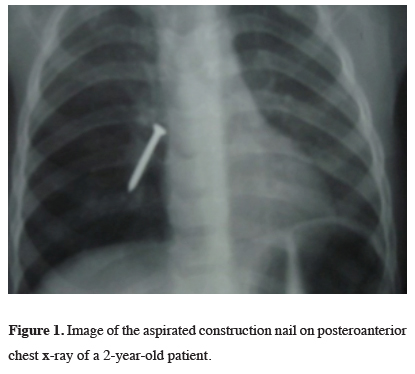
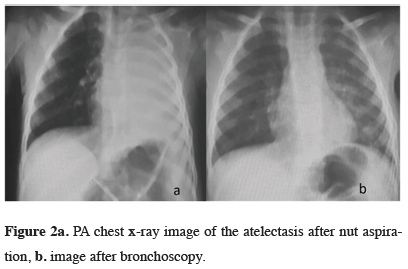
The most frequent radiological findings were radiopaque foreign body in 28.9% (76 cases) (Figure 1), followed by normal radiography in 24.7% (65 cases), unilateral hyperaeration in 19.8% (52 cases) and atelectasis in 15.2% (40 cases) (Figure 2).
 Click Here to Zoom |
Figure 1: Image of the aspirated construction nail on posteroanterior chest x-ray of a 2-year-old patient. |
 Click Here to Zoom |
Figure 2a: PA chest x-ray image of the atelectasis after nut aspiration, b. image after bronchoscopy. |
The foreign bodies were extracted from right main bronchus in 51% of the cases, from the left main bronchus in 31.9% and from the trachea in 17.1% (Table 2).
Table 2: Localizations of the foreign body.
The aspirated foreign bodies were varying objects ranging from dried nuts to plastic nylon, from hijab needles to beads. The most frequently aspirated foreign body were dried nuts. One case aspirated a plastic whistle (Figure 3). When analyzing the cases according to their time of diagnosis, most (61.9%) of the cases were diagnosed in the first week (Table
Table 3: Distribution of cases according to time of intervention.
The minimum and maximum time of application period to the emergency department was identified as 15 minutes and 6 years, respectively. Rigid bronchoscopy was performed on all patients with general anesthesia. Thoracotomy was conducted in six (2.2%) cases, because rigid bronchoscopy was inadequate or due to developing complications. No mortality was seen in our study group.
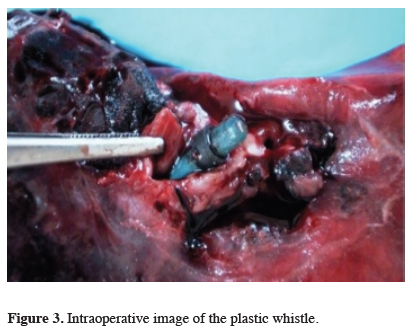
Click Here to ZoomFigure 3: Intraoperative image of the plastic whistle.
Discussion
FB aspiration is a serious situation that potentially results in death. The majority of the aspirations are seen in childhood period. Specifically, it may lead to more serious outcomes in children [15]. In literature, FB aspirations are more frequently seen in male children due to unexplainable reasons. This rate is about 2/1 [15-17]. However, in contrast to the literature, according to our results, FB aspirations were more frequent in female children. This was explained with the fact that hijab needle aspiration was more frequent in our country and all of these cases were seen in girls.Although FB aspirations are seen at every age, according to literature, it is most commonly seen between 1 and 3 years of age. This may be due to the tendency of children at this age to learn the world using their mouth [15]. Our patient group supports this fact.
Early diagnosis and treatment is important in preventing serious complications. In the pediatric patient group, the aspiration event is generally based on the observation of an adult. The presence of a witness is diagnostic. However, this observation may sometimes be unreliable [18]. The most important complaint of the patients at application to the hospital was coughing and rate of aspiration history among patients may be low. In our patient group, the history of aspiration rate was also low. However, this resulted from hiding the truth due to the social fear of the mother, rather than a witness not being present. Therefore, although there is no history of aspiration in the pediatric age group, FB aspiration should be considered in unexplainable and unresolved coughing despite treatment.
In many studies, organic foreign bodies were the most commonly aspirated foreign bodies, specifically in the pediatric age group. The rate of these foreign bodies ranges between 31.5% and 95% in literature [15].
Among organic bodies, the most common ones were dried nuts. This was supported in our study. However, the type and rate of foreign bodies varies according to country, diet and traditions. In developing countries, the majority of aspirated foreign bodies consist of organic bodies, while plastic bodies are more commonly seen in developed countries. In middle-eastern countries, like our country, aspiration of prayer beads, beads and hijab needle in girls is frequent due to cultural reasons [15]. In our study, hijab needle aspiration, particularly in female children, was common, although not being the most frequent.
Most of the aspirated foreign bodies (90%) are radiolucent, since most of them are food objects. Hence, indirect findings are seen in x-rays [19]. Of these, the most radiologically common ones are air trapping/hyperinflation (33%) and atelectasis (16%). Air trapping/hyperinflation are nearly perfect indicators of foreign bodies [20]. In our study group, since the most frequently aspirated object were food products, there were radiologically indirect findings supporting the literature.
Due to the anatomy of the bronchial tree, FBs are more common in the right main bronchus and its branches [15-17]. In the obtained data of our study, this hypothesis was supported with a foreign body aspiration rate of 51% in the right bronchial system.
In the literature, when analyzing the cases according to their time of diagnosis, the intervention rate at the first 24 hours ranges between 20.5% and 38.4%, and this rate varied between 57.6% and 71% at the first week [15]. Consistent with the literature, these rates were 29.7% for the first 24 hours and 61.9% for the first week in our study.
In our clinic all of the 510 cases that applied due to suspicion of foreign body aspiration underwent rigid bronchoscopy. Of these, foreign bodies were seen in 263 cases. The majority of the foreign bodies (97.8%) were extracted via rigid bronchoscopy. In our study, thoracotomy was performed in six (2.2%) patients due to inadequacy of rigid bronchoscopy or developing complications. Since the foreign body was too peripheral and was reachable via a forceps in 2 cases, since 2 cases that aspirated grass inflorescence developed massive hemoptysis, since one case that aspirated a plastic whistle developed bronchiectasis and the foreign body advanced to the pericardium in a case that aspirated a sewing needle, thoracotomy was performed. Moreover, laryngospasm was seen in 3 cases and cardiac arrest that resolved with intervention was seen in one case. The reason of the rarity of laryngospasm among patients was the use of corticosteroid before and after bronchoscopy, according to the recommendations in the literature [15]. In our study group, mortality was in none of the patients.
Conclusively, early diagnosis and treatment in pediatric foreign body aspirations are lifesaving. It should be noted that “suspicion” is the most important way to diagnosis. Notably, the bronchoscopy procedure should be performed by a well-trained, experienced anesthesiologist-endoscopy team and with appropriate tools. We consider that every possible problem may be resolved with education.
Declaration of conflicting interests
The authors declared no conflicts of interest with re¬spect to the authorship and/or publication of this article.
Funding
The authors received no financial support.
Reference
1) Katrancıoğlu Ö, Şahin E. Trakeobronşial Yabancı Cisim Aspirasyonlarında Bronkoskopik Yaklaşım. Turkiye Klinikleri J Pulm Med-Special Topics 2016; 9: 46-52.
2) Yıldızeli B, Yüksel M. Yabancı cisim aspirasyonları. Yüksel M, Kaptanoğlu M, eds. Pediatrik Göğüs Cerrahisi. İstanbul: Turgut Yayıncılık A.Ş; 2004. p.151-65.
3) Öncel M, Sunam GS, Ceran S. Tracheobronchial aspiration of foreign bodies and rigid bronchoscopy in children. Pediatr Int 2012; 54: 532-5.
4) Andreoli SM, Kofmehl E, Sobol SE. Is inpatient admission necessary following removal of airway foreign bodies? Int J Pediatr Otorhinolaryngol 2015; 79: 1436-8.
5) Rizk N, Gwely NE, Biron VL, and Hamza U. Metallic hairpin inhalation: a healthcare problem facing young Muslim females. J Otolaryngol Head Neck Surg 2014; 2; 43:21.
6) Pellissier A, Kebdani S, Lacheheb M, Lainez S, Froudarakis ME, Vergnon JM. 41 Years into the bronchial tree: a very obstructive cap. Clin Resp J 2017; 11: 1060-2.
7) Divarci E, Toker B, Dokumcu Z, Musayev A, Ozcan C, Erdener A. The multivariate analysis of indications of rigid bronchoscopy in suspected foreign body aspiration. Int J Pediatr Otorhinolarynol 2017; 100: 232-7.
8) Şahin E, Karadayı Ş, Kaptanoğlu M. Trakeobronşiyal yabancı cisimler. Turkiye Klinikleri J Thor Surg-Special Topics 2009; 2: 32-7.
9) Karadayı Ş, Kaptanoğlu M. Bölüm 60: Yabancı cisim aspirasyonu. Ökten İ, Kavukçu HŞ, editörler. Göğüs Cerrahisi. 2. Baskı İstanbul: Medikal Sağlık ve Yayıncılık Hiz. Tic. Ltd. Şti; 2013. p. 859-64.
10) Bodart E, Gilbert A, Thimmesch M. Removal of an unusual bronchial foreign body: rigid or flexible bronchoscopy? Acta Clinic Belg 2014; 69: 125-6.
11) Singh JK, Vasudevan V, Bharadwaj N, Narasimhan KL. Role of tracheostomy in the management of foreign body airway obstruction in children. Singapore Med J 2009; 50: 871-4.
12) Soysal O, Kuzucu A, Ulutas H. Tracheobronchial foreign body aspiration: a continuing challenge. Otolaryngol Head Neck Surg 2006; 135: 223-6.
13) Fenane H, Bouchikh M, Bouti K, El Maidi M, Ouchen F, Mbola TO et al. Scarf pin inhalation: clinical characteristics and surgical treatment. J Cardiothorac Surg 2015; 10: 61.
14) Pazarlı CA, Havan AG. Fıstık her zaman lezzetli olmayabilir: ilginç bir aspirasyon. Turk Toraks Derg 2014; 15: 68-70.
15) Yıldırım M, Doğusoy I, Okay T, Yaşaroğlu M, Demirbag H, Aydemir B et al. Tracheobronchıal Foreıgn Bodıes. Turk Gogus Kalp Dama 2003; 11: 228-31.
16) Ludemann JP, Hughes CA, Holinger LD. Management of foreign bodies of the airway. In: Shields TW, LoCicero J, Ponn RB, eds. General Thoracic Surgery. Philadelphia: WB Saunders, 2000; 73: 853-62.
17) Carluccio F, Romeo R. Inhalation of foreign bodies: Epideniological data and clinical considerations in the light of a statistical review of 92 cases. Acta Otorhinolaryngol Ital 1997; 17: 45-51.
18) İlhan H. Çocuklarda yabancı cisim aspirasyonları. Çocuk Cerrahisi Dergisi 2017; 31: 40-5.






