

Summary
Fistulas between the respiratory and digestive tract (trachea-esophageal, broncho-esophageal) can be congenital or acquired. Acquired fistulas due to malignancy can occur by direct invasion of the malignant tissue; or it may be a result of surgical treatment, chemotherapy or radiotherapy. Although such fistulas occur during or shortly after treatment, it is unlikely that they will emerge long years after treatment. We report a case of late term broncho-esophageal fistula and an endoscopic treatment method in a patient who underwent left pneumonectomy for bronchial carcinoma. Treatment of the patient was accomplished with bronchoscopic placement of polyglycolic acid patch with surgical tissue glue into the fistula tract. Fistulas between trachea-bronchus and digestive tract should be kept in mind, after surgical interventions of neighborhood structures. Bronchoscopic interventions may be a treatment alternative in appropriate patients.Introduction
Broncho-esophageal fistula in adults is a challenging problem for surgeons. Previously the initial treatment choice of this complication was surgery [1]. As a result of the development of endoscopic and bronchoscopic interventional methods and materials, such interventions can be used as the first choice in the treatment of broncho-esophageal fistula [2].Case Presentation
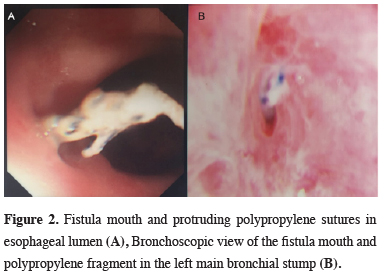
A 68-year-old male patient underwent left pneumonectomy in 2004 due to poorly differentiated squamous cell bronchial carcinoma. During the procedure, partial esophagus wall resection was performed due to invasion of tumor into the outer muscle tissue of the esophagus wall which was approximately 4 cm long. Pleural patch was used to support to esophageal wall and secure the mediastinum. The patient with pathological stage IIIA received chemotherapy and radiotherapy after surgery. Follow-up revealed no signs of recurrence for 9 years. In 2013, the patient was diagnosed with pneumonia after a cough complaint. Since the symptoms of the patient did not regress with antibiotics, thoracic tomography was performed, which revealed clues of broncho-esophageal fistula. In his esophagography, enlarged esophagus part due to the partial wall resection and the contrast leakage from esophagus to the left bronchial stump was seen (Figure 1). During esophagoscopy procedure, fistula orifice was observed in the 25th centimeter of the esophagus with the polypropylene suture part which was partially closing the orifice (Figure 2). There was no connection between the fistula and the pneumonectomy space. After obtaining informed consent from the patient, endoscopic fistula closure was planned and rigid bronchoscopy was performed under general anesthesia. During bronchoscopy, one end of the polypropylene suture was observed in the bronchial system. (Picture 3). After removing the suture material from the fistula tract, about 1 cm of polyglycolic acid patch (NEOVEIL- Gunze Limited, Kyoto/Japan) was placed tightly on the fistula tract and surgical tissue glue (TISSEEL- Johnson & Johnson corp. /New Jersey/USA) was applied on it. The procedure was ended after waiting for the drying time of the glue. In the follow-up, the patient had no symptoms and control bronchoscopy and esophagography (Figure 1) was performed 3 weeks later and there was no evidence of fistula. During the annual controls of the patient, there was no fistula signs and symptoms until the present day.
 Click Here to Zoom |
Figure 1: Esophagography before the closure of the broncho-esophageal fistula (Yellow arrow: dilated esophagus, Red arrow: the passage of the contrast through the fistula) (A), esophagography after the closure of the fistula without contrast leakage (B). |
 Click Here to Zoom |
Figure 2: Fistula mouth and protruding polypropylene sutures in esophageal lumen (A), Bronchoscopic view of the fistula mouth and polypropylene fragment in the left main bronchial stump (B). |
Written informed consent was obtained from the patient for publication of his data.
Discussion
Tracheo-broncho-esophageal fistulas can lead to severe lung complications and should be treated immediately after diagnosis. Fistulas can be seen immediately after surgery, or it may take years to appear. They are mostly seen in left side probably due to the relation with the esophagus and the left main bronchial stump after left pneumonectomy as in our patient [1]. Esophageal wall involvement and the suture material used to close the stump are probably responsible for fistula development. Contrast-enhanced esophagography is essential in diagnosis [2]. Treatment options vary from endoscopic procedures to surgery [2,3]. The goal of treatment is to prevent contamination of the bronchial system and to protect the patient from recurrent pneumonia and associated septic complications. The general condition of the patient and the localization of the fistula should be considered while planning the treatment. Considering that the majority of cancer patients have a high probability of surgical procedure complications, endoscopic interventions should be the primary treatment option. Moreover, even if endoscopic interventions fail, they do not interrupt the open surgical interventions for the treatment [4]. Endoscopic interventions can be performed via the airway or esophagus [3-5]. Endoscopic stent applications with esophagoscopy or bronchoscopy or endoscopic clipping via esophageal way are some of the treatment options. Additionally tissue adhesive can be applied directly to the fistula area [5]. Usually esophageal route is preferred for endoscopic clip use and stent applications. However, in patients with esophageal dilatation, these methods have a low chance of success and may be difficult to perform. In recent years, some successful results have been published on closure of esophageal fistulas using polyglycolic acid patch and tissue glue [6,7]. However these applications were made via esophagoscopy, bronchial interventions can be a treatment choice especially in patients with dilated esophagus. And we think that polyglycolic acid patch application into the fistula tract with surgical tissue glue had an additive effect on tissue adhesion since there is no recurrence in our patient for 5 years.In conclusion, the possibility of fistula in operated bronchial cancer patients with chronic cough complaints should be kept in mind even if they have passed through for many years. Endoscopic procedures should be preferred as initial therapy because they involve less risk compared to open surgical methods. Fistula closure with polyglycolic acid patch and surgical tissue glue via bronchoscopic way may be a treatment alternative.
Declaration of conflicting interests
The authors declared no conflicts of interest with respect to the authorship and/or publication of this article.
Funding
The authors received no financial support.
Authors’ contributions
MCS, ED; Collected the data, performed the analysis, co-wrote the paper.
Reference
1) Moreno P, Lang G, Taghavi S, Aigner C, Marta G, De Palma A et al. Right-sided approach for management of left-main-bronchial stump problems. Eur J Cardiothorac Surg 2011; 40: 926-30.
2) Balazs A, Kupcsulik PK, Galambos Z. Esophagorespiratory fistulas of tumorous origin. Non-operative management of 264 cases in a 20-year period. Eur J Cardiothorac Surg 2008; 34: 1103-7.
3) Ahn JY, Jung H-Y, Choi JY, Kim M-Y, Lee JH, Choi K-S et al. Benign bronchoesophageal fistula in adults: endoscopic closure as primary treatment. Gut Liver 2010; 4: 508-13.
4) Wang H, Tao M, Zhang N, Li D, Zou H, Zhang J et al. Airway Covered Metallic Stent Based on Different Fistula Location and Size in Malignant Tracheoesophageal Fistula. Am J Med Sci 2015; 350: 364-8.
5) Scappaticci E, Ardissone F, Baldi S, Coni F, Revello F, Filosso PL et al. Closure of an iatrogenic tracheo-esophageal fistula with bronchoscopic gluing in a mechanically ventilated adult patient. Ann Thorac Surg 2004; 77: 328-9.



