

2Department of Thoracic Surgery, Ege University School of Medicine, Izmir, Turkey
3Department of Thoracic Surgery, University of Health Sciences, Bozyaka Education and Research Hospital, Izmir, Turkey DOI : 10.26663/cts.2023.001
Summary
Background: In this study, the factors that had an effect on the recovery of respiratory functions of the patients with chest trauma were investigated, and it is aimed to question the adequacy of the follow-up and rest periods with a different method.Materials and Methods: One hundred and eighty patients with chest trauma hospitalized in our thoracic surgery department between August 2018 and December 2019 were analyzed. The effective factors on their recovery to normal respiratory functions were investigated using “Peak Expiratory Flow-meter” (PEF-meter). PEF values were recorded on the first three days of hospitalization and on the 10th, 40th and 70th days after their discharges.
Results: We examined when the chest trauma patients were able to reach a PEFR value of 80% (PEF80) as done in bronchial asthmatics. Pneumothorax, lung laceration, presence of pneumomediastinum and tube thoracostomy were found to delay achieving a PEF80. It was found that the location of the fracture, rather than the number of rib fractures, was effective in improving respiratory functions. Non-smokers were seen to have a higher capacity to return to normal respiratory activity after trauma.
Conclusions: In case of fractures occurring on the anterior and lateral of the ribs and in the situation of the presence of pneumothorax, pneumomediastinum, lung laceration, tube thoracostomy and smoking history pain management and follow-up should be handled more detailed. It should be taken into account that these cases may require longer rest period and disability/incapacity reports should be prepared bearing this in mind.
Introduction
Today, traumas are increasing due to both the increase in transportation opportunities and higher violence rate. Trauma requires hospitalization at every stage of life and is one of the main causes of disability. 10-15% of trauma patients’ admissions are due to chest injuries, and the resulting pathologies are related to approximately 25% of mortalities [1-3]. Pneumothorax, hemothorax, lung contusion and rib fracture are the frequently encountered pathologies in chest trauma cases [4]. Frequently observed rib fractures cause chronic pain-related problems [5].The treatment of most chest trauma cases do not call for a major surgery and more than 80% of the cases can be treated with pain control, effective respiratory physiotherapy and tube thoracostomy [3]. However, those who leave the hospital following their treatment may experience respiratory function limitation, which affects their quality of life [6,7]. Quantitative data are needed to measure the effect of trauma on respiratory functions and to objectively evaluate the treatment and follow-up approach [7]. “Peak Expiratory Flow” (PEF) measurement is a valuable method used to assess respiratory function. In monitoring the severity, course and response to treatment of the disease, the importance of daily recording of PEF value in bronchial asthmatics has long been known [8,9]. In addition to the factors that prevent the expansion of the thoracic cage and hinder respiratory muscle function, many factors such as any pathology that obstructs the airways and damage to the central nervous system can cause changes in the PEF value [8].
A thoracic surgeon should be able to competently treat a trauma patient, in addition to managing and monitoring the possible complications in the post-discharge period. The hospitalization period of trauma patients is mostly determined with the ending doctor and hospital requirement. Thinking differently from this customary condition, we aimed to categorize the cases with chest trauma using a quantitative method based on the question: “Which patients should be followed up for longer period of time?”. In this study, bearing in mind that PEF value is affected by chest wall pathologies, we performed the measurable follow-up of patients with chest trauma using PEF-meter device which measures the peak flow velocity in chest trauma patients. We also aimed to reveal the pathologies that prevented the patients initiated an inpatient treatment and later followed up in the outpatient clinic from achieving the expected respiratory function value. It was also aimed to investigate whether the data to be obtained would be a determining factor in terms of both patient follow-up and rest periods to be given.
Methods
The study was prospectively carried out with the participation of 180 chest trauma patients. The patients were hospitalized in our thoracic surgery department and also followed up in the outpatient clinic later between the dates of August 2018 and December 2019. All patients were included in the study after reading and confirming the “informed voluntary consent form”. The study was initiated with the approval letter obtained from the Ege University School of Medicine Ethics Committee dated 19.06.2018 and decision number 18-6.1/37.Those excluded from the study were as follows: the patients hospitalized on the second and following days of their trauma; those with mental or auditory disabilities that prevent the use of PEF-meters, those with cranial traumatic injuries with altered consciousness, those with lip, tongue, and facial injuries; those having underwent surgical intervention outside our hospital and referred to us; those who underwent surgery under general anesthesia due to trauma in our hospital; severe multisystem injuries requiring intensive follow-up of other clinics and lastly the cases under 18 years of age.
PEF measurements were made on the first 3 days of hospitalization and on the 10th, 40th and 70th days post discharge in accordance with the method in the outpatient clinic control. The value measured on the first day of the patient admissions was recorded as “clinical value 1st day” (CV1) then 2nd day (CV2) and 3rd day (CV3), and also the value measured in the outpatient follow-up on the 10th day of the discharge was recorded as the “outpatient value 10th day” (OV10), then as 40th day (OV40) and as 70th day (OV70).
Measurements were made using the “MSA-100 Peak Flow Meter” (patented by Beijing M&B Electronics Instruments Co Ltd, Beijing, People’s Republic of China) digital PEF-meter. With personalized mouthpieces, the device was prepared for multiple uses. The use of the PEF-meter device with the appropriate technique was explained to all participants.
The measurements were made at the same time of day and in body position (feet hanging off the side of the bed and in a way to let a comfortable breathing position). Three consecutive PEF measurements were made each time and the highest one was recorded. The applied treatments were standardized with a drug group consisting of analgesics, mucolytics, antibiotics and proton pump inhibitors. The surgical procedure of those who needed tube thoracostomy was performed using the same method, from the same site. In addition to the demographic data of the patients, such data as trauma mechanism, injury site, radiological findings, intervention, smoking habit, length of stay were analyzed. These variables were evaluated according to the PEF levels, which should be appropriate for the age and height of the subjects.
Statistical Analysis
Categorical data were expressed as numbers and percentages. Numerical variables were summarized as mean ± standard deviation when normally distributed, and as median (min, max) when not normally distributed. Cross-tables were created for group comparison in categorical data and chi-square analysis was performed. Comparisons between the two groups were made using the t-test for those with normal distribution in terms of numerical values, and using the Mann-Whitney U test for those who did not show normal distribution. The p < 0.05 was accepted as statistically significance.
Results
Of the 180 patients, 145 (80.6%) were male and 35 (19.4%) were female, with a mean age of 52.67 ± 18.27 (18-93). In the series of 77 (42.7%) active smokers, there were 57 (31.7%) non-smokers and 46 (25.6%) ex-smokers. Comorbidities were observed in 64 of the cases (35.5%) most of which were in the form of hypertension (35 cases), diabetes mellitus (27 cases), coronary artery disease (23 cases), and chronic obstructive pulmonary disease (8 cases).One hundred fifty-six (86.7%) of the subjects in the study had blunt injuries, while 24 (13.3%) had penetrating injuries. When analyzed according to subgroups; falling down was observed in 72 (40%), in-vehicle traffic accidents (IVTA) in 45 (25%), and sharp object injuries in 20 (11.1%) cases and in addition, motorcycle accidents (8.3%), out-vehicle traffic accident (OVTA) (7.2%), assault (3.9%), crushing (2.2%) and firearm injuries (FAI) (2.2%) were also observed.
Additional injuries requiring consultation of other clinics were also examined. Eight (4.4%) patients with cranial injuries were not excluded from the study as they did not cause problems in clinical perception and use of PEF-meters. Six of the cases (3.3%) had abdominal injuries not requiring surgery. In 32 patients (17.8%) with additional fractures at any level of the vertebral column, no condition to prevent the use of PEF-meters was observed. The number of cases with thoracic vertebral fracture was 14 (7.8%). While we observed clavicle fractures in 8 (4.4%) cases, scapula fractures were found in 4 (2.2%) cases.
When those with parenchymal and pleural pathologies were evaluated, it was seen that there was pulmonary contusion in 52 (28.9%) cases, atelectasis in 36 (20%) and parenchymal laceration in 17 (9.4%) cases. Pneumothorax was present in 86 (47.8%) patients and hemothorax in 71 (39.4%). Also, 11 (45.8%) had displaced fractures and 24 cases (13.3%) were present with sternum fracture. The number of cases with rib fractures in the right and left hemithorax was close to each other, and 18 (10%) patients had bilateral rib fractures. There were other pathologies without rib fracture in 35 of the cases (19.4%). Several general patient characteristics are given in table 1.
Table 1: Patient characteristics and their traumatic injuries.
The number of patients who achieved the PEF80 value in the 70-day follow-up period was 94 (52.2%), while the number of those achieving the PEF100 value was 55 (30.6%). There was no significant relationship between gender and achieving post trauma normal respiratory functions (p = 0.780). The mean age of those who achieved PEF80 in the 70-day-follow-up period was 54.48 ± 18.49 (20-93), while those who could not accounted for 50.61 ± 17.92 (18-93). Although those achieving PEF80 looked older than those who could not, no statistical significance was demonstrated (p = 0.157).
While 63.2% of non-smokers achieved the PEF80 by the 70th day; 58.7% of ex-smokers and 42.9% of active smokers were able to achieve this value, which shows that non-smokers had a higher capacity to restore normal respiratory functions in the post trauma period (p = 0.046). When active smoking was analyzed separately, 44 (57.1%) of 77 patients in this group did not achieve the PEF80 value. Being an active smoker during the trauma period was the worst factor affecting the post-traumatic recovery of respiratory capacity (p = 0.015). No relationship was found between the amount of smoking in pack-years (p = 0.056) and the number of years before quitting (p = 0.241), and returning to normal respiratory functions in post trauma (p > 0.05). Although a statistically significant relationship could not be demonstrated between the presence of comorbidity and failure to achieve the PEF80 value, it was an interesting finding that 60.9% of those with comorbidities achieved the PEF80 value.
In terms of etiology, it was understood that 82.1% of those who could not achieve the PEF80 were present with a blunt trauma. However, the fact that the number of cases with penetrating trauma in our series was very small should be taken into consideration, which might also account for why there was no significant relationship between the etiology of trauma and the ability to return to normal respiratory function (p = 0.217). It was found that both bone fractures such as scapula (p = 0.491), clavicle (p = 0.491), thoracic vertebrae (p = 0.490), and an injury outside the rib cage did not affect achieving the PEF80 value (p > 0.05).
No statistically significant relationship was found between the pneumothorax side (right/left) (p = 0.127) and the ability to return to respiratory functions, and 55.6% of bilateral pneumothorax cases could not achieve PEF80. 62.5% of those with pneumothorax reaching PEF80 were those who had no pneumothorax at their first admission in post-trauma period. Presence of pneumothorax on the first chest tomography at admission was determined to affect patient’s returning to normal respiratory function process (p = 0.031). Although similar results were found when examined for hemothorax, statistical significance could not be demonstrated (p = 0.055).
There was no relationship between achieving the PEF80 and whether there was a unilateral or bilateral rib fracture (p = 0.795), its number (p = 0.771), the presence and number of displaced rib fractures (p = 0.838), however, it was determined that the localization of the fracture in the rib affected respiratory recovery. In a 70-day follow-up, 66.1% of patients with posterior rib fractures reached PEF80, whereas 59.1% with anterior rib fractures and 54.7% with lateral rib fractures could not. It was determined that those with a posterior rib fracture achieved the PEF80 at a higher rate (p = 0.032).
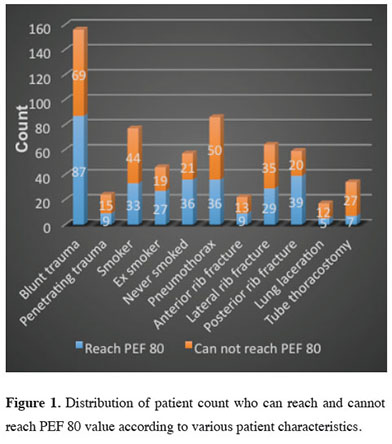
Lung laceration and pneumomediastinum were found to be effective factors in delaying the normalization of respiratory functions (p = 0.038) and (p = 0.009), respectively. Even though the number of cases with laceration was low, it was statistically significant that 12 cases did not reach PEF80, whereas 5 cases did. Considering the treatments, 61% of those who did not undergo tube thoracostomy and were followed up with medical treatment alone achieved PEF80. Also, it was remarkable to see that 79.4% of those who could not achieve the value had previously undergone tube thoracostomy. In terms of reaching PEF80, those who underwent tube thoracostomy were left behind compared to those who received medical treatment alone (p < 0.001). The relationship between PEF 80 value and several patient characteristics is given in the figure 1.
 Click Here to Zoom |
Figure 1: Distribution of patient count who can reach and cannot reach PEF 80 value according to various patient characteristics. |
Discussion
In recent years, studies investigating the quality of life in post trauma period have started to be conducted. In a study by Ulvik et al [10] which was started with 325 cases and completed with 210 cases at the end of a seven-year follow-up and in another study by Kaske et al [11] concluded with 129 cases after following 380 cases for two years, it was reported that the quality of life decreased due to post-traumatic health problems in most of the patients, and that they still complained of pain even after years. The authors emphasized that pain control is an important factor in returning to normal health functions.In a study reporting the five-year follow-up of 205 traumatized cases, it was reported that those with blunt trauma often experienced physical disability, while those suffering from penetrating trauma generally exhibited psychiatric problems [12]. Although there was no statistically significant difference between the two types of injury in terms of restoring normal respiratory functions in our study of 180 cases, the majority of whom had blunt trauma, the low number of cases with penetrating trauma in the series should be considered.
The literature generally focuses on post-traumatic long-term pain complaints, but there is no study designed in this series on the restoration of respiratory functions in the post-traumatic period. In order to question the adequacy of the follow-up period to be applied to trauma patients, we investigated the factors delaying the return to normal respiratory functions after discharge with a quantitative method.
As stated by other authors, we also believe that pain is the main factor preventing the return to adequate respiratory functions in patients with chest trauma. In our study, we tried to make this measurable by using PEF-meter and also to establish a connection with the damaged chest structures. For this purpose, we encountered no statistical relationship between reaching PEF80 in the 70-day follow-up and the number of rib fractures and in which hemithorax the fracture was (p > 0.05) while examining the number of post-traumatic rib fractures, the fracture side (right, left, bilateral), the localization of the fracture in the rib (posterior-anterior-lateral) and other bone fractures. However, it was determined that those with posterior rib fractures achieved the PEF80 more rapidly than those who had fractures with anterior and lateral localizations (p = 0.032). We attribute this to the fact that the posterior ribs are supported by more muscle mass and soft tissue, and also to the supportive effect of the scapula in stabilization.
Although it is known that smoking increases respiratory problems, the number of studies investigating its effect on respiratory functions in the post-thoracic trauma period is limited. In a prospective study by Calfee et al in 2011, the respiratory problems related to smoking in the intensive care unit for blunt trauma patients were analyzed and it was reported in this study examining lung injury that the rate of development of acute lung injury increased significantly in both active and passive smokers [13]. Similarly, in our series, active smoking during the trauma period was found to negatively affect the restoration of respiratory functions (p = 0.015), though no statistically significant relationship was found between the amount of cigarette smoked and returning to normal respiratory values in post trauma period (p = 0.056.
In a study of 1,478 cases investigating the problems caused by the presence of comorbidities, the association of advanced age (over 65 years) and comorbidity with mortality was demonstrated. The authors attributed this to the negative effects of advanced age and comorbidity on fluid-electrolyte and acid-base balances, heart rate-rhythm-contraction strength, and coagulation mechanism [14]. Although there was no statistically significant relationship between age and comorbidity and achieving the PEF80 value in 180 cases of our series, it was an interesting finding that patients with comorbidities and a higher mean age were able to achieve PEF80, which can be explained by the high compliance of the patient group to the hospital, physician and medical treatment.
In a study by Svennevig et al in which the sequela of pulmonary contusion caused by trauma was examined using pulmonary function test and arterial blood gas parameters, with a mean follow-up period of 4.9 years, it was pointed out that the patients with rib fractures tried to live with significant respiratory sequelae for years [15]. In our series in which we analyzed the earlier results, no statistically significant relationship was found between lung contusion and achieving the PEF80 (p = 0.809). In order to draw a meaningful conclusion, we are of the opinion that both the number of cases and the follow-up period should be increased. In a study of 34 pediatric cases treated for lung contusion and laceration, it was stated that no respiratory sequelae were encountered [16], while in our study including adult cases, lung laceration was found to be a determining factor in preventing the cases from reaching PEF80 in 70-day follow-up period (p = 0.038).
Tube thoracostomy is a painful procedure and most patients complain about pain at the tube thoracostomy incision site. It was determined that 79.4% of those who could not achieve the PEF80 were those who underwent tube thoracostomy due to the pathology caused by trauma (p < 0.001). It can be concluded from this data that tissue damage is more common and the restoration of-normal respiratory functions will be slower due to pneumothorax and hemothorax, and it can also be considered that tube thoracostomy itself is a painful procedure.
It should be kept in mind that pneumomediastinum may accompany pneumothorax in high-energy chest traumas [17], and eight of nine patients with pneumomediastinum in our series could not achieve the PEF80 during the follow-up period (p = 0.009). In the literature, no study has been found that reveals the time to return to normal respiratory functions in patients with pneumothorax and hemothorax. In our series, there was a significant difference between the presence of pneumothorax in the first post-trauma computed tomography imaging and failure to achieve the PEF80 (p = 0.031), but there was a moderately statistical relationship (p = 0.055) between the presence of hemothorax and failure to achieve the PEF80.
In conclusion, although thoracic surgeons have different follow-up fashions for trauma patients, patients are followed up for an average of one or two months. The vast majority of cases return to work after the first month of trauma. However, our study consisting of 180 cases based on objective measurements revealed that nearly half of the patients could not achieve 80% of the required pulmonary function value even after a 70-day follow-up period.
In our series, we tried to determine what pathologies were present in those who had difficulty in achieving the PEF80 value. Even in the light of the preliminary information we obtained with the limited number of cases, we are of the opinion that a specific evaluation should be carried out based on the trauma type while preparing the treatment and resting reports. We recommend conducting studies of this nature, bearing in mind that series with more cases and longer follow-up periods are needed to calculate the optimal and specific resting times for each trauma type.
Declaration of conflicting interests
The authors declared no conflicts of interest with respect to the authorship and/or publication of this article.
Funding
The authors received no financial support for the research and/or authorship of this article.
Ethics approval
The study was approved by the Ege University School of Medicine Ethics Committee dated 19.06.2018 and decision number 18-6.1/37.
Authors’ contribution
SA; project administration, conceptualization, developed the methodology, co-wrote the paper, AÇ; validation, manuscript reviewing and editing, SKA; conceived and designed the analysis, collected the data, co-wrote the paper, ÖK; collected the data, formulated and evaluated research goals and aims, AGE; collected and processed the data TİA; conceptualization, developed the methodology, AÖ; collected the data, KT; manuscript reviewing, UÇ; manuscript reviewing
Reference
1) Ceran S, Sunam GS, Arıbaş OK, Görmüş N, Solak H. Chest trauma in children. Eur J Cardiothorac Surg 2002; 21: 57-9.
2) Çağırıcı U, Uç H, Çalkavur T, Gürcün U, Badak İ, Bilkay Ö et al. Toraks travmaları: 6 yıllık deneyimlerimiz. Ulus Travma Acil Cerrahi Derg 1998; 4: 248-52.
3) Al-Koudmani I, Darwish B, Al-Kateb K, Taifour Y. Chest trauma experience over eleven-year period at al-Mouassat University Teaching Hospital-Damascus: a retrospective review of 888 cases. J Cardiothorac Surg 2012; 7: 35.
4) Shorr RM, Crittenden M, Indeck M, Hartunian SL, Rodriguez A. Blunt thoracic trauma. Analysis of 515 patients. Ann Surg 1987; 206: 200.
5) Marasco S, Lee G, Summerhayes R, Fitzgerald M, Bailey M. Quality of life after major trauma with multiple rib fractures. Injury 2015; 46: 61-5.
6) Mefire AC, Pagbe JJ, Fokou M, Nguimbous JF, Guifo ML, Bahebeck J. Analysis of epidemiology, lesions, treatment and outcome of 354 consecutive cases of blunt and penetrating trauma to the chest in an African setting. S Afr J Surg 2010; 48: 90-3.
7) Gabbe BJ, Sutherland AM, Hart MJ, Cameron PA. Population-based capture of long-term functional and quality of life outcomes after major trauma: the experiences of the Victorian State Trauma Registry. J Trauma Acute Care Surg 2010; 69: 532-6.
8) Quanjer PH, Lebowitz MD, Gregg I, Miller MR, Pedersen OF. Peak expiratory flow: conclusions and recommendations of a Working Party of the European Respiratory Society. Eur Respir J 1997; 24: 2-8.
9) Self TH, Cross LB, Nolan SF, Weibel JB, Hilaire M, Franks AR et al. Gender differences in the use of peak flow meters and their effect on peak expiratory flow. Pharmacotherapy 2005; 25: 526-30.
10) Ulvik A, Kvale R, Wentzel-Larsen T, Flaatten H. Quality of life 2–7 years after major trauma. Acta Anaesthesiol Scand 2008; 52: 195-201.
11) Kaske S, Lefering R, Trentzsch H, Driessen A, Bouillon B, Maegele M et al. Quality of life two years after severe trauma: a single-centre evaluation. Injury 2014; 4: 100-5.
12) Sluys K, Häggmark T, Iselius L. Outcome and quality of life 5 years after major trauma. J Trauma Acute Care Surg 2005; 59: 223-32.
13) Calfee CS, Matthay MA, Eisner MD, Benowitz N, Call M, Pittet JF et al. Active and passive cigarette smoking and acute lung injury after severe blunt trauma. Am J Respir Crit Care Med 2011; 183: 1660-5.
14) Scheetz LJ. Relationship of age, injury severity, injury type, comorbid conditions, level of care, and survival among older motor vehicle trauma patients. Res Nurs Health 2005; 28: 198-209.
15) Svennevig JL, Vaage J, Westheim A, Hafsahl G, Refsum HE. Late sequelae of lung contusion. Injury 1989; 20: 253-6.



