

2Clinics of Anesthesiology and Reanimation, Samsun Research and Education Hospital, Samsun, Turkey
3Department of Thoracic Surgery, Ondokuz Mayıs University, Medical School, Samsun, Turkey
4Department of Anatomy, Ondokuz Mayıs University, Medical School, Samsun, Turkey DOI : 10.26663/ cts.2022.003
Summary
Background: We aimed to evaluate the changes in pain, dyspnea perception and respiratory functions by applying pain tape in the postoperative period in patients who underwent thoracotomy.Materials and Methods: 55 patients were included in the prospective, randomized study with local ethics committee approval. The patients were divided into two groups, and on the postoperative 1st day, pain tape was applied to group I patient and placebo tape similar to pain tape was applied to group II patient. Visual Analogue Scale (VAS) was used for pain assessment, Modified Borg Scale (MBS) for dyspnea assessment, pulmonary function test and six-minute walking test (6 MWT) were used to evaluate pulmonary functions in the preoperative and postoperative periods.
Results: There were 29 patients in group I and 26 patients in group II, with mean age of 59.2 ± 10.4 (18- 75) years. According to the statistical analysis, no difference was found between the groups in terms of age, gender, height, weight, BMI, 6 MWT, MBS, FEV1, FVC, FEV1/FVC values (p > 0.05). There was a difference between the groups in terms of VAS values measured on the 3rd postoperative day (4.65 ± 1.79 vs. 6.57 ± 1.74; p > 0.001). In addition, the postoperative complication rate was different in group I compared to group II (17.2% vs. 30.7%; p = 0.003).
Conclusion: Pain tape application is a reliable and simple method for pain control in the postoperative period in patients undergoing thoracotomy. It can be applied to patients for pain control in the early period, and in this way, the development of postoperative complications can be prevented.
Introduction
Thoracotomy pain is an acute traumatic pain that occurs due to iatrogenic causes such as soft tissue, muscle and visceral damage, bone and joint trauma, inflammation. Insufficient breathing and coughing, atelectasis, hypoxia and lung infections due to this pain are important causes of postoperative morbidity [1,2]. Effective analgesia provides early postoperative mobilization and reduces morbidity. Today, there are a wide variety of methods and drugs used to relieve pain after thoracotomy. These are; systemic narcotic analgesic or nonsteroidal anti-inflammatory drug use, patient-controlled analgesia, thoracic epidural analgesia, cryoanalgesia, transcutaneous nerve stimulation, paravertebral block, intercostal nerve block, and administration of local anesthetic agents to the intrapleural and extrapleural space [3-5].Integration of all these analgesia techniques with the pulmonary rehabilitation program can accelerate recovery, prevent postoperative pulmonary complications, and shorten the hospital stay [6,7]. New ones are added to the classical respiratory physiotherapy techniques applied today. One of these new techniques is the application of pain tape, which is known to help in pain management. Pain tape; kinesiology taping technique was developed in the 1970s by Dr. Kenzo Kase to prevent limitations in joint movements and functional activities, which are an undesirable effect in standard tape and tape applications. This tape contains polymer fibers, which has a 60% stretching share, is used to integrate the inflamed areas for any reason, reduce edema, and support circulation. Due to the absence of any pharmacological agents in the tape and its hypoallergenic feature, it provides ease of use in all patients from the pediatric group to the geriatric group [8].
The aim of our study is to investigate the effect of pain tape application on postoperative pain, dyspnea level, and respiratory functions in addition to routine analgesic treatment in patients undergoing thoracotomy.
Methods
Fifty five patients who underwent thoracotomy were included in our prospective, randomized, double-blind and placebo-controlled study, which was approved by Ondokuz Mayıs University Medical Research Ethics Committee. All cases were operated by the same thoracic surgery team under the supervision of an experienced anesthesiologist. Similar surgical indications and anesthesia management were used. All cases were approached with posterolateral or lateral thoracotomy, depending on the surgeon’s preference. A single dose of cefuroxime axetil administered as a prophylactic intravenous (IV) antibiotic regimen (Cefaks© 1.5 g/flk, Deva, Istanbul, Turkey) and an additional dose was administered at the 4th hour when the surgery was prolonged. At the end of the operation, a chest tube was placed in the 7th or 8th intercostal space accordingly. All patients were extubated in the operating room and transferred to the intensive care unit. In the absence of any obstacle, the patients were transferred to the service on the first postoperative day.For postoperative analgesia, dexketoprofen (Arveles© 50 mg, UFSA İlaç, İstanbul, Turkey) in 2x1 doses and paracetamol (Parol© 10 mg/mL, Atabay İlaç Fabrika A.Ş., Istanbul, Turkey) 3x500 mg IV was given for all patients. Tramadol hydrochloride IV (Contramal© 100 mg/2 mL, Abdi İbrahim, Istanbul, Turkey) and pethidine hydrochloride IM (Aldolan© 100 mg/2 mL, LIBA laboratories A.Ş., Istanbul, Turkey) were administered when necessary.
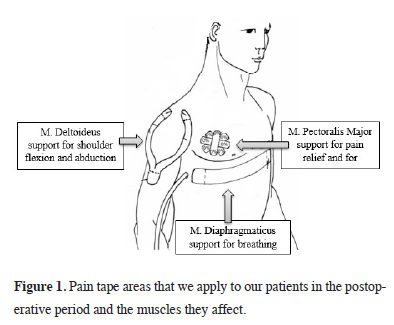
The patients who were taken to the service on the 1st postoperative day were divided into two groups, and pain tape (Kinesio Taping Association International, Albuquerque, NM, USA) was applied to group I (n = 29) patients and a placebo tape similar to pain tape was applied to group II (n = 26) patients. Pain tape taping was applied to the patients on the 1st postoperative day together with the dressing by a physiotherapist who is an expert in the field. The application to be made in the placebo control group was applied by the same specialist physiotherapist to the same areas with the clothing tape in a way that mimics the application of the pain tape. The physiotherapist applying taping did not know whether the tapes were placebos or real tapes. Tape application was made in standardized length, tension, and shape. Three skin areas designated for application, the pain trigger point, were found on the patient by palpation. Y-shaped deltoid/trapezius inhibition on the ipsilateral deltoid/trapezoid and Y- and I-shaped tapings were made on the diaphragm for relaxation and facilitation [9] (Figure 1). The tapes were removed on the day the patient was discharged.
 Click Here to Zoom |
Figure 1: Pain tape areas that we apply to our patients in the postoperative period and the muscles they affect. |
In the study, Visual Analogue Scale (VAS) [10] was used for pain assessment, Modified Borg Scale (MBS) [11] for dyspnea assessment, six-minute walk test (6 MWT) [12] and pulmonary function test (PFT) were used to assess pulmonary functions in the preoperative and postoperative periods. VAS and MBS were applied preoperatively and postoperatively on the 1st and 3rd days, 6 MWTs were performed preoperatively and postoperatively on the 3rd day, and PFT was performed at the preoperative and postoperative 3rd month. The specialist physiotherapist and patients who made these evaluations did not know which group they were in.
The inclusion criteria for the study are; patients who have undergone thoracotomy, patients who have not applied a pain tape before the surgical procedure, patients who can cooperate in the postoperative period, patients who give voluntary consent and patients between the ages of 18-80. The exclusion criteria for the study are; patients staying in the intensive care unit for more than 24 hours after surgery, patients with previous thoracic trauma, thoracotomy, or tube thoracostomy, patients who receive psychiatric treatment and cannot cooperate due to the drugs they use, patients who cannot give their own voluntary consent, patients under 18 years of age and patients who develop allergies to the applied pain tape.
Statistical Analysis
Whether the data met the normality assumption was checked using the Shapiro-Wilk test. Mann-Whitney U test was used to test the difference between two groups in terms of ordinal or non-normally distributed continuous variables. Results are expressed as mean value ± SD, or median value and interquartile range (IQR). Bonferroni correction was applied for multiple tests. Number and % values were given for categorical variables. Since the data to be obtained from the study will be subjected to the t-test, considering the power and sample size test based on previous studies in this area, the sample size was calculated as alpha=0.05 and the power of the test was 90%, with a minimum of 25 patients per group. SPSS Windows version 24.0 (Chicago, IL, USA) package program was used for statistical analysis and p < 0.05 was considered statistically significant.
Results
Of the 55 patients included in the study, 46 were male and 9 were female, with mean age of 59.2 ± 10.4 (18-75) years. It was determined that 74.54% (n = 41) of the patients were active smokers. The most common type of surgery was lobectomy in 27 patients and segmentectomy/wedge resection in 12 patients. In the study, the mean hospital stay was 7.12 ± 3.2 days and no mortality was observed for thirty days. There was no statistical difference between the groups in terms of age, gender, weight, height, BMI, ASA score, PFT values, smoking status, types of surgery, duration of chest tube stay and duration of hospitalization. Demographic and preoperative data of the patients are shown in Table 1.Table 1: General characteristics and data of the patients.
There was no significant difference between the groups in terms of FVC, FEV1, FEV1/FVC and PEF values according to the pulmonary function test results performed in the preoperative and postoperative period. Again, although MBS and 6 MWT values performed in the postoperative period were better in group I patients, no statistical difference were found between the groups. When VAS values were evaluated, there was no significant difference between preoperative (1.0 ± 0.88/ 1(2) vs. 0.92 ± 0.97/ 1(2); p = 0.762) and postoperative 1st day values (6.62 ± 1.84/ 7(3) vs. 7.07 ± 1.54/ 7(2); p = 0.323), while VAS values were significantly lower on the 3rd postoperative day in group I patients (4.65 ± 1.79/ 4(3) vs. 6.57 ± 1.74/ 6.5(3); p < 0.001) (Table 2).
Table 2: Comparison of the groups in terms of preoperative and postoperative data.
Although hospitalization time (6.5 ± 3.01 days vs. 7.8 ± 3.8 days; p = 0.167) and chest tube removal time (4.9 ± 1.81 days vs. 5.2 ± 2.08 days; p = 0.354) were shorter in Group I, no statistical difference was found. When compared in terms of postoperative complications, it was found to be 17.2% (n = 5) in group I and 30.7% (n = 8) in group II, which was statistically significant (p = 0.003) and the most common complication was atelectasis. (Table 1).
Discussion
According to the results of this prospective, randomized, double-blinded and placebo-controlled study, it is seen that pain tape application is effective in pain control in the early postoperative period. In our study, in which we evaluated the perception of pain in patients with VAS, it was observed that while VAS was significantly lower in group I patients on the postoperative 3rd day than in group II patients, this value was the same in both groups on the postoperative 1st day. We attribute this situation to the intensive analgesic administration in the intensive care unit before the first postoperative day. In addition, the complication rate observed in the early postoperative period was lower in group I patients, indicating that patients had good pain control in the early postoperative period.In the postoperative period, as after many surgeries, severe pain occurs in approximately 70% of patients after thoracotomy. Pain after thoracotomy is an acute traumatic pain and occurs as a result of stretching of the costovertebral, costotransverse joint ligaments, and posterior spinal muscles [1,2]. After all thoracotomy operations, whether pulmonary resection is performed or not, respiratory muscle strength decreases and respiratory reserve decreases due to the deteriorated respiratory physiology due to the surgical procedure. In addition, postoperative pain restricts diaphragmatic movements by creating phrenic nerve inhibition and causes a decrease in its strength [13]. As a result, breathing becomes shallow, lung volume and capacity decreases, coughing reflex is impaired, causing sputum retention, atelectasis, hypoxemia, hypercapnia and respiratory failure. In addition, age, cardiopulmonary comorbidities, smoking history, variable and low pulmonary function test results, and low exercise capacity increase the risk of postoperative pulmonary complications (PPC) [14-16].
Although developments in postoperative pain management, innovations in anesthesia, and surgery in the last 20 years have reduced general postoperative complications, the most important cause of mortality and morbidity in thoracic surgery is still postoperative pulmonary complications. Factors such as the operation performed, the type of incision and the size of the tissue removed may affect the result, and the rate of PPC can reach 36% [17,18]. In addition, PPC increases the length of stay of patients in the intensive care unit and hospital, and health expenditures [7,19].
To date, various treatment strategies and methods have been developed to reduce the incidence of PPC, such as the detection and prevention of risk factors, improvement of preoperative condition and patient education, intraoperative applications, and postoperative pulmonary care [16-18]. Among these, respiratory physiotherapy has been accepted as a useful practice in preventing pulmonary complications and it has been recommended to be routinely applied by the European Respiratory Society (ERS), European Society of Thoracic Surgeons (ESTS) [20] and American College of Chest physicians (ACCP) [21] due to its functional benefits.
According to the current literature, postoperative pulmonary rehabilitation applied in the early period after thoracic surgery aims; to increase alveolar ventilation, to increase lung volume and capacity, to ensure effective coughing, and to prevent areas under mechanical pressure from going into atelectasis during surgery [13,18]. Although it is stated in the literature that postoperative physiotherapy is necessary and beneficial, there is no standard information about which program should be applied to which patient. The rehabilitation program to be implemented should be planned individually according to the patient’s clinic and needs [7,18]. In our study, we applied the pain tape taping technique, which is a pulmonary rehabilitation application method that has not been investigated and mentioned much in patients who underwent thoracotomy.
The pain tape taping technique is a rehabilitation method that was developed in the 1970s and consists of application. A specially designed elastic tape (Kinesio®) is applied to the patient’s skin to replace the underlying soft tissue areas and achieve therapeutic effects [8]. By causing the skin to rise in the area where the pain patch is applied, it increases the skin and subcutaneous interstitial area, thus increasing circulation and movement in this area. The increase in circulation and movement directs the exudate to the lymphatic pathways, reducing the edema and inflammation and reducing the pain. In addition, the pain tape provides stimulation of mechanoreceptors through the skin, thereby activating the central nervous system [8,22]. In our study, we also used the pain tape taping method, which is easy to apply and does not cause any discomfort to the patient, and we found that the patients in the group in which we applied the pain tape had less pain in the early postoperative period and accordingly, the postoperative complication rate was lower.
The modified Borg scale was developed by the Borg in 1970 to measure the effort expended during physical exercise. It is a scale that is frequently used to evaluate the severity of dyspnea on exertion and the severity of dyspnea at rest [11]. Studies have reported that MBS is a reliable scale for determining the severity of resting and exertional dyspnea and is correlated with respiratory rate and pulmonary function tests. In addition, it is emphasized that MBS is superior to other scales in terms of long-term reproducibility and can be used to predict respiratory reserves of patients. In a study conducted by Akkoca et al, it was found that there was a relationship between the mean dyspnea severity evaluated by patients with MBS and pulmonary function test parameters. In another study conducted by Güneş et al [23,24], it was determined that there was a relationship between the mean dyspnea severity evaluated by patients with MBS and lung functional parameter values. In our study, we used MBS in our patients in the preoperative and postoperative periods to evaluate the perception of dyspnea. Accordingly, we did not observe a statistical difference between the groups, although the MBS values were lower, especially on the postoperative 3rd day, in our patients who were applied pain tape.
Respiratory system functions are always affected during and after surgery. After pulmonary resection, there is an increase in residual volume as a result of both removal of the lung parenchyma tissue and decreased diaphragm and chest wall mobility. While the FEV1 value shows a rapid decrease in the early period; general anesthesia applications cause a decrease in functional residual capacity. This depends on the anaesthetic agents and muscle relaxants used during surgery [20,21]. When the findings related to pulmonary function tests were examined in our study, we found a decrease in the FVC, FEV1, FEV1/FVC, and PEF values measured in both groups of patients in the postoperative period. This decrease was less in group I patients than in group II patients, but we did not observe a statistical difference between the two groups.
The six-minute walk test, developed by Balke in 1963 to measure functional exercise capacity, is a submaximal, indirect cardiovascular physical fitness test. The parameter it tries to measure indirectly is the maximal oxygen consumption, and it measures the distance the person takes in 6 minutes in meters [12]. 6 MWT is easy to perform and evaluate, it does not require equipment. A normal person’s walking distance is 400-700 meters during this time. The six-minute walk test is a widely used approach to evaluate the change in functional exercise capacity of patients in the pulmonary area [13,25]. In a related study in the literature, it was reported that the exercise capacity measured by the 6 MWT improved significantly more than the control group in the 4-week pulmonary rehabilitation program applied to lung cancer patients after resection [13]. In another study conducted by Spruit et al [26] with patients who underwent resection for lung cancer, it was reported that the 6-minute walking distance of the 8-week pulmonary rehabilitation program was significantly better than the control group. Since it was an easily applicable test in our study, we applied 6 MWT to our patients preoperatively and postoperatively. Accordingly, although postoperative 6 MWT values were better in group I patients to whom we applied pain tape, compared to group II patients, we did not detect a statistical difference between the groups.
In conclusion, there is a need for well-programmed and fully implemented pulmonary rehabilitation programs to reduce pain after thoracotomy operations, eliminate pulmonary complications, and return the patient to their preoperative functional life as soon as possible. Considering the clinical benefits, giving importance to simple, cost-effective and low-risk PR practices in thoracic surgery clinics will be important in terms of the success of the surgery, health costs and patient benefits. In this study, we applied pain tape in addition to routine postoperative pain treatment in patients who underwent thoracotomy, and we found that patients felt less pain in the early postoperative period. From this point of view, pain tape seems to be an easy to apply, inexpensive and effective method, and we recommend it to be applied as a part of the pulmonary rehabilitation program in addition to routine pain treatment in patients.
Declaration of conflicting interests
The authors declared no conflicts of interest with respect to the authorship and/or publication of this article.
Funding
The authors received no financial support for the research and/or authorship of this article.
Ethics approval
The study was approved by the Medical Research Ethics Committee of Ondokuz Mayıs University, Faculty of Medicine (KAEK/383).
Authors’ contribution
SGT, BÇ; Conceived and designed the analysis, collected the data, contributed data/analysis tools, performed the analysis, co-wrote the paper, HKÇ; Conceived and designed the analysis, performed the analysis, co-wrote the paper, ZA; Collected the data, co-wrote the paper.
Reference
1) Benumof JL. Management of postoperative pain. In: Benumof JL, ed. Anesthesia for Thoracic Surgery. 2nd ed. Philadelphia. W.B. Sounders Company, 1995; 756-74.
2) Sentürk M. Acute and chronic pain after thoracotomies. Curr Opin Anaesthesiol 2005; 18: 1-4.
3) Kavanagh BP, Katz J, Sandler AN. Pain control after thoracic surgery. A review of current techniques. Anesthesiology 1994; 81: 737-59.
4) Sentürk M, Ozcan PE, Talu GK, Kiyan E, Camci E, Ozyalçin S et al. The effects of different analgesia techniques on long-term postthoracotomy pain. Anesth Analg 2002; 94: 11-5.
5) Soto RG, Fu ES. Acute pain management for patients undergoing thoracotomy. Ann Thorac Surg 2003; 75: 1349-57.
6) Rodriguez-Larrad A, Vellosillo-Ortega JM, Ruiz-Muneta C, Abecia-Inchaurregui LC, Seco J. Postoperative respiratory exercises reduce the risk of developing pulmonary complications in patients undergoing lobectomy. Arch Bronconeumol 2016; 52: 347-53.
7) Çınar HU, Kefeli Çelik H, Çelik B, Doğan C. Is respiratory physiotherapy effective on pulmonary complications after lobectomy for lung cancer? Turk Gogus Kalp Dama 2020; 28: 638-647.
8) Kase K, Wallis J, Kase T. Clinical therapeutic applications of the Kinesio taping method, 2nd ed. Tokyo, Japan: Ken Ikai Co. Ltd.; 2003.
9) Imperatori A, Grande A, Castiglioni M, Gasperini L, Faini A, Spampatti S et al. Chest pain control with kinesiology taping after lobectomy for lung cancer: initial results of a randomized placebo-controlled study. Interact Cardiovasc Thorac Surg 2016; 23: 223-30.
10) McCormack HM, Horne DJ, Sheather S. Clinical applications of visual analogue scales: a critical review. Psychol Med 1988; 18: 1007-1019.
11) Borg GA. Psychophysical bases of perceived exertion. Med Sci Sports Exerc 1982; 14: 377-81.
12) ATS Committee on Proficiency Standards for Clinical Pulmonary Function Laboratories. ATS statement: guidelines for the six-minute walk test. Am J Respir Crit Care Med 2002; 166: 111-7.
13) Riesenberg H, Lübbe AS. In-patient rehabilitation of lung cancer patients-a prospective study. Support Care Cancer 2010; 18: 877-82.
14) Smetana GW. Postoperative pulmonary complications: an update on risk assessment and reduction. Cleve Clin J Med 2009; 76: S60–5.
15) Canet J, Gallart L, Gomar C, Paluzie G, Vallés J, Castillo J et al. Prediction of postoperative pulmonary complications in a population-based surgical cohort. Anesthesiology 2010; 113: 1338–50.
16) Feltracco P, Serra E, Barbieri S, Milevoj M, Ori C. Postoperative care of patients undergoing lung resection. J Anesthe Clinic Res 2012; 4: 288.
17) Reeve JC. Physiotherapy interventions to prevent postoperative pulmonary complications following lung resection. What is the evidence? What is the practice? NZ J Physiother 2008; 36: 118-30.
18) Stéphan F, Boucheseiche S, Hollande J, Flahault A, Cheffi A, Bazelly B et al. Pulmonary complications following lung resection: a comprehensive analysis of incidence and possible risk factors. Chest 2000; 118: 1263-70.
19) Varela G, Ballesteros E, Jiménez MF, Novoa N, Aranda JL. Cost-effectiveness analysis of prophylactic respiratory physiotherapy in pulmonary lobectomy. Eur J Cardiothorac Surg 2006; 29: 216-20.
20) Brunelli A, Charloux A, Bolliger CT, Rocco G, Sculier JP, Varela G et al. ERS/ESTS clinical guidelines on fitness for radical therapy in lung cancer patients (surgery and chemoradiotherapy). Eur Respir J 2009; 34: 17-41.
21) Deng GE, Rausch SM, Jones LW, Gulati A, Kumar NB, Greenlee H et al. Complementary therapies and integrative medicine in lung cancer: diagnosis and management of lung cancer, 3rd ed: American Physicians Evidence-Based Clinical Practice Guidelines. Chest 2013; 143: 420-36.
22) Kalichman L, Vered E, Volchek L. Relieving symptoms of meralgia paresthetica using Kinesio taping: a pilot study. Arch Phys Med Rehabil 2010; 91: 1137-9.
23) Akkoca Ö, Öner F, Saryal S. The relationship between dyspnea and pulmonary functions, arterial blood gases and exercise capacity in patients with COPD. Tüberküloz ve Toraks Dergisi 2001; 49: 431-8.
24) Güneş ÜY, Kara D, Erbağcı A. Comparison of the different dyspnea scales in patients with complaints of dyspnea. Dokuz Eylül Hemşirelik Yüksekokulu Elektronik Dergisi 2012; 5: 65-71.



