

Summary
Background: Although the disease progression can be silent, the pulmonary hydatid cyst (HC) may be considered a life-threatening disorder. The mainstay of pulmonary HC treatment is still surgical removal of the cyst. In the current study, we evaluated the results of surgery in patients with pulmonary HC.Materials and Methods: Thirty pulmonary HC patients who underwent surgery between 2007 and 2020 were analyzed retrospectively. The symptoms, cyst features, surgical procedures, and postoperative findings were recorded. The patients were divided into two subgroups: complicated cyst hydatid (CHC) and simple hydatid cyst (SHC).
Results: Thirteen cases were diagnosed as complicated HC with rupture into the pleural or bronchial cavity (CHC group, 43.4%), whereas 17 cases (56.6%) involved intact cysts (SHC group). Cystotomy and capitonnage were performed in the majority of the patients (n = 24, 80.0%). No mortality was observed during the one-year follow-up period.
Conclusions: Surgical management is an effective and safe method for the treatment of pulmonary HC.
Introduction
Echinococcosis is a zoonotic disease caused by Echinococcus species in the cestode class. It is an important cause of morbidity and mortality in many parts of the world [1]. Lung involvement with hematological spread is one of the most common accompanying conditions, and it may present with extrapulmonary involvement in this region due to the close proximity of the lung [1-3]. The aim of the present study was to compare our results with the relevant literature.Methods
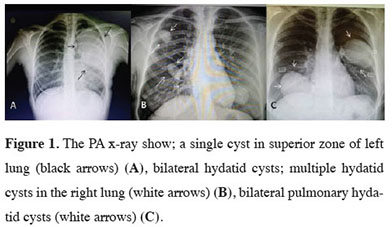
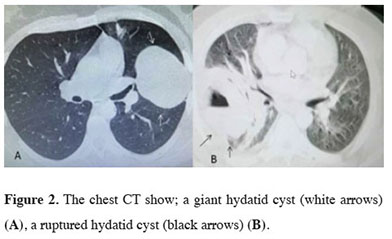
Thirty patients that were diagnosed and operated on between 2007 and 2020 due to simple hydatid cyst (SHC) or complicated hydatid cyst (CHC) were evaluated respectively. The study took place at Tokat Government Hospital. The clinical manifestation, age, sex, symptomatology, additional organ involvement, diagnostic methods, surgical interventions and preoperative and postoperative complications, duration of hospital stay, and one-year follow-up findings were recorded.After a detailed history was obtained, chest X-ray (Figures 1A-C) and thorax computed tomography (Figures 2A,B) were used to establish the diagnosis. Serologic tests were not used routinely due to their low diagnostic value.
Rupture of the hydatid cyst into the pleural cavity or bronchus was defined as CHC and an intact cyst was defined as SHC. In complicated cysts, tube thoracostomy was performed.
 Click Here to Zoom |
Figure 1: The PA x-ray show; a single cyst in superior zone of left lung (black arrows) (A), bilateral hydatid cysts; multiple hydatid cysts in the right lung (white arrows) (B), bilateral pulmonary hydatid cysts (white arrows) (C). |
 Click Here to Zoom |
Figure 2: The chest CT show; a giant hydatid cyst (white arrows) (A), a ruptured hydatid cyst (black arrows) (B). |
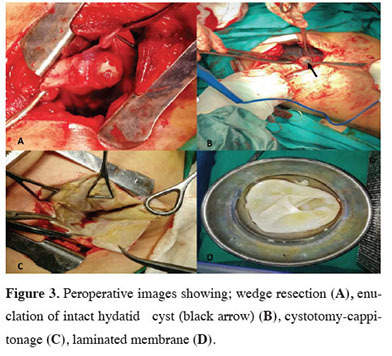
The routine surgical procedures were cystotomy and capitonnage. Posterolateral thoracotomy was performed in all patients under general anesthesia. Compresses soaked with hypertonic NaCl (10%) as a scolicidal agent were placed around the cyst field to prevent spread. The cyst content was aspirated to decrease the intracystic pressure and the laminated membrane was removed with care. The cyst cavity was irrigated with saline solution with immediate aspiration and each subsegment opening was sutured meticulously with absorbable sutures; then the cavity was obliterated from bottom to top. The pleural surface was finally sutured for prevention of any air leakage.
Wedge resection and enucleation were also performed using similar protective measures. (Figures 3A-D). Decortication and pleurectomy were the additional procedures performed for thickened pleural surfaces
 Click Here to Zoom |
Figure 3: Peroperative images showing; wedge resection (A), enuclation of intact hydatid cyst (black arrow) (B), cystotomy-cappitonage (C), laminated membrane (D). |
No mortality or serious morbidity was observed in our study. Prolonged air leakage was observed in three patients (10%), atelectasis in two patients (6.6%), and superficial wound infection in one patient (3.3%). Postoperatively all CHC patients with a rupture received albendazole treatment with a dose of 10-15 mg/kg/day in 2 or divided doses. The treatment was continued intermittently for 3 months. In the monthly follow-up, liver function tests were performed to detect possible toxicity. The study was approved by the local ethics committee of TOGU Medical School (Approval No. 22-Kaek-111).
Statistical Analysis
All statistical evaluations were made using SPSS ver 22.00 (IBM, Armonk, NY, USA). Continuous variables were presented as mean ± standard deviation (SD) and ranges. Rates were expressed as percentages.
Results
The average age was 30.8 ± 17.3. Sixteen patients (53.3%) were female and 14 (46.6%) were male. There were 17 (56.6%) SHC and 13 CHC (43.4%) patients in our case series. The main complaints were cough (40%), dyspnea (26.6%), sputum (26.6%), fever (16.6%), chest pain (16.6%), hydotoptysis (6.6%), and hemoptysis (6.6%) in the entire patient population. Fever and productive cough (in 4 (30.7%) of the patients) were the most prominent complications in complicated cases (CHC). Four patients (13.3%) had liver involvement (primary lesion) and one patient had subcutaneous HC (3.3%). The imaging methods revealed multiple HCs in six patients (20.0%), bilateral HCs (10.0%) in three patients, and a single lesion in 21 patients (70%). The HCs were localized in the left lung in 13 patients (43.4%) and right-sided HC was detected in 14 patients (46.6%). Six cases (20.0%) required chest tube thoracostomy before surgery. A preoperative biopsy was not taken from any of these patients. Three patients had been operated on previously due to HC disease (10%). Pneumonia was detected in 5 (16.6%) patients that required antibiotic therapy during the preoperative period. Moreover, in the CHC group, 3 patients had empyema (23.1%) and 3 patients hydropneumothorax (23.1%). Additionally, cyst rupture into the bronchopulmonary tree was detected in 15.4% of these cases. The main findings of the patients are summarized in table 1.Table 1: The main findings of patients.
The surgical procedures were cystotomy and capitonnage in 24 (80.0%) patients, wedge resection in 2 (6.6%) patients, and enucleation in 4 (13.3%) patients. Additional pleurectomy was applied in 4 patients (13.3%). Two of them had larger HC size (≥12 cm). Mean hospital stay was 15.46±6.1 days (201 days) for CHC, whereas it was 7.35 ± 2.4 days for SHC (125 days).
The postoperative complications observed were atelectasis, prolonged air leakage, and superficial wound infection (in 6 (20.0%) of all patients). Two (6.6%) patients underwent rigid bronchoscopy due to atelectasis after the operation.
Discussion
The diagnosis of HC is based on suspicion depending on patient history, occupation, and imaging method. Serological tests such as direct hemagglutination, latex agglutination, immunoelectrophoresis and ELISA could be used for the diagnosis [4,5]. However, the exact diagnosis is performed preoperatively and confirmed via pathological examination of material. Chest radiography, computed tomography (CT), and magnetic resonance imaging (MRI) are very effective in identifying the cyst size and localization [4,6]. Although chest X-ray is the primary diagnostic method due to its simplicity, availability, and cost, it is insufficient for evaluating the surrounding tissue and the exact localization and associated complications.The symptoms include non-specific cough, chest tightness, and pain, which can be seen in all lung diseases [1,7]. It can even be diagnosed incidentally as it may be asymptomatic until reaching large sizes. Acute symptoms may occur in complicated cysts. Spontaneous or traumatic rupture may be the cause of admission to the emergency department with chest discomfort, hemoptysis, fever, and productive cough [8-11]. The main symptom in our series was cough. Fever and productive cough were prominent in complicated patients.
The prediagnosis can be performed with imaging methods such as chest X-ray, CT, and MRI and can be strengthened with serological tests [4-6]. However, seronegative results are highly probable and therefore not essential [12,13]. In particular, direct chest X-ray gives information about the general structure of the cyst, but MRI and CT provide clearer data for the exact location, adjacent anatomical positions, and surgical planning [4-6]. Chest radiography was used as the first imaging test in our series and thorax CT was performed in all. We did not routinely use thorax MRI and serological tests in our clinic. It is important to examine the cyst material for a definitive diagnosis. However, needle aspiration biopsy is not recommended due to the risk of rupture of the infected cyst content and the formation of new cysts in the same area or anaphylactic shock. However, we performed thoracentesis for complicated cysts with acute onset symptoms that ruptured into the pleura.
The mainstay treatment for pulmonary hydatid cysts is surgery. The basic methods include excision of the cyst while preserving the tissue. The surgical technique is based on closure of air leakages from subsegmental/segmental bronchi and removal of the cyst and its contents [14]. Although lung-sparing surgery is recommended as much as possible, tissue loss may be inevitable with segmentectomy and lobectomy, depending on the extent of the cyst and the severity of complications [15,16]. This risk is slightly higher with large cysts. Cysts greater than 10 cm in diameter are defined as gigantic and have been associated with an increased risk of complications. In many aspects such as hospital duration, mean chest tube removal time, and especially postoperative prolonged air leakage large cysts are considered a different entity when compared to smaller cysts. In large cysts non-capitonnage is used as a surgical method. Variable high morbidity rates have been reported in different series; however, according to Özpolat et al, regardless of the size and surgical method surgery provides excellent outcomes [17,18]. Pulmonary hydatid disease and liver disease may occur simultaneously in 4% to 25% of cases [19]. In patients simultaneous lung and liver hydatid disease may be managed through a transdiaphragmatic approach or in some cases via a thoracoabdominal approach. This procedure is safe and spares the patient from undergoing another surgical intervention.
Currently, minimally invasive treatment in thoracic surgery is being used extensively, including in surgery for hydatid cysts. When compared to open surgery, it has obvious advantages such as less postoperative pain, fast recovery, and reduced postoperative complications [20].
When the decision concerning surgery is made carefully and meticulous planning is performed with preoperative imaging methods, unnecessary tissue loss is prevented and the incidence of postoperative adverse events is reduced [21].
The most common complication related to surgery was reported to be atelectasis and other complications indicated were wound infection, prolonged air leak, empyema, pneumothorax, and secondary hydatidosis [22]. Surgical methods were applied to all patients in our series. No mortality was observed during the one-year follow-up. Although two patients had cysts larger than 12 cm in diameter, no serious complication developed in these patients. The most common complications after surgery in our cases were atelectasis, prolonged air leak, and superficial wound infection.
In conclusion, surgery is sufficient for curative results in pulmonary hydatid cyst.
Declaration of conflicting interests
The authors declared no conflicts of interest with respect to the authorship and/or publication of this article.
Funding
The authors received no financial support for the research and/or authorship of this article.
Ethics approval
The study was approved by the local ethics committee of TOGU Medical School (Approval No. 22-Kaek-111).
Authors’ contribution
KC: Conceived and designed the analysis, collected the data, developed the methodology, wrote the paper.
Reference
1) Rawat S, Kumar R, Raja J, Singh RS, Thingnam SKS. Pulmonary hydatid cyst: Review of literature. J Family Med Prim Care 2019; 8: 2774-8.
2) Lodhia J, Chugulu S, Sadiq A, Msuya D, Mremi A. Giant isolated hydatid lung cyst: two case reports. J Med Case Rep 2020; 14: 200.
3) Dehkordi AB, Sanei B, Yousefi M, Sharafi SM, Safarnezhad F, Jafari R et al. Albendazole and Treatment of Hydatid Cyst: Review of the Literature. Infect Disord Drug Targets 2019; 19: 101-4.
4) Durhan G, Tan AA, Düzgün SA, Akkaya S, Arıyürek OM. Radiological manifestations of thoracic hydatid cysts: pulmonary and extrapulmonary findings. Insights Imaging 2020; 11: 116.
5) Moradi M, Rampisheh Z, Roozbehani M, Razmjou E. A retrospective study of hydatid cysts in patients undergoing liver and lung surgery in Tehran, Iran. Heliyon 2019; 5: e01897.
6) Lupia T, Corcione S, Guerrera F, Costardi L, Ruffini E, Pinna SM et al. Pulmonary Echinococcosis or Lung Hydatidosis: A Narrative Review. Surg Infect (Larchmt) 2021; 22: 485-95.
7) Dudha M, Shaikh Z, Bhaiyat M, Wadiwala IJ, Bhaiyat ZT. A Case of Echinococcal Cyst of the Lung. Respir Med Case Rep 2018; 25: 286-92.
8) Yaşar Z, Acat M, Turgut E, Onaran H, Dincer HE, Arda N et al. Diagnosis of Pulmonary Hydatid Cyst by Bronchoscopy. J Bronchology Interv Pulmonol 2015; 22: 343-6.
9) Engström ELS, Salih GN, Wiese L. Seronegative, complicated hydatid cyst of the lung: A case report. Respir Med Case Rep 2017; 21: 96-8.
10) Sarkar M, Pathania R, Jhobta A, Thakur BR, Chopra R. Cystic pulmonary hydatidosis. Lung India 2016; 33: 179-91.
11) Özpolat B, Sayın M, Doğan OV, Doğan Y. Simultenous traumatic rupture of bilateral pulmonary hydatic cysts. J Thorac Cardiovasc Surg 2005; 130: 908-9.
12) Kayhan S, Akgunes A. Histopatolojik Olarak Tanı Konulan Komplike Akciğer Kist Hidatik Olguları. Turkiye Parazitol Derg 2011; 35: 189-93.
13) Kara T, Arpaci RB, Vayisoğlu Y, Serinsöz E, Gürsoy D, Özgür A et al. Hydatid Cyst of Parotid Gland: An Unusual Case Diagnosed by Fine Needle Aspiration Biopsy. Turk Patoloji Derg 2017; 33: 171-4.
14) Cangir AK, Sahin E, Enön S, Kavukçu S, Akay H, Okten I et al. Surgical treatment of pulmonary hydatid cysts in children. J Pediatr Surg 2001; 36: 917-20.
15) Aletras H, Symbas PN. Hydatid disease of the lung. In: Shields TW, LoCicero J III, Ponn RB, editors. General thoracic surgery. 5th ed. Philadelphia: Lippincott Williams & Wilkins; 2000. p. 1113-22.
16) Halezeroglu S, Celik M, Uysal A, Senol C, Keles M, Arman B. Giant hydatid cysts of the lung. J Thorac Cardiovasc Surg 1997; 113: 712-7.
17) Karaoglanoglu N, Kurkcuoglu IC, Gorguner M, Eroglu A, Turkyilmaz A. Giant hydatid lung cysts. Eur J Cardiothorac Surg 2001; 19: 914-7.
18) Özpolat B, Yazkan R, Günal N, Dural K. A comparative analysis of giant and smaller hydatic of lung cysts treated surgically. Turk J Clin Lab 2017; 8: 184-90.
19) Sahin E, Enön S, Cangir AK, Kutlay H, Kavukçu S, Akay H et al. Single-stage transthoracic approach for right lung and liver hydatid disease. J Thorac Cardiovasc Surg 2003; 126: 769–73.
20) Turna A. Minimally invasive approach for pulmonary hydatid cyst. J Vis Surg 2019; 5: 16.



