

Summary
Background: Buerger and Raynaud diseases are peripheral circulatory disorders that cause ulcers at fingers and affect the quality of life. The aim of this study is to detect the role of sympathectomy via video-assisted thoracoscopic surgery (VATS) in Buerger and Raynaud for an effective treatment.Materials and Methods: Study was designed retrospectively on prospective data. Sympathectomy via VATS, was applied to 45 patients who were diagnosed as Buerger or Raynaud disease in a 6-years period. Patients were followed with 6 months intervals. Age, gender, initial symptoms, smoking habit, quality of life with the operation type, duration and hospital stay were recorded. After surgery all datas related to the patient were also noted at follow-up period.
Results: Ten of 45 patients were in Buerger disease group and 35 in Raynaud. After VATS, existing finger ulcers were regressed 100% and regression in symptoms was more than 70% for both diseases. For overall, progression in life quality was noted as more than 95% of patients. Median hospital-stay was 2 days. There was no mortality and serious complication. Pneumothorax was the most common complication.
Conclusions: In order to increase the life quality of the patients and prevent the tissue loss, sympathectomy seems the only satisfactory surgical method of treatment for Buerger and Raynaud diseases especially for the circularity disorders of upper extremities.
Introduction
Thromboangiitis obliterans (Buerger), is an inflammatory disease of mid-sized arteries that hold the vessels of upper and lower extremities and it is strongly associated with smoking. The diagnosis depends on angiography, doppler ultrasonography and tissue biopsy, the inflammation occludes all the layers as panarteritis and panphlebitis. Atherosclerosis is not observed in the occluded arteries. Although it was Leo Buerger [1] in 1908, who published a detailed description of the pathological findings on 11 amputated limbs and named the disease, Winiwarter [2] had mentioned the disease as endarteritis obliterans far before that date. Males between the ages of 25 and 40 are under a higher risk. The upper extremities have a risk ratio of 45%. The disease progresses through recuperations and exacerbations. Protecting the extremities from severe hot and cold weather etc., quitting use of tobacco products are the main factors for an effective treatment.Raynaud’s phenomenon is characterized by recurring vasospasm of the fingers and toes by paleness, redness after bruising-cyanosis, after being exposed to cold or emotional stress. It has been proven that blood does not enter the capillaries when this condition is observed with a microscope [3]. The diagnosis is based on the identification of the attacks. Raynaud phenomenon is classified as primary (Raynaud’s disease) if there is not an underlying disease and secondary (Raynaud’s syndrome) if another disease has been confirmed. This phenomenon was first described by Maurice Raynaud in 1862 and later studied by Thomas Lewis in 1930 [4].
In response to the effective factor, faintness develops in the fingers and hands; when the effective factor disappears, cyanosis evolves in 8-10 minutes, then chilblains are observed and spread to the whole hand within an hour. Paresthesia, sensation of tingling, trophic changes on the skin and the bones in the advanced stages, even a clinical picture progressing towards gangrene. Digital skin temperature measurement, plethysmography and capillary microscopy methods can be used for the local blood flow. The cold pressor test is also an easy diagnostic test [4-6]. Raynaud phenomena occurs more frequently in women (20-30%), particularly in younger age populations (teens to 20s) [7]. The objective of the treatment is to decrease the number and the severity of the attacks, to prevent the amputations and tissue damage. Lewis [4] claimed that the primary pathology of the disease existed in the epitome of digital arteries which were affected by the sympathetic system. Hughes [8], described the endoscopic thoracic sympathectomy for the first time.
Handling with diseases includes preservation of the body temperature, using gloves and stockings, quitting smoking, decreasing emotional stress and exercising, vasodilators, antiaggregant agents, in some cases hyperbaric oxygen therapy as medical approaches [3,9]. However, sympathectomy seems the major surgical aspect. It should be applied in the case of vasospastic symptoms and superficial trophic disorders [10,11]. Despite the fact that the description of Buerger and Raynaud diseases has existed for almost 150 years, so far no consensus has been reached in respect to the classification, etiology, pathogenesis, diagnosis criteria and treatment methodology. There is an instability between the medical and surgical treatment that brings about a loss of time, the disenchantment of the patient’s faith in receiving treatment, worse still the formation of irreversible pathologies.
Due to the role of vasospasticity and increase in sympathetic tone in etiopathogenesis of both diseases, we thought it would be appropriate to examine the results and effectiveness of sympathectomy in treatment in both groups of patients. In our study, we planned to demonstrate effects of surgery in the treatment of Raynaud and Buerger, including short and long-term results, side effects, and recurrence rates, on the basis of patient satisfaction.
Methods
Study Group and DesignDuring the six-year period between 2005 and 2011, 45 patients, diagnosed with Raynaud and Buerger, were applied 75 thoracic sympathectomies with VATS. The study was planned retrospectively through prospective data. Patients were evaluated based on age, gender, smoking, duration of surgery, duration of hospitalization, treatment success, complications, follow-up and patient verbal reported satisfaction information.
In terminology for both Raynaud and Buerger, there is diversity in the naming that has come from the past and continues to the present day. We chose to define them as Raynaud and Buerger for the sake of consistency throughout our article, and to add a ‘phenomenon’ where appropriate, since it is considered a sign/symptom rather than a disease.
Although cold protection, sedatives, peripheral vasodilator drugs such as calcium channel blockers and pentoxidil and nicotine stopped medical treatment, severe symptoms, ulcer development and risk of amputation were considered as criteria for inclusion in the study, with the definition of lack of response to medical treatment. While Raynaud patients were diagnosed with clinical history and cold application testing, Buerger patients were diagnosed with Doppler ultrasonography and angiography, while operation indication was determined according to the symptoms and findings of the patients. Our patients’ hand temperatures during the preoperative period were measured. In the postoperative period, values were also measured and compared with preoperative values. Detection of complete drying and temperature increase in the hands at an early postoperative period was considered an indicator that sympathetic ganglia were effectively cauterized and sympathectomy was successful.
Follow-up period for patients was 1- 60 months. The patient was called for a check-up a week after sympathectomy. Long-term follow-up was either by control or by calling for re-changes in quality of life by the questionnaire in scoring between 0-5, before and after the surgery (reached a value of 0 is very distressed, very good with a value of 5 patient satisfaction). Surgeries were performed in the same thoracic surgery clinic and the author was the main or second surgeon. Study was approved by Ethic Committee of Vakıf Gureba Training and Research Hospital, registered by 2010-68/22. The work was carried out in accordance with the principles of the Helsinki Declaration, detailed information was given to all patients before ETS and informed consent forms were signed by patients.
Surgery
Under double-lumen intubated general anesthesia, all patients were administered a single-session endoscopic thoracoscopic sympathectomy (ETS) operation. In Raynaud 30 were bilaterally and surgery was started firstly with the right side, In Buerger patients the symptomatic side was the incision side. By a single port, with a 30-degree videothoracoscope, cauterization was used for T2-3-4, and rarely T5 ganglions. The efficacy of ETS is tested intraoperatively with the presence of dryness and increased heat in the hands just after the sympathectomy. Both lungs were expanded under a high pressure by the anesthesiologist at the end of the operation, the air was taken out, and without placing a chest tube, the incisions were sutured. Postoperative chest x-ray was in routine.
Statistical Analysis
The data obtained was analyzed statistically by using the SPSS for Windows® (V.11.0; SPSS, Inc., Chicago, Illinois, USA). Descriptive data of the effects of the same post-treatment (sympathectomy) data in two specific close-up diseases between certain years are shared. The entire universe that came to our clinic in the specified years was taken. Power was not calculated because there was no two-group comparison. Mean time to relapse was evaluated by Kaplan-Meier survival analysis. In descriptive analyses, the continuous variables were given as mean-standard deviation and categorical ones indicated as percentages and counts. Differences between the groups for categorical variables were analyzed using Chi Square test or Fisher’s Exact test. Difference between two dependent groups was evaluated by paired t test. P value less than 0.05 was considered significant.
Results
The age-range of 45 patients who did not response to medical treatment, was 15-76, the mean was 39.5 ± 18.5. While the age-range in the Buerger group was 26-76, with a mean of 47.4 ± 21.3, the age-range in the Raynaud group was 15-62 and mean of 36.7 ± 14.6. Thirty-five patients were Raynaud and 10 were Buerger patients. In total, 29 patients (64.4%) were male. In separately examining of the groups, the male sex was also seen more. It was noted that 27 out of 45 patients smoked an average of 15 ± 10 packs/year, between 2-35 packs. All 10 patients with Buerger and 17 of Raynaud patients were smoking (Table 1).Table 1: Sex and smoking data of Buerger and Raynaud patients.
It was realized that 42 of 45 (93.3%) patients had an increase in complaints about cold-contact. When symptoms are evaluated, there was redness in the 31 (68.9%) of the patients, in addition to this, there was excessive sweating complaints in 14 of them (31.1%). A total of 45 patients were applied 75 sympathectomies, including 30 patients with Raynaud bilaterally, the rest 5 patients and 10 patients with Buerger unilaterally. The left sympathectomy was applied to 10 patients (22.2%) applied to a single-sided operation (22.2%), the right of it was applied to 5 patients (11.1%). In 27 patients (60%) T2-3-4 level ganglions, in 18 patients (40%) T2-3-4-5 levels were cauterized (up to 4 cm to eliminate the fibers of Kuntz).
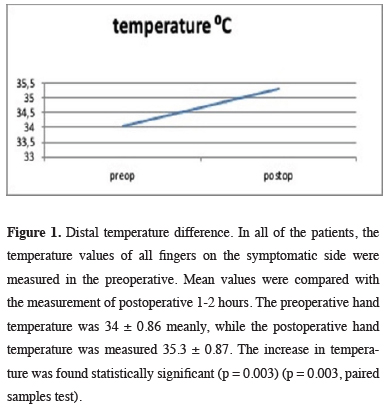
The surgery period was between 15-70 minutes, meanly 41 ± 15. As a surgical complication; in 16 cases (21.3%) of pneumothorax developed of 14 of needed tube thoracostomy. In 1 patient (2.2%) bronchospasm and respiratory-failure developed and improved with 16 hours of mechanical ventilation support. Mortality wasn’t observed. Duration of staying in hospital was 1-18 days and it was noted as a mean of 2 days. The five fingers’ temperatures on the diseased side were measured separately pre and postoperatively. The average values were compared. The hand temperature was measured as a mean of preoperative 34 ± 0.86, as postoperative 35.3 ± 0.87. The 1.30C increase in heat was found to be significant. This has shown that sympathectomy is effective at the applied levels (Figure 1).
 Click Here to Zoom |
Figure 1: Distal temperature difference. In all of the patients, the temperature values of all fingers on the symptomatic side were measured in the preoperative. Mean values were compared with the measurement of postoperative 1-2 hours. The preoperative hand temperature was 34 ± 0.86 meanly, while the postoperative hand temperature was measured 35.3 ± 0.87. The increase in temperature was found statistically significant (p = 0.003) (p = 0.003, paired samples test). |
In the follow-up of 45 patients, when preoperative and postoperative-life quality surveys were compared, it was stated that life quality of 15 patients (33.3%) was bad before surgery, 30 patients (66.6%) of life quality were worse, besides, one of the postoperative patients (2.2%) declared he hadn’t got any benefit of surgery, another 1 patient (2.2%) was worse compared to before. Regarding these cases, it was found that all patients with the disease of Buerger and Raynaud are 95.6% successful in improving the quality of life after sympathectomy.
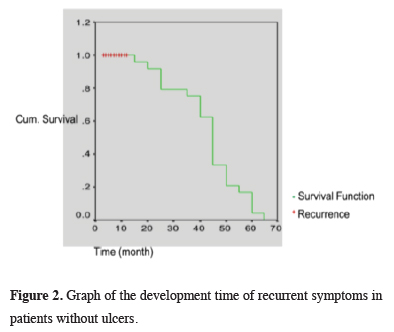
In the preoperative period, 22 patients (48.9%) with ulcer complaint (48.9%) of 11 (24.4%) only in one finger, of 6 (13.3%) on two fingers, of 4 (4%) on three fingers and 1 patient (2.2%) more than four ulcers on both hands had diagnosed. In postoperative follow-up, 22 patients’ ulcers which existed before sympathectomy healed of all (100%); however, due to both the patient’s exposure to external factors (hot- cold difference, smoking) and the clinical progress of the disease, it was observed that ulcers developed on the other fingers which didn’t exist beforehand. New ulcer development was observed in 6 (60%) of 10 Buerger and 8 (66.6%) of 12 Raynaud patients with ulcers. While 14 (63.6%) of the 22 ulcerated patients in our study group had recurrent ulcers in new localizations, 8 (36.4%) patients had no recurrence. If the remaining 8 patients become completely non-ulcerative is accepted as complete recovery, our success rate is 36.4% (Table 2, Figure 2).
Table 2: Results of Raynaud and Buerger patients with ulcer signs, after sympathectomy.
 Click Here to Zoom |
Figure 2: Graph of the development time of recurrent symptoms in patients without ulcers. |
In this table, we show statistically that the Buerger and Raynaud groups are similar and there is no difference between the groups
This non-mortal procedure has more than 70% complete symptom improvement in Raynaud’s patients and 100% success in target finger improvement in ulcerated patients. In addition, in terms of improving quality of life, our overall success is above 95%, even a subjective assessment.
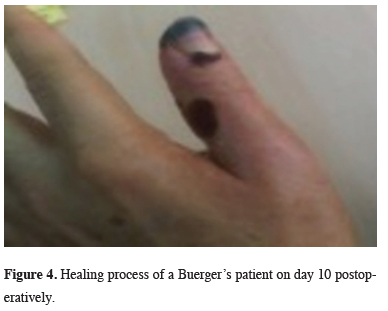
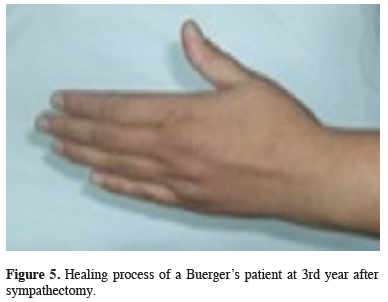
A whole recovery and progress have been succeeded in the patients of 33% with ulcer and Raynaud’s. As for the patients with no ulcer, the perfect success in the form of recovery and improvement of the symptoms has been 70% and whereas the partial success is 30%. In the survey of quality of life, 95.6% of the patients have indicated that they feel better and gave a higher score. The complete success of sympathectomy in the patients with Buerger’s has been assessed as 40% for the cases with ulcers (Figures 3-5). The symptom recovery rate could not be determined as there were no cases without ulcer and according to the survey of quality of life, success was again 95.6%.
 Click Here to Zoom |
Figure 3: Healing process of a Buerger’s patient with ulcer is shown preoperatively. |
 Click Here to Zoom |
Figure 4: Healing process of a Buerger’s patient on day 10 postoperatively. |
 Click Here to Zoom |
Figure 5: Healing process of a Buerger’s patient at 3rd year after sympathectomy. |
Discussion
Due to the role of vasospasticity and increase in sympathetic tone in etiopathogenesis of both and the fact that they are known to be effective in their treatment, we examined the results of sympathectomy with VATS, which is considered the most effective option in surgery in both groups of patients. During an attack, radial and ulnar pulses are clearly received. It is accepted by all authorities that the main pathology begins with vasoconstriction in arterioles and metarterioles [3,8,9]. In Buerger patients, histopathological disorders are constantly present. In the clinic, it is in a state of attacks, often starting at the tip of the nail and can deepen to gangrene. Doppler and angiography are important in diagnosis, especially in differentiation with atherosclerosis. In addition, a positive cold test indicates the place of sympathetic activity in both diseases and sympathectomy in treatment [10-12]. In our study, Raynaud patients were diagnosed with cold water testing technique and Buerger patients were diagnosed with angiography.In studies, 2% of Buerger patients were women, and in Raynaud patients, this ratio was 85% [3,9]. In contrast to the literature in our study, 21 (60%) of the 35 patients with Raynaud’s were male and 14 (40%) were female. Of the 10 patients with Buerger, 8 (80%) were male and 2 (20%) were female. Buerger patients were often 25-40 years old, and Raynaud was of asthenic, anemic types under the age of 40 [3,9] while the mean age in our group was 39.5 years old.
The main factor in treatment is the cessation of smoking. In his study, Van Damme [6] showed the importance of quitting smoking before treatment, 16 of 29 Buerger patients had good postoperative results, and 9 of these patients stopped smoking. In our study, the return symptoms were accelerated in both Raynaud and Buerger patients who continued to smoke. In our series, 27 patients smoked a mean of 15 packs/year, and 11 patients quit smoking. In follow-up, we noted that 4/10 (40%) of Buerger patients and 12/35 (33%) of Raynaud patients continued to smoke.
In the medical treatment of Raynaud’s and Buerger diseases, cold protection consists of sedatives, peripheral vasodilator drugs, such as calcium channel blockers and pentoxyphiline, and the cessation of nicotine [3,9]. We performed 75 endoscopic thoracic sympathectomies (ETS) on a total of 45 patients who did not respond to medical treatment. We performed bilateral sympathectomy on 30 of the 35 patients with Raynaud’s. The rest of 5 patients and 10 patients with Buerger had sympathectomy on the side of the symptom and/or ulcer. In the first sympathectomy session, bilateral sympathectomy can be performed, considering progression and continuity of sympathetic hyperactivity, as well as the operation can be performed only on the side of the findings. Thoracoscopic technique shows differences. In the use of clips compared to the cauterization method, there may be a dislocation of the clip, a incomplete clipping of the chain, and inappropriate ganglion localization. In patients, the goal is complete sympathetic blockade and the risk that the clip may fail by sliding should not be taken. Although it is not in routine use, there are reports about chemical symphatectomy [13], in our study, we applied thoracic sympathectomy to all of our patients with cauterizing via thoracoscope.
In different publications, authors have reported that they cauterize T2-4 level ganglia and considered them appropriate when evaluating their results [12-15]. In our study, 27 (60%) of 45 patients had T2-3-4 ganglia, and 18 patients (40%) had T2-3-4-5 the ganglia were cauterized, and at these levels it was found that complete sympathetic blockade of the upper extremities could be achieved. In our study, a mean value was found by measuring heat on the diseased side, preoperative five fingers of each hand separately, and this value was compared with the postoperative one. The increase in temperature of 1.3&;ordmC was found to be significant. This suggests that sympathectomy is effective at the levels administered.
The most common complication associated with the procedure was minimal pneumothorax, was also top in our study with 16 patients (21.3%). In one patient developed bronchospasm and respiratory failure and required 16 hours of mechanical ventilation support (2.2%). Looking at the duration of hospital stays, it was recorded as the shortest 1 and the longest 18 days. The mean was 3.4 days. Eleven patients (24.4%) were discharged on the first day of postoperative and 7 patients were discharged on the second day. We believe that patients who have not trouble checking after the procedure can be discharged on the day of surgery, so VATS sympathectomy can be performed in the form of daily surgery.
A study by Lorenzo et al [14], found no satisfactory results after sympathectomy of patients with Buerger. In contrast, success in ulcer healing was rated at 85% and in symptom improvement at 14% in a literature survey involving 30 years in the publications of Coveliers et al [16]. In the early period after sympathectomy, local blood flow increases by 8 times and provides an increase in heat, and the O2 gradient increases due to the opening of shunts. But after 2-3 months, when the late effects are examined, they fall to the preactive level and relapse occurs [12]. The 100% recovery rate of initial ulcers should also not be decimated. Our follow-up period is between 1 and 60, a median of 32 months, and the return of symptoms is meanly 8 months. This non-mortal procedure has more than 70% complete symptom improvement in Raynaud’s patients and 100% success in target finger improvement in ulcerated patients. In addition, in terms of improving quality of life, our overall success is above 95%, even a subjective assessment.
In conclusion bilateral or one-sided blockage of the thoracic ganglia is achieved fully via thoracoscopic sympathectomy technique. It can be proved that the ganglia have been deactivated (sympathectomy) by digital temperature measurement. The changes in the temperature clearly show the circulation of the skin. Although the symptoms of some patients with Raynaud’s disease return after the VATS sympathectomy, there is a considerable decrease in their intensity and frequency; the success of the treatment is; 70% full and 30% partial recovery in the symptoms, 100% recovery in the chronic ulcers and 33% recovery in the overall ulcers. Thoracoscopic sympathectomy can be advised for all of the Raynaud cases. The success of VATS sympathectomy for Buerger’s is 100% recovery of chronic ulcers and 40% recovery of the overall ulcers. VATS sympathectomy is suitable for the Buerger’s patients with ulcer. Referring to our study we can say that among 30-40% of the patients with Buerger’s and Raynaud’s, the patients can be free of disease and saved from amputation with the help of VATS sympathectomy. Cauterization of T2-3-4 ganglia seems enough for a satisfying result.
Sympathectomy via VATS increases the quality of life considerably in Buerger’s and Raynaud’s and should be considered a final choice for those who are resistant to medical treatment and have severe symptoms and/or serious complications with an impaired quality of life. Although the possibility of the recurrence especially in symptoms must be kept in mind, VATS sympathectomy is a harmless surgical operation without mortality and with tolerable minor complications, short hospitalization after a short and minimally invasive surgery, it is a comfortable treatment period and does not exhaust the patient.
Declaration of conflicting interests
The authors declared no conflicts of interest with respect to the authorship and/or publication of this article.
Funding
The authors received no financial support for the research and/or authorship of this article.
Ethics approval
The study was approved by the Ethic Committee of Vakıf Gureba Training and Research Hospital, registered by 2010-68/22.
Authors’ contribution
UT; collected/analysed data, and wrote the whole manuscript.
Reference
1) Buerger L. Thromboangiitis obliterans: A study of the vascular lesions leading to presenile spontaneous gangrane. Am J Med Sci 1908; 136: 567-80.
2) Winiwarter V. Ueber eine eigenthumliche Form von Endarteritis und Endophlebitis mit Gangren des Fusses. Arch Klin Chir 1879; 23: 202-26.
3) Musa R, Qurie A. Raynaud Disease. [Updated 2020 Nov 19]. In: StatPearls Publishing; 2021 Jan. Available from: https://www.ncbi.nlm.nih.gov/books/NBK499833/
4) Lewis T. Experiments relating to the peripheral mechanism involved in spasmodic arrest of the circulation in the fingers, a variety of Raynaud’s disease. Heart 1929; 15: 7-101.
5) Hellon RF. Local effects of temperature. Brit Med Bull 1963; 19: 141.
6) Van Damme H, De Leval L, Creemers E, Limet R. Thrombangitis Obliterans (Buerger Disease): Still a limb threatening Disease. Acta Chir Belg. 1997; 97: 229-36.
7) Belch J, Carlizza A, Carpentier PH, Constans J, Khan F, Wautrecht JC et al. ESVM guidelines - the diagnosis and management of Raynaud’s phenomenon. Vasa 2017; 46: 413-23.
8) Hughes J. Endoscopic sympathectomy. Proc R Soc Med 1942; 35: 585-6.
9) Galmer A, Weinberg I. Thromboangiitis Obliterans (Buerger’s Disease) Expert Analysis. ACC. 2019 Available: https://www.acc.org/latest-incardiology/articles/2019/10/21/15/05/thromboangiitis -obliterans.
10) Talwar S, Prasad P. Single-stage lumbar sympathectomy and omentopexy: a new surgical approach towards patients with Buerger’s disease. Trop Doct 2001; 31: 73-5.
11) De Giacomo T, Rendina EA, Venuta F, Lauri D, Mercadante ES, Anile M et al. Thoracoscopic sympathectomy for symptomatic arterial obstruction of the upper extremities. Ann Thorac Surg 2002; 74: 885-8.
12) Maga P, Kuzdzal J, Nizankowski R. Long term effects of thoracic sympathectomy on microcirculation in the hands of patients with primary Raynaud Disease. J Thorac Cardiovasc Surg 2007; 133: 1428-33.
13) Cacione DG, Moreno DH, Nakano LCU, Baptista-Silva JCC. Surgical sympathectomy for Buerger’s disease. JRSM Open. 2017; 8: 1-8. Doi: 10.1177/2054270417717666.
14) Di Lorenzo N, Sica GS, Sileri P, Gaspari AL. Thoracoscopic Sympathectomy for Vazospastic Diseases. JSLS 1998; 2: 249-53.



