Summary
Background: In this study, we reviewed the treatment, follow-up, and prognostic factors associated with complications in patients who underwent tracheal resection due to postintubation tracheal stenosis (PETS), in light of the literature.Materials and Methods: Twenty-five patients who were operated for PETS between June 2012 and June 2017 were retrospectively evaluated. The patients’ postoperative complications and prognostic factors affecting mortality were examined.
Results: There was 11 female (44%) and 14 male (56%) patients. Eight patients (32%) had comorbidities. The mean prolonged intubation time was 47.4 ± 55.0 minutes. Eight patients (32%) developed postoperative morbidity. The main prognostic factors associated with morbidity were the length of the stenotic area and the presence of endocrine and respiratory comorbidities (p<0.05). Tracheal fistulae were observed in 2 patients. The postoperative mortality rate was 8% (n=2). One patient with fistula died on postoperative day 2, while another patient died at postoperative three months due to cardiac failure. No significant factor was identified in relation to the development of tracheal fistulae.
Conclusions:The most important factor associated with complications was the presence of endocrine comorbidities. Although tracheal surgery results in high rates of postoperative morbidity and mortality, we believe these risks can be reduced by experienced surgeons and appropriate patient selection.
Introduction
In addition to surgical treatment for postintubation tracheal stenosis (PETS), methods such as bronchoscopic dilatation, laser ablation, and stent placement are also available. Reports have indicated that bronchoscopy can be curative in many selected cases [1-3]. Mehta et al. reported that diaphragm- or web-like stenoses could be treated by mucosal separation technique with a success rate of 60% after 1–3 sessions [4]. However, mechanical dilation alone in cases of long or inoperable stenoses leads to more than 90% recurrence [1].To date, there have been few publications regarding tracheal resection due to PETS. In particular, there is not enough literature on this subject in Turkey. There have also been very few studies investigating the prognostic factors associated with anastomotic complications.
In this study, we review the treatment options, follow-up, and prognostic factors that may lead to complications in patients who undergo tracheal resection due to PETS, in light of the literature.
Methods
Data pertaining to patients operated for PETS between June 2012 and June 2017 were retrospectively evaluated from a routine patient database. Twenty-six PETS patients were initially evaluated for the study. One patient was excluded due to a lack of follow-up. The study included 25 patients, 11 females (44%) and 14 males (56%), who underwent tracheal resection and end-to-end anastomosis due to PETS. This study was approved by the institutional review board of İstanbul Education and Research Hospital (2017/1035) and was conducted in accordance with the principles of the Declaration of Helsinki.
Preoperative Evaluation
Fiberoptic bronchoscopy was performed on each patient to determine the location and size of the tracheal lesion. Rigid bronchoscopy was performed to perform dilation in patients with severe respiratory distress. In addition to bronchoscopy, cervical computed tomography was used on all patients to determine the location of the lesion and the relationship of the trachea with adjacent structures. An esophagography was requested in addition to bronchoscopy from one patient because they had a tracheoesophageal fistula in addition to tracheal stenosis.
Preoperative comorbidities were classified into three groups: endocrine diseases (diabetes), cardiac problems (hypertension, heart failure, and coronary artery disease), and respiratory conditions (asthma and chronic obstructive lung disease).
Surgical Technique
All patients were evaluated on the operating table by rigid bronchoscopy. To mark the proximal edge of the stenosis, the anterior trachea was pierced with a sterile needle as the patient lay in a supine position. The patients were intubated with a spiral intubation tube (number 6-7) based on stenosis severity. Patients with stenoses too narrow to be intubated underwent dilatation with rigid bronchoscopy on the operating table before intubation.
Operations were performed using the technique described by Pearson and Grillo [5,6]. The neck was positioned in hyperextension, and a collar incision was made. The trachea was freed from the surrounding tissues while preserving the vascular supply and avoiding unnecessary dissection proximal and distal to the stenosis as much as possible.
Healthy tissue was cut horizontally from the inferior lesion margin. A sling suture with 2/0 polyglactin was placed in the distal trachea to prevent the trachea from moving distally when the horizontal incision was made. In general, horizontal incisions were made more proximally and even in the middle of the stenotic segment instead of at the far distal aspect of the lesion. Thus, the proximal and distal borders of the stenosis were also visible from within the lumen. Therefore, the stenotic segment was usually sent for pathological examination as two pieces, the distal and proximal portions. The intubation tube was removed proximally. It was noted that in cases of subglottic and proximal tracheal stenoses, the intubation tube moved proximally to the vocal cords during retraction, which made it difficult to reposition the intubation tube distally during anastomosis. To prevent this, a fixation stitch with 0 silk suture was placed at the end of the intubation tube. This allowed the tube to be positioned by pulling distally instead of pushing through the mouth. The distal trachea was intubated with a second spiral tube that was connected to a ventilator via a sterile circuit brought into the surgical field.
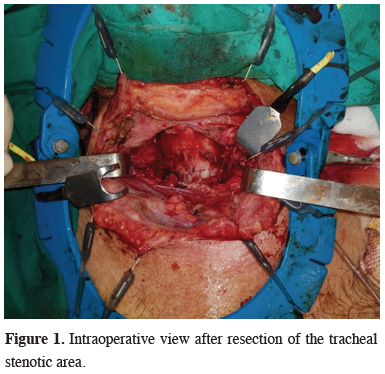
The stenotic area was removed by circular resection at the upper and lower borders of the lesion (Figure 1).
 Click Here to Zoom |
Figure 1: Intraoperative view after resection of the tracheal stenotic area. |
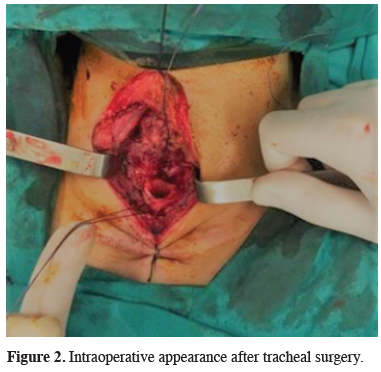
Support sutures with 2-0 polyglactin were placed at the upper and lower ends of the trachea. The anastomosis was started from the posterior wall. The anastomosis of the posterior membranous wall was completed with interrupted or continuous stitches with 3-0 or 4-0 polyglactin or polydioxanone (PDS) suture. The anterior and lateral walls were also anastomosed with 3-0 or 4-0 polyglactin, or PDS interrupted sutures (Figure ffigure2>2). Two jaw sutures were placed to prevent postoperative neck extension. These sutures were removed on postoperative day 7.
 Click Here to Zoom |
Figure 2: Intraoperative appearance after tracheal surgery. |
Postoperative Follow-up
Postoperative morbidities were evaluated as complications that occurred in a hospital or during the first 30 days. Postoperative fistulae, hoarseness, superficial surgical site infections, deep surgical site infections, and hemorrhages were accepted as morbidities. Postoperative mortality was defined as deaths that occurred in a hospital or during the first 30 days.
Statistical Analysis
Statistical analysis of the study was performed with SPSS version 22 (Statistical Program for Social Sciences) software package. Descriptive statistics pertaining to categorical variables were expressed as frequencies and percentages, while those of continuous variables were expressed as mean, standard deviation, median, and minimum and maximum values. The Mann–Whitney U test was used to compare means between groups, and the chi-square test was used for comparisons of categorical variables. For all statistical comparisons, p values below 0.05 were considered statistically significant.
Results
Of the 25 patients included in the study, 14 were male, and 11 were female. Their mean age was 41.7 ± 16.81 (17-76) years. Comorbidities were present in 8 (32%) of the patients. The patients’ demographic characteristics are shown in Table 1. PETS developed postoperatively in 11 patients (44%), due to respiratory arrest in 5 patients (20%), due to cardiac arrest in 4 patients (16%), and due to prolonged intubation for neurological reasons in 5 patients (20%). The mean prolonged intubation time was 47.4 ± 55.0 hours.Table 1: Demographic characteristics of the patients.
Eight patients had a history of tracheostomy due to prolonged intubation. Three patients had tracheostomy at the time of surgery, while five patients had surgical scars from the previous tracheostomy. The average time to onset of postintubation symptoms in our patients was 12 months. All of the patients complained of dyspnea. Bronchoscopic examinations revealed that the distance between the level of stenosis and the vocal cords ranged from 1 to 4 cm. In one patient, the stenosis was 1.5 cm proximal to the tracheal carina. Twenty-four patients underwent a collar incision, while the patient with stenosis proximal to the tracheal carina underwent thoracotomy. The mean resection length was 3.19 cm. Resection length was 2.4-3 cm in 10 patients, 3-4 cm in 12 patients, and 4 cm or longer in 3 patients. The mean length of tracheal stenosis was 3.2 ± 0.67 cm.
Fifteen patients (60%) underwent a mean of 1.60 ± 0.73 (1-3) preoperative dilatations. Three patients (12%) who had surgery for PETS at another center were reoperated due to restenosis. Of these three patients, one had undergone laryngeal release in the previous surgery. This patient had a stenotic segment of 4.5 cm, and resection of 5.5 cm was performed. In another patient, esophagoscopic and bronchoscopic examination confirmed the persistence of the tracheal stenosis and tracheoesophageal fistula for which they underwent surgery previously. Simultaneous tracheal resection and tracheoesophageal fistula repair were performed. The third patient was reoperated due to the development of granulation tissue on the anastomosis made 3 cm from the vocal cords.
A total of 8 patients (32%) developed morbidities: tracheal fistulae in 3 patients (12%), hoarseness in 6 patients (24%), hemorrhage in 4 patients, deep surgical site infections in 3 patients, and superficial surgical site infections in 3 patients. Emergency tracheostomy was performed due to respiratory failure in 1 patient who developed hemorrhage. One patient underwent emergency tracheostomy in the early postoperative period due to bilateral recurrent damage. Complications occurred in 2 (66.6%) of the three patients who underwent repeat tracheal resection and in 6 (27.3%) of the 22 patients who were operated for the first time (p = 0.231). Factors associated with postoperative morbidity were having diabetes or respiratory problems as comorbidity. Prognostic factors associated with complications are shown in Table 2.
Table 2: Evaluation of factors associated with morbidity.
Two patients with tracheal fistulae underwent a permanent tracheostomy. Fistula-related mortality occurred in 1 patient. No factor was statistically associated with the formation of tracheal fistulae in the study (Table 3). Polyglactin and PDS sutures were used in all patients in this study. For the membranous part, polyglactin was used in 3 patients (12%), while PDS was used in 88%. For anterior wall anastomosis, polyglactin was used in 8 patients (32%), and PDS was used in 17 (68%). In terms of anastomosis technique, interrupted sutures were used in the anterior wall in all patients. In the membranous wall, interrupted sutures were used in 9 patients and continuous sutures in 16 patients.
Table 3: Prognostic factors of tracheal fistula.
Postoperative recurrence occurred in 3 patients. Two patients developed granulation tissue at the anastomosis site after two months and 18 months, and the stenosis was resolved with cryotherapy. Emergency tracheostomy was performed on one patient who presented with dyspnea at three months.
The postoperative mortality rate was 8% (n=2). One patient with fistula died on postoperative day 2, while another patient died due to cardiac failure at postoperative three months.
Discussion
Prolonged intubation may result in stenosis at different levels of the trachea. Stenosis can occur anywhere in the glottic and subglottic areas, depending on the level of the endotracheal intubation tube. It occurs most commonly where the endotracheal tube cuff comes into contact with the tracheal wall [7,8]. PETS is seen in 0.1-20% of patients with chronic intubation [9]. A much smaller proportion of these becomes clinically significant stenosis [10]. Patients generally seek medical attention when the stenosis occludes about 70% of the normal tracheal lumen. For this reason, mild stenoses are not detected.Surgical treatment is considered for a small number of symptomatic patients. In their series, Grillo and Pearson also reported stridor and exertional dyspnea as important signs of stenosis in patients with PETS [5,6]. In the literature, the average length of PETS is reported as 2.6 cm [11]. In our series, all patients had complaints of dyspnea and stridor. The mean length of PETS was 3.2 ± 0.67 cm, similar to the literature.
Surgery is contraindicated, at least temporarily, in patients with poor general condition or unstable concomitant disease. Therefore, treatments, including bronchoscopic dilation, laser, and stenting, are recommended as an alternative to surgery [1,12]. Grillo et al. reported in a 1995 study that laser treatment was unsuccessful in 23-43% of cases and that conservative approaches can only be successful in selected patients [13]. In the present study, we observed that although bronchoscopic dilation is not an effective treatment, it is an effective method of gaining time until surgery and determining the length of the lesion by advancing the scope to the distal border of the stenotic segment. Of the 25 patients operated in our hospital, 15 (60%) had previously undergone dilation. These patients exhibited restenosis after the dilation procedure. Segmental tracheal resection and end-to-end anastomosis are the most effective methods for patients with PETS.
Although it may vary depending on stenosis location, the primary approach in cases of benign tracheal stenosis should be cervical incision and collar incision. Rarely, partial sternotomy can be performed if necessary. In a 589-case series published in 2004, Wright et al. reported using cervical, mediastinal, and thoracic incisions in 79.6%, 20%, and 0.5% of their patients, respectively [15]. In the present study, a cervical incision was used in all cases except a 76-year-old patient with stenosis 1.5 cm proximal to the tracheal carina. In order to minimize complications, curative surgery is only recommended for selected patients with good neurological, cardiovascular, and respiratory status. The basic principles for avoiding complications have been determined to be reducing the tensile force on the anastomosis, not disrupting the vasculature, and practicing meticulous dissection [16]. Release techniques are used to reduce the tensile force on anastomoses. Although the resection limit was 2 cm in early studies, this limit was increased up to 6.5 cm with the development of release techniques [14]. When we compared resection length and complication rates in the present study, the length of 3.73 cm in the group with complications and 2.95 cm in the group without complications was statistically significant, as expected (p = 0.006). The mean length of the resected segment was 3.13 cm in the three patients with fistulae, while this length was 3.21 cm in patients without fistulae (p = 0.906). We attribute the discrepancy between our results and those in the literature to our small patient group.
Release techniques include right hilar release, suprahyoid and laryngeal release, pulmonary ligament dissection, intrapericardial dissection of pulmonary vessels, reimplantation of the left main bronchus to the intermediary bronchus, and head flexion. Wynn et al. preferred supralaryngeal release to avoid postoperative dysphagia and reported a success rate of 89% [15]. All of these release techniques reduce tension on the anastomosis line as well as prevent surgical site separation and granulation, restenosis, and surgical site infection. Laryngeal release techniques were not used in any of the 25 patients in the present study.
Diabetes is an important predisposing factor for anastomotic complications. It increases the complication rate by 3% [16,17]. When we evaluated complication rates in terms of diabetes mellitus, various complications were observed in 4 of the five diabetic patients (p = 0.023). Microcirculation is known to be impaired in diabetic patients. Disruptions in collateral circulation are seen on the anastomosis line, which adversely affects tissue healing. Separation at the anastomosis line has been observed in 22% of diabetic patients [18]. Two of the three patients with fistulae in our study were diabetic (p = 0.091).
Another patient group with impaired microcirculation is patients undergoing revision surgery. We encountered complications in 2 of our three previously operated patients (p = 0.231), though these complications were surgical site infection and hoarseness. Although fistula was not observed, the rate of anastomotic complications is higher in these patients due to impaired collateral circulation.
Another important issue related to the development of complications is comorbidities [7]. In the present study, comorbidities were found to be associated with complication development (p = 0.024). One of our patients was died because of self-extubation after the operation. Self-extubation was damage the anastomosis. Therefore, comorbidities must be taken into account during patient selection. We believe that patient compliance is a more important criterion for patient selection than the length of the stenotic trachea.
As described by Grillo and Pearson, anastomosis of the posterior wall is done first with interrupted sutures; then the cartilage part is approximated with interrupted sutures [13,19]. Macchiarini used the continuous suture technique on the posterior wall and reported a restenosis rate of 7.6% [20]. Wynn et al. used the posterior and anterior interrupted anastomosis technique described by Grillo and Pearson and reported 11% restenosis [15]. In the present study, polyglactin and PDS sutures were used in all patients. The ratio of polyglactin to PDS use was 12%/88% for the membranous part and 32%/68% for anterior wall anastomosis, respectively. As the anastomosis technique; interrupted sutures were used in the anterior wall in all patients, while the ratio of interrupted to continuous suture use in the membranous wall was 36%/64%, respectively.
Anastomotic complications are detected during routine bronchoscopic examinations [21]. Wright et al. stated that the best option for the treatment of restenosis is the T-tube or tracheostomy tube because it does not impair airway humidification and allows phonation [17]. In the present study, repeated bronchoscopy and laser ablation were performed on two patients with granulation. One patient with restenosis underwent a permanent tracheostomy.
The limitations of the study are the retrospective design and the fact that the patients’ preoperative general condition could not be evaluated, and their operations were performed by different surgeons may create bias in our study.
In conclusion, while we were not able to identify risk factors for fistulae due to the small number of patients in our study, we determined that comorbidities were the most important factor affecting postoperative complications. Although tracheal surgery is associated with high postoperative morbidity and mortality, we believe these risks can be reduced with experienced surgeons and appropriate patient selection.
Declaration of conflicting interests
The authors declared no conflicts of interest with respect to the authorship and/or publication of this article.
Funding
The authors received no financial support for the research and/or authorship of this article.
Reference
1) Bisson A, Bonnette P, Leroy M, Colchen A, Personne C, Toty L et al. Tracheal sleeve resection for iatrogenic stenoses (subglottic laryngeal and tracheal). J Thorac Cardiovasc Surg 1992;104:882-7.
2) Perotin J-M, Jeanfaivre T, Thibout Y, Jouneau S, Lena H, Dutau H et al. Endoscopic management of idiopathic tracheal stenosis. Ann Thorac Surg 2011;92:297-301.
3) Balis E, Kotsifas K, Tatsis N, Papanikolaou A, Boulia S, Chrysou G et al. Long-term results of bronchoscopic cryotherapy for post-intubation tracheal stenosis. Eur Respir J 2018;52:PA4160. doi:10.1183/13993003.congress-2018.pa4160.
4) Mehta AC, Lee FYW, Cordasco EM, Kirby T, Eliachar I, De Boer G. Concentric tracheal and subglottic stenosis: management using the Nd-YAG laser for mucosal sparing followed by gentle dilatation. Chest 1993;104:673-7.
5) Pearson FG, Andrews MJ. Detection and management of tracheal stenosis following cuffed tube tracheostomy. Ann Thorac Surg 1971;12:359-74.
6) Grillo HC. Surgical treatment of postintubation tracheal injuries. J Thorac Cardiovasc Surg 1979;78:860-75.
7) Hashemzadeh S, Hashemzadeh K, Kakaei F, Aligholipour R, Ghabili K. Surgical treatment of postintubation tracheal stenosis: Iranian experience of effect of previous tracheostomy. Int J Gen Med 2012;5:93.
8) Nandakumar R, Jagdish C, Prathibha CB, Shilpa C, Sreenivas V, Balasubramanya AM et al. Tracheal resection with end-to-end anastomosis for post-intubation cervical tracheal stenosis: study of 14 cases. J Laryngol Otol 2011;125:958-61.
9) Papla B, Dyduch G, Frasik W, Olechnowicz H. Post-intubation tracheal stenosis-morphological-clinical investigations. Pol J Pathol 2003;54:261-6.
10) Stratakos G. Postintubation tracheal stenosis and endoscopic management. Pneumon 2003;16:262-70.
11) V. McCaffrey T. Classification of laryngotracheal stenosis. Laryngoscope 1992;102:1335-40.
12) Martinez-Ballarin JI, Diaz-Jimenez JP, Castro MJ, Moya JA. Silicone stents in the management of benign tracheobronchial stenoses: tolerance and early results in 63 patients. Chest 1996;109:626-9.
13) Grillo HC, Donahue DM, Mathisen DJ, Wain JC, Wright CD. Postintubation tracheal stenosis: treatment and results. J Thorac Cardiovasc Surg 1995;109:486-93.
14) Van der Maten J, Blaauwgeers JLG, Sutedja TG, Kwa HB, Postmus PE, Wagenaar SS. Granular cell tumors of the tracheobronchial tree. J Thorac Cardiovasc Surg 2003;126:740-3.
15) Wynn R, Har-El G, Lim JW. Tracheal resection with end-to-end anastomosis for benign tracheal stenosis. Ann Otol Rhinol Laryngol 2004;113:613-7.
16) Sezen CB, Kocaturk CI, Bilen S, Kalafat CE, Cansever L, Dincer SI et al. Long-Term Outcomes of Carinal Sleeve Resection in Non-Small Cell Lung Cancer. Thorac Cardiovasc Surg 2020;68:190-8.
17) Wright CD, Grillo HC, Wain JC, Wong DR, Donahue DM, Gaissert HA et al. Anastomotic complications after tracheal resection: prognostic factors and management. J Thorac Cardiovasc Surg 2004;128:731-9.
18) Blasberg JD, Wright CD. Surgical considerations in tracheal and carinal resection. Semin Cardiothorac Vasc Anesth 2012;16:190-5.
19) Pearson FG, Cooper JD, Nelems JM, Van AWN. Primary tracheal anastomosis after resection of the cricoid cartilage with preservation of recurrent laryngeal nerves. J Thorac Cardiovasc Surg 1975;70:806-16.






