2Department of Cardiovascular Surgery, Hacettepe University School of Medicine, Ankara, Turkey DOI : 10.26663/cts.2019.00018
Summary
Dental extraction is a frequently performed procedure in daily routine. Although this procedure is associated with a low complication rate, it has the potential to cause lethal complications such as head and neck emphysema, pneumomediastinum, pharyngeal abscess, septic thrombophlebitis of internal jugular vein, descending necrotizing mediastinitis, peribronchovascular inflammation of the lung parenchyma, and septicaemia. Conservative management is sufficient in majority of patients with emphysema and/or pneumomediastinum. However, treatment of pharyngeal abscess, mediastinitis and mediastinal abscess cannot be achieved with solely antibiotic administration and surgical drainage is necessary in most of the cases. In this report, we present three cases; two cases of pneumomediastinum and one case with severe deep neck inflammation, thrombophlebitis of jugular vein, mediastinitis and empyema occurred following molar tooth extraction by using air-tribune drills. Two cases without infectious complications were treated conservatively while the other patient was treated surgically. Complete resolution was achieved in all patients during follow-up.Introduction
Dental extraction is a frequent procedure that has the potential to cause lethal complications if not performed under appropriate conditions. Complications encountered after dental extraction range in a variety of disorders including head and neck emphysema, pneumomediastinum, pharyngeal abscess, septic thrombophlebitis of internal jugular vein, mediastinitis and mediastinal abscess, peribronchovascular inflammation in the lung parenchyma, and septicemia [1-4]. Pneumomediastinum, which is defined as entrapment of free air in the mediastinal space, was first described by Laënnec in 1819 [5]. The occurrence of pneumomediastinum and subcutaneous emphysema due to dental treatments is very rare. The usage of high-speed air-tribune drills can lead to the introduction of air into soft tissues and has been reported as the most common cause of this complication [6-8]. Oral flora may also spread to the neck through the cervical fascia and cause deep neck infection or descending necrotizing mediastinitis (DNM) [3,9]. Herein, we report two cases of pneumomediastinum and one case with severe deep neck inflammation, thrombophlebitis of jugular vein, mediastinitis and empyema occurred following molar tooth extraction by using air-tribune drills.Case Presentation
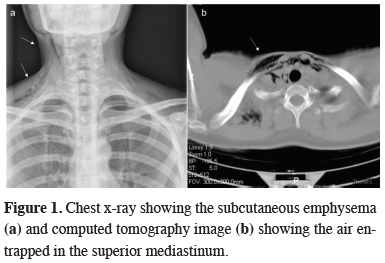
Case 1:A 30-year-old woman was admitted to our emergency department with a swollen neck, 2 h after she had undergone root canal restoration of the third right mandibular molar with an air-tribune drill, which inflates air in the root canal. Her physical examination revealed neck swelling with crepitation on both sides. Chest x-ray showed subcutaneous emphysema of the laterocervical and presternal regions (arrows) (Figure 1a). Computed tomography (CT) of the neck and chest demonstrated air entrapment at the submaxillary and retromandibular spaces, extending through superior mediastinum (arrows) (Figure 1b).
 Click Here to Zoom |
Figure 1: Chest x-ray showing the subcutaneous emphysema (a) and computed tomography image (b) showing the air entrapped in the superior mediastinum. |
Prophylactic antibiotic and analgesia were administered. The patient had an uneventful recovery and was discharged after 4 days without any sequelae.
Case 2:
A 31-year-old woman presented in our emergency department with mild dyspnea and right-sided neck swelling, 4 h after right third molar surgical extraction. A high-speed air turbine drill was used during the procedure. Physical examination showed right-sided facial and neck swelling and crepitation on palpation. All vital signs were stable. CT of the neck and thorax demonstrated air in the subcutaneous and visceral spaces in the right mandibular area, spreading through right maxillary sinus to orbital region and superior mediastinum (arrows) (Figure 2).
 Click Here to Zoom |
Figure 2: CT image showing air entrapped in the superior mediastinum. |
The patient was admitted to the Thoracic Surgery Department unit for spontaneous air resorption. Antibiotic prophylaxis with amoxicillin-clavulanic acid was administered. She had an uneventful recovery and was discharged after 3 days. She attended a follow-up visit in two weeks later, confirming complete resolution of the process.
Case 3:
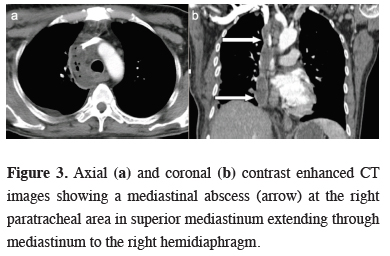
A 54-year-old male patient was admitted to our emergency department three days after molar teeth extraction. He had fever, limited mouth and neck movements, neck swelling, shortness of breath and difficulty swallowing. Physical examination revealed poor oral hygiene, swelling, redness and crepitation in the right supraclavicular region. He also had a history of diabetes mellitus. CT examination demonstrated subcutaneous emphysema in right submandibular and submental regions and inflammatory stranding in fat tissues of deep neck region and superior mediastinum suggesting deep neck infection spreading to mediastinum. Management of the patient was discussed with the ENT (Ear, nose, throat) surgeons. Medical treatment with antibiotherapy and early follow-up CT was planned. Fourth day follow-up CT revealed increased severity and extension of inflammation and additional submandibular abscess, thrombophlebitis of right internal jugular vein, mediastinitis, mediastinal abscess, peribronchovascular thickening in right parahilar region and right-sided empyema (Figure 3).
 Click Here to Zoom |
Figure 3: Axial (a) and coronal (b) contrast enhanced CT images showing a mediastinal abscess (arrow) at the right paratracheal area in superior mediastinum extending through mediastinum to the right hemidiaphragm. |
Blood culture yielded Streptococcus anginosus. Surgical intervention was planned as interventional drainage was not considered by the Interventional Radiology Department. Single-port Video Assisted-Thoracoscopic Surgery (VATS) was performed. Cervical mediastinal pleura was swollen and edematous. Cervical mediastinal pleura was opened from the uppermost level of the swollen tissue and the abscess was drained. There was no purulent drainage from the chest tube during the post-operative period. Follow-up CT imaging showed shrinkage of the neck abscess and mediastinal infection with persistence of the right internal jugular vein thrombophlebitis. The post-operative course of the patient was uneventful. The patient was symptom free at 1st month follow-up.
Discussion
The appearance of subcutaneous emphysema and pneumomediastinum can be secondary to trauma, infections, maxillofacial operations, and dental surgery. In general, the condition is self-limiting and not life threatening, but rarely it can progress to tension pneumothorax, mediastinitis or gas embolism [6,10]. The use of high-speed dental air turbine drills can lead to the introduction of air or water into soft tissue spaces through the dentoalveolar membrane in the root canal. Third molar tooth extraction in which the tooth was sectioned using an air- turbine drill was observed as the most frequent cause, which was also seen in our second case [8,11]. Occasionally, it may also arise during restorative treatment, root canal treatment, periodontic surgery, scaling, laser irradiation, and even flashing of the air syringe, as seen in case one [12].Fascial spaces around the cervical fascias are not real spaces. They contain small amounts of loose connective tissues. During dental procedures, compressed air may enter from the tooth roots to the submandibular space and dissects through the cervical fascial planes and gradually extends between these spaces. After accessing to lateral pharyngeal and retropharyngeal spaces, air can easily spread to the mediastinal cavity. Thus, these spaces should be considered as potential pathways for the spread of air, fluid and any microorganism [8,13,14]. The cause of infections is oral flora containing both aerobic and anaerobic microorganisms, which may cause life-threatening complications in the setting of immunosuppression. The presence of diabetes mellitus in our patient may be an underlying cause for spreading of infection along the neck and mediastinal soft tissues resulting in DNM [15]. Although we consider administering immediate prophylactic antibiotherapy to all patients to avoid any potential infectious complication, we were unable to prevent occurrence of DNM in one of our patients.
Most common signs and symptoms of subcutaneous emphysema are swelling, dysphagia, chest pain, dyspnea and crepitus. Fever and redness are additional symptoms of a potential infection. These symptoms may occur immediately, within few hours or days following the procedure [6,7]. Two patients typically described swelling within few hours after dental procedures.
Imaging plays a crucial role in diagnosis of mediastinal complications caused by dental procedures. Chest x-rays demonstrate widened mediastinum with or without evidence of a pleural effusion in the setting of DNM. CT scan of the neck and thorax usually provide correct diagnosis and reveal mediastinal complications. Cervicothoracic CT can reveal gas and pus collections extending along the cervicothoracic fascia with accompanying abscesses. In all our patients definitive diagnosis was achieved by CT imaging. The differential diagnosis includes cellulitis, hematoma, angioedema, and allergic reaction [16].
Treatment strategy depends on the severity of the condition. Mostly, pneumomediastinum resolve after 3 to 5 days of supportive treatment without any consequences. Antibiotic prophylaxis is indicated, particularly in the presence of underlying respiratory diseases or dental infections. Surgical decompression could only be necessary in the presence of complications such as compression of the thoracic outlet, airflow obstruction, and respiratory failure. However, treatment of DNM and mediastinal abscess cannot be achieved with solely antibiotic administration. Interventional drainage of the mediastinal abscess is necessary in most of the cases for recovery [6,16]. In our 3rd case, interventional drainage of the mediastinum was not considered and surgery remained the optimal option.
In conclusion, dental procedures can cause mediastinal complications. Although pneumomediastinum manifests as a self-limiting condition descending of the oral flora into the mediastinum across the cervical fascial planes and spaces may cause life-threatening complications including deep neck infection, neck abscesses, DNM, mediastinal abscess and empyema. Thus, the use of compressed air could be avoided in dental practice and emergency department physicians should consider these complications when a patient experience with dyspnea, subcutaneous emphysema, fever, neck swelling and/or redness, and chest pain after a dental procedure.
Declaration of conflicting interests
The authors declared no conflicts of interest with respect to the authorship and/or publication of this article.
Funding
The authors received no financial support.
Reference
1) Tan S, Nikolarakos D. Subcutaneous emphysema secondary to dental extraction: A case report. Aust Dent J 2017; 62: 95-7.
2) Arai I, Aoki T, Yamazaki H, Ota Y, Kaneko A. Pneumomediastinum and subcutaneous emphysema after dental extraction detected incidentally by regular medical checkup: a case report. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2009; 107: 33-8.
3) Fukuchi M, Suzuki O, Nasu D, Koizumi K, Muta Y. Descending Necrotizing Mediastinitis Treated with Tooth Extractions following Mediastinal and Cervical Drainage. Case Rep Gastroenterol 2015; 9: 311-6.
4) Ghaly B, Bertram A, Naim A. Lemierre’s syndrome: a serious complication of a routine dental procedure. Aust Dent J 2013; 58: 246-9.
5) Peker RO, Sabuncu T, Alpat S, Pasaoglu I. Two unusual causes of a rare clinical entity: pneumomediastinum. Turk Gogus Kalp Damar 2015; 23: 359-60.
6) Aslaner MA, Kasap GN, Demir C, Akkas M, Aksu NM. Occurrence of pneumomediastinum due to dental procedures. The American Journal of Emergency Medicine 2015; 33: 125.e1-125.e3.
7) Kim Y, Kim MR, Kim SJ. Iatrogenic pneumomediastinum with extensive subcutaneous emphysema after endodontic treatment: report of 2 cases. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2010; 109: 114-9.
8) McKenzie WS, Rosenberg M. Iatrogenic subcutaneous emphysema of dental and surgical origin: a literature review. J Oral Maxillofac Surg 2009; 67: 1265-8.
9) Makeieff M, Gresillon N, Berthet JP, Garrel R, Crampette L, Marty-Ane C, et al. Management of descending necrotizing mediastinitis. Laryngoscope 2004; 114: 772-5.
10) Johannesma PC, Vonk Noordegraaf A. Pneumomediastinum and Pneumopericardium Due to High-Speed Air Turbine Drill Used During a Dental Procedure. Ann Thorac Surg 2014; 98: 2232.
11) Yang S.C, Chiu TH, Lin TJ, Chan HM. Subcutaneous emphysema and pneumomediastinum secondary to dental extraction: a case report and literature review. Kaohsiung J Med Sci 2006; 22: 641-5.
12) Durukan P, Salt O, Ozkan S, Durukan B, Kavalci C. Cervicofacial emphysema and pneumomediastinum after a high-speed air drill endodontic treatment procedure. Am J Emerg Med 2012; 30: 2095 e3-6.
13) Dongel I, Bayram M, Uysal IU, Sunam GS. Subcutaneous emphysema and pneumomediastinum complicating a dental procedure. Ulus Travma Acil Cerrahi Derg 2012; 18: 361-3.
14) Kost M. Thoracic complications associated with utilization of the air turbine dental drill. AANA J 1996, 64: 288-92.






