

2Department of Thoracic Surgery, Dr. Suat Seren Chest Diseases and Thoracic Surgery Training Hospital, İzmir, Turkey
3Deparment of Pathology, Dr. Suat Seren Chest Diseases and Thoracic Surgery Training Hospital, İzmir, Turkey DOI : 10.26663/cts.2019.00124
Summary
Background: Until the reclassification by the International Association for the Study of Lung Cancer, the term bronchoalveolar carcinoma (BAC) has been used for many years. Accordingly, the terms BAC and mixed adenocarcinoma were replaced by the terms such as adenocarcinoma in situ, minimally invasive adenocarcinoma, lepidic dominant type adenocarcinoma, mucinous minimally invasive adenocarcinoma, and mucinous invasive adenocarcinoma. The aim of this study was to retrospectively evaluate the cases diagnosed as BAC and mixed type adenocarcinoma operated in our clinic and to compare the clinical and survival characteristics of these cases according to the new classification.Materials and Methods: 37 patients who were operated in our clinic between January 2005 and December 2014 and diagnosed as BAC and mixed adenocarcinoma containing BAC components were included in the study. Pathologic slides were re-reviewed by the pathologists of our hospital and reclassified according to the predominant histologic subtype. In addition to the predominant cell type, the ratio of other cell types were also specified in 5% ratio slices.
Results: The histopathological diagnoses of 37 formerly BAC patients, 14 of whom were mixed type, were changed as 33 lepidic, two mucinous, one adenocarcinoma in situ and one micro-invasive adenocarcinoma. The 5-year survival rate for lepidic predominant histological subtype was 70.3, while it was 50% (p = 0.533) for the two mucinous cases.
Conclusions: The predominant cell type distribution used in the new classification of IASLC is more effective in determining survival and is more suitable for use in treatment and follow-up programs.
Introduction
The term bronchoalveolar carcinoma (BAC) was first used by Avril Liebow as in the diagnostic sense in 1960 [1]. This term had served as a subtype of lung adenocarcinoma for decades to the thoracic oncology. However, in 2011, the International Association for the Study of Lung Cancer (IASLC) proposed a new classification of adenocarcinoma and argued that the terms “BAC” and “mixed type adenocarcinoma”, which included bronchoalveolar pattern, should not be used anymore due to their broad spectrum [2]. The World Health Organization’s new lung cancer classification published in 2015 also included the majority of these proposed changes [3]. Accordingly, the terms BAC and mixed adenocarcinoma were replaced by the terms such as adenocarcinoma in situ, minimally invasive adenocarcinoma, lepidic dominant type adenocarcinoma, mucinous minimally invasive adenocarcinoma, and mucinous invasive adenocarcinoma (Table 1). The aim of this study was to retrospectively evaluate the cases diagnosed as BAC and mixed type adenocarcinoma operated in our clinic and to compare the clinical and survival characteristics of these cases according to the new classification.Table 1: Categories of new adenocarcinoma classification.
Methods
37 patients who were operated in our clinic between January 2005 and December 2014 and diagnosed as BAC and mix adenocarcinoma containing BAC components were included in the study.Pathologic slides were re-reviewed by the pathologists of our hospital and re-classified according to the predominant histologic subtype as defined by IASLC/ATS/ERS classification, and recently 2015 WHO classification. In addition to the predominant cell type, the ratio of other cell types were also specified in 5% ratio slices.
Patients were excluded if they had an incomplete resection, metastatic disease or nodule found at the time of surgery.
Before 2010, all patients were evaluated with contrast-enhanced chest computed tomography, and after 2010, PET-CT was added due to its ability to detect unknown metastases. Patients without enlarged lymph nodes and with a PET-negative mediastinum proceeded directly to the surgery. However, patients with enlarged lymph nodes on CT, independently from PET findings, underwent EBUS-TBNA and/or mediastinoscopy. All pathological N2 cases received adjuvant chemotherapy and/or radiotherapy.
From years 2005 to 2010, serratus anterior muscle-sparing thoracotomy was performed in all patients. Since year 2010, almost 25% of patients underwent video-assisted thoracoscopic surgery (VATS).
Medical records of 37 patients were reviewed for clinicopathologic information, including age, gender, smoking history, comorbidity, histologic subtype and, pathologic tumor-node-metastasis (TNM) stage according to the 8th edition of the lung cancer staging system. Patients were followed up at 3-month intervals for the first 2 years and at 6-month intervals thereafter. The date of death was found from the medical records and verified by a software program, linked to the national population registration system.
The study protocol was approved by the local Institutional Review Board (Approval no: 2018/49109414-806.02.02).
Statistical Analysis
Statistical evaluation was performed with IBM SPSS version 21.0 software (IBM Corp., Armonk, NY, USA). Patient survival was expressed by actuarial analysis according to the method of Kaplan Meier, and differences in survival were determined using the log-rank test in the univariate analysis. A multivariate analysis of variables was performed using the Cox proportional odds regression model. For all analyses, p < 0.05 was considered as statistically significant.
Results
The mean age of 37 patients, as 25 male and 12 female, was found to be 61.9 (std: 10.0, range: 29-76). The 5-year survival rate was 71.0%, the mean expected survival was 92.5 months (std: 8.4, 76.1-108.8). There was no 30-day mortality.
Survival Analysis
The overall 5-year survival of 37 patients was found to be 71.0%. The number of cases in stages I, II and III were 23 (62.2%), 9 (24.3%), and 5 (13.5%), respectively. 5-year survival in stages I, II, and III were found 76.7%, 87.5%, and 0.0%, respectively. The survival in stage III was significantly worse compared to stage I and stage II (p = 0.001, p = 0.007, respectively).
The diagnoses of a total of 37 patients, 14 of whom were mixed type, with BAC according to the former classification in our study group, were re-classified as 33 lepidic (89.2%), two mucinous (5.4%), one adenocarcinoma in situ (AIC) and one micro-invasive adenocarcinoma (MIC) according to the new classification of 2015 WHO lung cancer classification. The 5-year survival rate for lepidic predominant histological subtype was 70.3%, while for the two mucinous cases, it was 50% (p = 0.533). The other two patients are still under follow-up.
According to the T factor, 40.6% of the patients (n = 15) had T1, 32.4% (n = 12) had T2, 16.2% (n = 6) had T3 and 10.8% (n = 4) had T4; and 5-year survival was 85.1%, 64.2%, 83.3%, and 0.0%, respectively. There was a significant difference in 5-year survival between only T1 and T4 (p = 0.004).
N involvement was present in three patients (8.1%), as one N2 and two N1. The 5-year survival was 75.1% in patients with N0, while in patients with N positivity, it was 0.0% (p < 0.001). The mean lepidic pattern rate of 33 lepidic predominant patients was 63.3% (range: 40-90) and the median value was 60%. The 5-year survival rate of patients with a lepidic pattern rate of 60% or above was significantly better than those who had below 60% (81.4%, 50.0%, respectively, p = 0.003). In addition, 21 (59.5%) patients had solid components (mean 22.1%, median 20%). The 5-year survival of six patients with a solid component rate below 20% was better than the rest, but it was not statistically significant (60.0%, 50.6% respectively, p = 0.183).
Pleural invasion was present in three patients (8.1%). The 5-year survival of these patients was 66.7%, but there was no significant difference between the other patients (p = 0.379).
Mean clinical follow-up period was 67.5 months (std: 38.9, range: 8-132 months). The last follow-up time was 01.01.2017.
Clinical characteristics and survival of patients are shown in table 2.
Table 2: Clinic characteristics and survival of patients.
Discussion
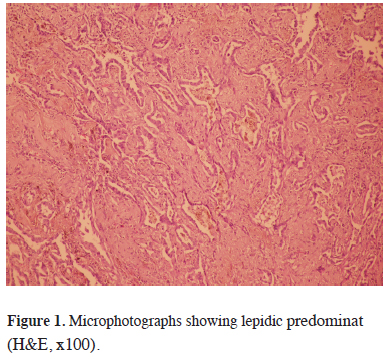
BAC as a pathological diagnosis describes the spread of adenocarcinoma alongside the alveolar wall. However, this term has now been replaced by a new classification because it is used in a wide range of heterogeneous tumor groups ranging from in situ tumors to invasive carcinomas [4]. In our study, patients with a diagnosis of BAC were re-classified as 33 lepidic, two mucinous and a micro-invasive adenocarcinoma and an adenocarcinoma in situ.The “lepidic” term is defined as tumor cell growth evenly across pre-existing alveolar structures without involving the papillary or micropapillary structures. Lepidic growth is usually accompanied by thickened alveolar walls, but typically there is no inflammation. In addition, there is no stromal, vascular or pleural invasion [5] (Figure 1).
 Click Here to Zoom |
Figure 1: Microphotographs showing lepidic predominat (H&E, x100). |
An absolute consensus exists in which lepidic predominant subtype has a better prognosis than other subtypes [5-9]. In our patient group, 5-year survival was 70.3% in lepidic pattern predominant patients, consistent with the literature. Moreover, as many publications in the literature indicate that patients with adenocarcinoma have a better prognosis as the rate of lepidic pattern increases [6,10]. In addition, the higher the rate of lepidic pattern, the lower the possibility of recurrence reported [11]. In our study, mean lepidic pattern rate was found to be 63.2% (std: 17.6, range: 40-100), and the median was 60% in all patients. The cases whose lepidic pattern rate was above 60% had better survival than others (p = 0.009). Anami et al. reported that the lepidic component is a more useful prognostic marker than lymph node metastasis [7]. In our patient group, only three patients had lymph node positivity and 2 of them had lepidic and one had a mucinous pattern. Of course, the number is insufficient to reach a conclusion.
Mucinous adenocarcinoma is characterized by tumor cells having goblet cell with abundant intracytoplasmic mucin or columnar cell morphological pattern histopathologically [12]. The prognosis of invasive mucinous adenocarcinoma among invasive adenocarcinomas in the new classification is still controversial. Even though there are studies reporting that mucinous adenocarcinomas are associated with poor prognosis in the literature [8,13], there are also reports that mucinous adenocarcinomas have a better prognosis than nonmucinous adenocarcinomas [14]. All these different results are thought to be due to the fact that mucinous adenocarcinomas constitute only 2-5% of all lung cancers and therefore the number of patients in the studies is low. As in our patient group, the diagnosis of mucinous adenocarcinoma was determined in only two (5.4%) patients.
In conclusion, the predominant cell type distribution used in the new classification of IASLC is more effective in determining survival and is more suitable for use in treatment and follow-up programs.
Declaration of conflicting interests
The authors declared no conflicts of interest with respect to the authorship and/or publication of this article.
Funding
The authors received no financial support for the research and/or authorship of this article.
Reference
1) Leibow AA. Bronchiolo-alveolar carcinoma. Adv Intern Med 1960; 10: 329-58.
2) Travis WD, Brambilla E, Noguchi M, Nicholson AG, Geisinger KR, Yatabe Y, et al. International association for the study of lung cancer/american thoracic society/european respiratory society international multidisciplinary classification of lung adenocarcinoma. J Thorac Oncol 2016; 6: 244-85.
3) Travis WD, Brambilla E, Nicholson AG, Yatabe Y, Austin JH, Beasley MB, et al. The 2015 World Health Organization classification of lung tumors: impact of genetic, clinical and radiologic advances since the 2004 classification. J Thorac Oncol 2015; 10: 1243-60.
4) Xu L, Tavora F, Battafarano R, Burke A. Adenocarcinomas with prominent lepidic spread: retrospective review applying new classification of the American Thoracic Society. Am J Surg Pathol 2012; 36: 273-82.
5) Weichert W, Warth A. Early lung cancer with lepidic pattern: adenocarcinoma in situ, minimally invasive adenocarcinoma, and lepidic predominant adenocarcinoma. Curr Opin Pulm Med 2014; 20: 309-16.
6) Strand TE, Rostad H, Strøm EH, Hasleton P. The percentage of lepidic growth is an independent prognostic factor in invasive adenocarcinoma of the lung. Diag pathol 2015; 10: 94.
7) Anami Y, Iijima T, Suzuki K, Yokota J, Minami Y, Kobayashi H, et al. Bronchioloalveolar carcinoma (lepidic growth) component is a more useful prognostic factor than lymph node metastasis. J Thorac Oncol 2009; 4: 951-8.
8) Russell PA, Wainer Z, Wright GM, Daniels M, Conron M, Williams RA. Does lung adenocarcinoma subtype predict patient survival?: A clinicopathologic study based on the new International Association for the Study of Lung Cancer/American Thoracic Society/European Respiratory Society international multidisciplinary lung adenocarcinoma classification. J Thorac Oncol 2011; 6: 1496-504.
9) Hung JJ, Yeh YC, Jeng WJ, Wu KJ, Huang BS, Wu YC, et al. Predictive Value of the International Association for the Study of Lung Cancer/American Thoracic Society/European Respiratory Society Classification of Lung Adenocarcinoma in Tumor Recurrence and Patient Survival. J Clin Oncol 2014; 32: 2357-64.
10) Lin D, Ma Y, Zheng S, Liu X, Zou S, Wei W. Prognostic value of bronchioloalveolar carcinoma component in lung adenocarcinoma. Histol Histopathol 2006; 21: 627.
11) Kadota K, Villena-Vargas J, Yoshizawa A, Motoi N, Sima CS, Riely GJ, et al. Prognostic significance of adenocarcinoma in situ, minimally invasive adenocarcinoma, and nonmucinous lepidic predominant invasive adenocarcinoma of the lung in patients with stage I disease. Am J Surg Pathol 2014; 38: 448.
12) Lee HY, Cha MJ, Lee KS, Lee HY, Kwon OJ, Choi JY, et al. Prognosis in resected invasive mucinous adenocarcinomas of the lung: related factors and comparison with resected nonmucinous adenocarcinomas. J Thorac Oncol 2016; 11: 1064-73.



