

2Department of Thoracic Surgery, Sureyyapasa Chest Disease and Thoracic Surgery Training and Research Hospital, Istanbul, Turkey
3Department of Thoracic Surgery, Burdur State Hospital, Burdur, Turkey
4Department of Emergency Medicine, Merkezefendi State Hospital, Manisa, Turkey DOI : 10.26663/cts.2022.007
Summary
Background: Not all of the N1 lymph nodes are routinely dissected during surgical resection of nonsmall cell lung cancer (NSCLC). The aim of our study is to determine the risk factors for N1 lymph node metastasis in NSCLC with peroperative dissection.Materials and Methods: Patients who underwent lung resection in our hospital between September 2014 and April 2016 were retrospectively included in this study. Resected specimens were dissected in the operating room by the surgeon before being put into formaldehyde solution. Patients were divided into three groups: with a single positive N1 node (Group 1), with multiple positive N1 nodes (Group 2), and with single or multiple positive N1 nodes and incidentally positive N2 nodes (Group 3).
Results: Fifty patients were included (46 males, 4 females). Univariate analysis showed significant correlation between N1 positivity and left-sided tumor, left central mass, squamous cell carcinoma, maximum standardized uptake (SUVmax) on positron emission tomography (PET/CT), pneumonectomy, and tumor size (p < 0.05). Logistic regression showed that the risk of N1 involvement was higher for squamous cell carcinoma compared to adenocarcinoma in all three groups.
Conclusions: Left central mass, squamous cell carcinoma, SUVmax ≥ 10, uptake in hilar lymph nodes on PET-CT, and tumor diameter > 3.5 cm correlated with single or multiple positive N1 nodes in our study. Specimen dissection in patients with such preoperative findings could improve the accuracy of pathological nodal staging, thus refining the assessment of prognosis and selection of patients who would benefit from adjuvant therapy.
Introduction
In the 8th edition of the TNM Staging System for lung cancer, there are changes in the classification of T and M groups. The changes in these two groups affect prognosis [1]. However, one of the most reliable factors in the prognosis of lung cancer patients and in determining optimal treatment options is the lymph node status. A publication, which is also mentioned in the 8th TNM edition manual, propose changes to N classifications [2].In the surgical treatment of non-small cell lung cancer (NSCLC), mediastinal lymph node dissection is performed after resection. However, not all of the N1 lymph node stations are routinely dissected during surgery. In order to determine the correct stage, immediately after the surgery, the N1 lymph nodes on the lesion may be dissected by the surgeon before the specimens are put into formaldehyde solution and sent to pathology. Dissection of all N1 lymph nodes during an operation is inconvenient, because this may extend the duration of the operation and jeopardize the surgery. The idea behind dissecting the specimens before placing them into formaldehyde solution is that formaldehyde may affect the structure of lobes, reduce their volume, and cause possible false negative results in N1 lymph nodes. For this reason, we believe that the dissection of N1 nodes of the peripheral zone (stations 12-14) should be performed by the surgeon, not the pathologist.
This study aimed to determine the risk factors for involvement of one or more N1 lymph nodes of the hilar/interlobar (stations 10 and 11) as well as peripheral (stations 12, 13 and 14) zone acquired by dissection of fresh specimens prior to formaldehyde fixation.
Methods
Patient selectionAfter giving informed consent, patients who underwent pulmonary resection for NSCLC with thoracotomy or video-assisted thoracoscopic surgery (VATS) between September 2014 and April 2016 were retrospectively included in the study. All patients had positron emission tomography (PET / CT) scans before the operations. All patients were also diagnosed with NSCLC before the surgery. Patients with known N2, synchronous tumor, distant organ metastasis; who had undergone sublobar resection, neoadjuvant chemotherapy, and/or radiotherapy; who had wedge resection during the lobectomy; or who had a T4 tumor and/or those on whom a complete resection could not be performed were not included in the study. Approval was obtained from scientific research committee of University of Health Sciences, Istanbul Sureyyapasa Chest Diseases and Thoracic Surgery Research and Training Hospital.
Technique
Mediastinoscopy was performed at the time of resection on patients suspected to be N2-positive. These include patients who have a ≥ 2.5 maximum standard uptake value (SUVmax) at mediastinal lymph nodes on PET/CT or centrally located tumors. Pulmonary resection was performed via VATS or thoracotomy in patients who had no clinical evidence of N2 disease. After the resection, the lobectomy or pneumonectomy specimens were dissected in another area in the operating room without being placed in the formaldehyde solution. Care was taken to preserve the integrity of the lesion and total removal of the N1 lymph nodes. The dissection was performed from the center to the periphery. The parenchyma over the bronchus was opened by beginning with the bronchus located in the most central duct (right or left main bronchus for pneumonectomy, lobar bronchus for lobectomy) to the periphery. The bronchus was not cut during any dissection. The N1 lymph nodes located between the bifurcation regions of the bronchi were dissected. The Mountain-Dressler nodal map was used to identify lymph node stations and assign the individual resected nodes [3]. All of the lymph nodes were dissected one by one and put into separate containers filled with formaldehyde to send to pathology.
Patient groups
The patients were evaluated in three groups. The first group included patients who were identified by the dissection as being positive for only a single N1 node. The second group included patients identified by the dissection as having more than one N1-positive node. The third group included the patients with single or multiple positive N1 nodes and incidentally positive N2 nodes. The numbers of patients in each group was determined according to the distribution of lymph node status during the study period.
The following parameters were included in the analysis: Age, sex, side, systemic disease, history of previous surgeries, history of smoking, forced expiratory volume (FEV1), tumor localization and diameter on computed tomography (CT), tumor uptake and hilar lymph node involvement on PET/CT (SUVmax ≥ 2.5), tumor type, tumor differentiation, tumor grade, invasion of visceral pleura, mediastinoscopy result, N1 dissection, N1 positivity status, N2 positivity status, N1 positivity according to different resected segments and centrally located tumors, resection type, duration of operation, duration of dissection, tumor stage according to the 8th TNM Staging System, morbidity, 30-day mortality [1].
In tumors involving more than one lung segment, the segment where the tumor occupies a larger proportion was chosen. Masses the origin of which could not be precisely determined due to the centralization of the mass were named central masses. Tumor SUVmax cut-off value was determined as 10 and above, vs. below 10 according to the median value of SUVmax. Plus tumor diameter cut-off value was determined as 3.5 cm according to the median value of the tumor.
From the perspective of localization, it was observed that N1 positivity was more frequent in the left upper lobe apicoposterior segment, as well as in cancers involving both the left upper lobe apicoposterior and anterior segments, those involving a left central mass, and those involving central masses (left and right) than any other groups. Therefore, these four groups were evaluated separately.
In the evaluation of dissected N1 lymph node results, the number of positive N1 lymph nodes (LNs) was determined and the lymph node ratio (LNR: Positive lymph nodes/sampled lymph nodes) was calculated [4].
Statistical Analysis
The data obtained in the study were analyzed using SPSS (Statistical Package for Social Sciences) for Windows 22.0 software. Number, percentage, mean, and standard deviation were used as descriptive statistics. Logistic regression analysis was applied to examine the association of independent variables (predictors) with our dichotomous dependent variable (N1 positivity). Any variable whose univariable test has a p-value less than 0.20 or 0.25 along with all variables of known clinical importance was included in the multivariable model. The findings were evaluated with a 95% confidence interval and a 5% significance level.
Results
Fifty patients were included in the study. Forty-six of the patients were male and four were female. Demographic information about the patients is given in table 1.Table 1: Patient characteristics.
PET/CT scans showed that 13 patients had hilar lymph node involvement, seven patients had mediastinal lymph node involvement, eight patients had both types, and 22 patients had none of these. In patients with hilar lymph node involvement on PET/CT, the false negative rate for N1 was 27.5%, and the false positive rate was 57.1%. Six patients underwent resection with VATS, while two patients had en-bloc chest wall resection. Sleeve resection was performed in three patients. Of the 24 patients who underwent right-sided intervention, there were patients with upper left lobectomy (46%), right lower lobectomy (21%), middle lobectomy (17%), superior bilobectomy (8%), inferior bilobectomy (4%), and pneumonectomy (4%). Of the 26 patients that underwent left-sided intervention, there were patients with upper lobectomy (46%), pneumonectomy (31%), and lower lobectomy (23%).
The average age of the participants was 61.7 ± 8.8 years (Table 2).
Table 2: Descriptive statistics.
Mediastinoscopy was performed in 31 patients. The mean duration of operation, including the duration of mediastinoscopy during the same anesthesia, was 234.2 ± 77.6 min, and the mean duration of nodal dissection of the resected specimen was 12.1 ± 3.6 min. The average duration of hospital stay was 6.5 ± 3.33 days (range 1-18 days). Five patients (10%) had prolonged air leakage, one patient (2%) had pneumonia, one patient (2%) had chylothorax, and one patient (2%) had bronchopleural fistula. Two patients (4%) underwent re-thoracotomy due to hemorrhage. There was no postoperative mortality. When evaluated in terms of tumor type, 24 patients were identified as having squamous cell carcinoma (SCC), 24 had adenocarcinoma, one had large cell carcinoma, and one had adenosquamous carcinoma.
Four hundred and eighty-eight N1 lymph node stations (10-14) were dissected in the study. Fifty-three of them had N1 lymph node metastasis (Table 3). The average number of N1 lymph node stations dissected from resected specimens was 9.76 ± 3.32 (range 5-19), while the LNs were 2.73 ± 1.59 (range 0-6). The LNR was 0.10. Seventy percent of N1 positive patients had direct lymph node invasion.
Table 3: N1 positive lymph node stations.
Fifteen patients were in group 1, while 15 were in group 2, and 20 were in group 3. Tables 4-6 show the relationships of statistically significant variables prior to logistic regression analysis to determine the risk factors for N1 positive in all three groups. Logistic regression analysis showed that likelihood of N1 positivity in cases with SCC was higher than in cases with adenocarcinomas separately for each group (p = 0.007, 0.004, 0.003; OR: 10.587, 11.000, 13.472; 95%CI: 1.90-58.92, 2.10-57.50, 2.35-76.95 respectively) and for the whole study group (p = 0.001; OR: 9.167; 95% CI: 2.38-35.30).
Table 4: Univariate analysis in group 1.
Table 5: Univariate analysis in group 2.
Table 6: Univariate analysis in group 3.
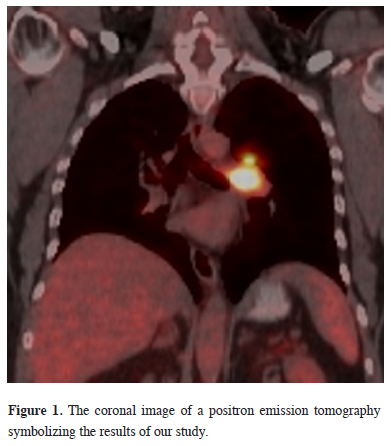
According to the results of our study, a typical PET/CT image example of a patient who may benefit from lymph node dissection is shown in figure 1.
 Click Here to Zoom |
Figure 1: The coronal image of a positron emission tomography symbolizing the results of our study. |
Discussion
The debate over the prognostic significance of N1 involvement is ongoing, and the variability of survival in these patients indicates the need to include a more detailed N1 status in predicting prognosis. It is most likely that the varied number of N1 positive lymph nodes causes this inconsistency. Therefore in our time, careful N1 lymph node dissection is becoming more important to better predict prognosis and understand the disease, plus it may affect the stage in upcoming TNM classifications [2].In a study by Maeshima et al, the researchers suggested routinely sampling lymph nodes 13 and 14 [5]. Another study indicating the prognostic significance of LNs in N1 disease is described by Jonnalagadda et al [6]. They showed that a greater number of N1 LNs was associated with worse lung cancer-specific (P < 0.0001) and overall (P < 0.0001) survival. As the number of positive N1 lymph nodes increase, survival decreases, and as a result, N1 positivity was suggested to be an independent prognostic factor.
Although LNs appear to be important in prognosis, some authors have emphasized that LNR is more critical than LNs in determining prognosis [7-9]. In the study of Matsuguma et al, the 5-year survival rate for N1 disease was 52.2%, 54.3% according to LNs, and 58.8% according to LNR [7]. In the same study, they reported that LNR is superior to LNs, both are more significant than N1 in the TNM classification, and both may be present in future TNM classifications. Results of a meta-analysis of 6130 diseases, which was published in 2016, showed that LNR is an important determinant in survival and cancer relapse [8]. All of these studies agree that a higher LNR was associated with a worse survival. Plus, it was shown that patients with a ≤ 0.15 LNR had the best survival, whereas in patients with a LNR > 5 survival was the worst [4]. In our study LNR was calculated as 0.10. It seems that by increasing the number of lymph nodes dissected, LNR is better calculated.
As an outcome, the significant differences in the survival of patients without N2 disease may arise from LNs and LNR factors. Therefore, N1 lymph nodes should be carefully dissected to calculate LNs and LNR correctly in patients with NSCLC.
In the literature, N1 lymph node metastasis has been reported to be more frequent in adenocarcinomas than in SCC [10,11]. Nakao et al reported that N1 lymph node involvement was seen more frequently in adenocarcinomas than in SCC [11]. In another study LNs was significantly higher, and tumors recurred more frequently in adenocarcinoma cases than in SCC cases. This applies to tumor metastases to N1 lymph nodes, not direct invasion.
However, for direct invasion the situation seems to be different. In a study, it is stated that SCC prefer a direct invasion as it arises more frequently in the wall of the lobar bronchi and is associated with a higher incidence of direct lymph node involvement compared with the usually peripherally located adenocarcinoma [12]. In another study by Varlotto et al investigating the effect of resection in patients with NSCLC on relapse and general survival, N1 lymph node involvement was higher in SCC than in adenocarcinoma [13]. In our study, the probability of N1 lymph node metastasis in SCC was higher than in adenocarcinoma. This difference can too be explained by the fact that a higher number of our patients with direct lymph node invasion had SCC.
In left-sided stage 1 NSCLC patients, survival rate is not adequate [14]. Particularly, survival of patients with left lower lobe cancers is lower than that of patients with other lobe cancers [15]. It has been suggested in the literature that this may be due to the presence of right paratracheal lymph node involvement in left-sided lung cancers [16]. High involvement of the N1 lymph nodes in left-sided NSCLC may also contribute to this situation [17]. In a study it is stated that left-sided tumors tend to directly invade or reach the hilar nodes more easily [12]. In our study, the likelihood of having N1 positivity in left-sided tumors was higher than in the right.
Tumor location may affect pN1 upstaging during operations in patients with NSCLC [18]. Central tumors tend to have more positive N1 lymph nodes along with them, plus they may have retrograde lymphatic spread to other lobes. In our study, N1 positivity was seen in all patients who underwent pneumonectomy (n = 9). Four of these patients (44.4%) were found to have N1 positivity in a different lobe from where the tumor exists. These cases were a patient with a left lower lobe tumor and N1 positivity at the left upper lobe apicoposterior segment, a patient with a right upper lobe tumor and N1 positivity at the right middle lobe lateral segment, a patient with a left upper lobe tumor and N1 positivity at the left lower lobe in an anterobasal segment, and a patient with a left upper lobe tumor and N1 positivity at the left lower lobe laterobasal segment.
PET/CT scanning during the preoperative period has great importance. This method is especially highly sensitive and specific in detecting mediastinal lymph node metastasis. In a recent study, the value of PET/CT in detecting prognosis was emphasized; however, the requirement for pathological diagnosis was still described [19]. The benefits of PET/CT are much lower in the N1 lymph nodes. The method is useful in detecting hilar lymph nodes, but its value in detecting interlobar, lobar, segmental, and subsegmental lymph nodes is low. In our study, PET/CT scans showed that a mass SUVmax value greater than 10 and hilar lymph node involvement in the N1+ and N1+, N2- groups was significant.
Tumor localization is also an important factor in evaluating the presence of N1 in the preoperative period. In a previous study, unexpected N1 disease-related progression of stage occurred in 1/3 of central tumor patients, and tumor localization was found to be the only independent variable in pathological N1 stage increase [20]. In our study, central tumor presence for all three groups was significant in terms of N1 positivity.
There are publications in the literature about the relationship between tumor diameter and N1 positivity. In a study by Zhang et al., the researchers investigated the determinants of lymph node involvement in small and peripheral NSCLC patients [21]. In our study, multivariate analysis showed that the probability of lymph node metastasis in patients with a tumor diameter greater than 10 mm was significantly higher than in other patients. In our study, the clinical and pathological tumor size was significantly higher in groups 1 and 2.
There are different practices about specimen handling throughout the globe. In some institutions the specimens are put into formaldehyde solution and sent to pathology while in others they are sent fresh. The reason why the dissection was done by a surgeon instead of a pathologist is that in our institution the specimens are not sent fresh to pathology but are put into formaldehyde solution first.
Limitations of the study
No significant survival study could be performed due to the short study period. Parameters such as 5-year survival rate, disease-free survival, and tumor relapse have not been investigated. Plus, due to the many criteria that reduce the sample size, dissection could be performed only on a limited number of lesions. However, this article contains only preliminary results and studies are still continuing. This study contains only one clinical center. However, our hospital is a reference center for lung cancer, accepting patients from many different places.
In conclusion preliminary results show that dissection of lymph nodes may be useful for both lung sides but especially for left central masses. In cases with SCC, involvement on PET/CT with mass SUVmax above 10, hilar LAP involvement on PET/CT, and tumor diameters over 3.5 cm, performing dissection may be useful for improved detection of N1 and multi-N1 positivity and may provide prognostic information.
Declaration of conflicting interests
The authors declared no conflicts of interest with respect to the authorship and/or publication of this article.
Funding
The authors received no financial support for the research and/or authorship of this article.
Ethics approval
The study was approved by the scientific research committee of University of Health Sciences, Istanbul Sureyyapasa Chest Diseases and Thoracic Surgery Research and Training Hospital (2021/223).
Authors’ contributions
TD; Conceived and designed the analysis, collected the data, contributed data/analysis tools, VB; Conceived and designed the analysis, co-wrote the paper, SC; Contributed data, co-wrote the paper, SD; Performed the analysis, co-wrote the paper, AM; Contributed data, SK; Contributed data, LA; Contributed data, CT; Contributed data.
Reference
1) Goldstraw P, Chansky K, Crowley J, Rami-Porta R, Asamura H, Eberhardt WE et al. The IASLC Lung Cancer Staging Project: Proposals for Revision of the TNM Stage Groupings in the Forthcoming (Eighth) Edition of the TNM Classification for Lung Cancer. J Thorac Oncol 2016; 11: 39-51.
2) Asamura H, Chansky K, Crowley J, Goldstraw P, Rusch VW, Vansteenkiste JF et al. The International Association for the Study of Lung Cancer Lung Cancer Staging Project: Proposals for the Revision of the N Descriptors in the Forthcoming 8th Edition of the TNM Classification for Lung Cancer. J Thorac Oncol 2015; 10: 1675-84.
3) Mountain CF, Dresler CM. Regional lymph node classification for lung cancer staging. Chest 1997; 111: 1718-23.
4) Jonnalagadda S, Arcinega J, Smith C, Wisnivesky JP. Validation of the lymph node ratio as a prognostic factor in patients with N1 nonsmall cell lung cancer. Cancer 2011; 117: 4724-31.
5) Maeshima AM, Tsuta K, Asamura H, Tsuda H. Prognostic implication of metastasis limited to segmental (level 13) and/or subsegmental (level 14) lymph nodes in patients with surgically resected nonsmall cell lung carcinoma and pathologic N1 lymph node status. Cancer 2012; 118: 4512-8.
6) Jonnalagadda S, Smith C, Mhango G, Wisnivesky JP. The number of lymph node metastases as a prognostic factor in patients with N1 non-small cell lung cancer. Chest 2011; 140: 433-40.
7) Matsuguma H, Oki I, Nakahara R, Ohata N, Igarashi S, Mori K et al. Proposal of new nodal classifications for non-small-cell lung cancer based on the number and ratio of metastatic lymph nodes. Eur J Cardiothorac Surg 2012; 41: 19-24.
8) Li Q, Zhan P, Yuan D, Lv T, Krupnick AS, Passaro A et al. Prognostic value of lymph node ratio in patients with pathological N1 non-small cell lung cancer: a systematic review with meta-analysis. Transl Lung Cancer Res 2016; 5: 258-64.
9) Sun G, Xue L, Wang M, Zhao X. Lymph node ratio is a prognostic factor for non-small cell lung cancer. Oncotarget 2015; 6: 33912-8.
10) Anami K, Yamashita S, Yamamoto S, Chujo M, Tokuishi K, Moroga T et al. Contralateral mediastinal lymph node micrometastases assessed by video-assisted thoracoscopic surgery in stage I non-small cell left lung cancer. Eur J Cardiothorac Surg 2013; 43: 778-82.
11) Kudo Y, Saji H, Shimada Y, Nomura M, Usuda J, Kajiwara N et al. Do tumours located in the left lower lobe have worse outcomes in lymph node-positive non-small cell lung cancer than tumours in other lobes? Eur J Cardiothorac Surg 2012; 42: 414-9.
12) Marra A, Hillejan L, Zaboura G, Fujimoto T, Greschuchna D, Stamatis G. Pathologic N1 non-small cell lung cancer: correlation between pattern of lymphatic spread and prognosis. J Thorac Cardiovasc Surg 2003; 125: 543-53.
13) Varlotto JM, Yao AN, DeCamp MM, Ramakrishna S, Recht A, Flickinger J et al. Nodal stage of surgically resected non-small cell lung cancer and its effect on recurrence patterns and overall survival. Int J Radiat Oncol Biol Phys 2015; 91: 765-73.
14) Hata E, Hayakawa K, Miyamoto H, Hayashida R. Rationale for extended lymphadenectomy for lung cancer. Theor Surg 1990; 5: 19-25.
15) Kuroda H, Sakao Y, Mun M, Uehara H, Nakao M, Matsuura Y et al. Lymph Node Metastases and Prognosis in Left Upper Division Non-Small Cell Lung Cancers: The Impact of Interlobar Lymph Node Metastasis. PLoS One. 2015; 10: e0134674.
16) Gunluoglu MZ, Demir A, Turna A, Sansar D, Melek H, Dincer SI et al. Extent of lung resection in non-small lung cancer with interlobar lymph node involvement. Ann Thorac Cardiovasc Surg 2011; 17: 229-35.
17) Tachi R, Hattori A, Matsunaga T, Takamochi K, Oh S, Suzuki K. The impact on the prognosis of unsuspected N2 disease in non-small-cell lung cancer: indications for thorough mediastinal staging in the modern era. Surg Today 2017; 47: 20-6.
18) Decaluwé H, Stanzi A, Dooms C, Fieuws S, Coosemans W, Depypere L et al. Central tumour location should be considered when comparing N1 upstaging between thoracoscopic and open surgery for clinical stage I non-small-cell lung cancer. Eur J Cardiothorac Surg 2016; 50: 110-7.
19) Park S, Cho S, Yum SW, Kim K, Jheon S. Comprehensive analysis of metastatic N1 lymph nodes in completely resected non-small-cell lung cancer. Interact Cardiovasc Thorac Surg 2015; 21: 624-9.



