

2Department of Thoracic Surgery, Beykent University Faculty of Medicine, İstanbul, Turkey
3Department of Thoracic Surgery, Marmara University Faculty of Medicine, Istanbul, Turkey
4Division of Thoracic Surgery, Yedikule Teaching Hospital for Chest Diseases and Thoracic Surgery, Istanbul, Turkey
5Division of Thoracic Surgery, Dr. Siyami Ersek Hospital for Cardiothoracic Surgery, Istanbul, Turkey DOI : 10.26663/cts.2023.006
Summary
Background: Spreading to almost all countries in the world, the COVID-19 pandemic impacted healthcare and prevented or postponed major thoracic surgeries. In this study, members of the Turkish Society of Thoracic Surgery report a consensus reached by the members for providing thoracic surgery safely during the COVID-19 pandemic.Materials and Methods: In this study, a questionnaire included categories of questions aimed to explore the aspect and perspectives of the professionals in the field. The survey was distributed through the email platform of the National Association which includes active members of the society and it was kept open between the 8th of April and the 7th of May 2021.
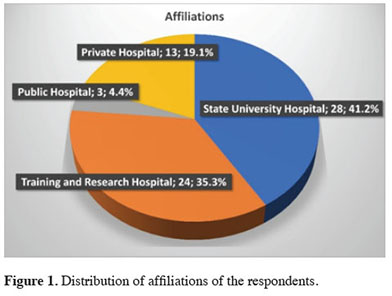
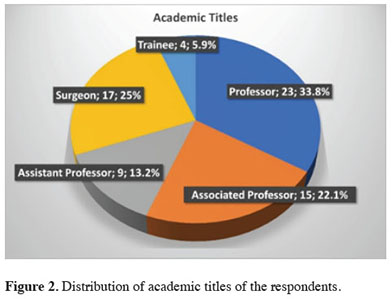
Results: Eighty members of the national association completed the survey. Most of the respondents were academic surgeons from university hospitals (43.8%) or teaching hospitals for thoracic surgery (36.3%). Almost all respondents agreed that patients with lung cancer and prolonged air leaks should be operated during the pandemic (98.8% and 96.3% respectively). The majority required that patients should be quarantined at the hospital or home up to 1 week before surgery. Academic surgeons statistically significantly more frequently thought that the quarantine period was unnecessary (p = 0.045). Most respondents indicated that stage IA to IIIA lung cancer patients should be operated. All respondents agreed that patients can be operated on provided that a PCR-negative swab test. Most of the professors thought elective surgeries should be delayed 1 to 4 weeks while some surgeons believed the delay should be more than a month (p = 0.028).
Conclusions: Thoracic surgery services for patients with thoracic should be maintained during the COVID-19 pandemic. We as thoracic surgeons are responsible to perform good surgical management of patients during this and any future pandemic.
Introduction
Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) has spread to almost all countries, with WHO declaring a COVID-19 pandemic on March 11, 2020 [1]. It has prevented major thoracic surgical surgeries in most countries redirecting almost all sources to patients with COVID-19. However, as necessary care for patients with COVID- 19 is provided, there is also a concern regarding how management for cases needing treatment for other diseases can be provided.The specialty of general thoracic surgery is expected to maintain the management of important entities such as lung cancer, esophageal cancer, inflammatory pulmonary diseases, and mediastinal and chest wall diseases. Appropriate treatment of these diseases is time-dependent. A number of guidelines have been published for the management of surgical patients during the SARS-CoV-2 pandemic [2,3]. However, they are based on expert opinions. A very large-multi-national study reported the outcomes of patients who had undergone surgery with perioperative SARS-CoV-2 infection indicated that; postoperative pulmonary complications occur in half of the patients they are associated with high mortality [4]. The necessity of timely treatment of thoracic malignancies is arguably higher than that of other malignancies where elective resections can be postponed [5,6]. It is therefore a surgical ethical challenge to maintain appropriate surgical treatment for patients with lung cancer despite limited resources during the continuing COVID-19 pandemic [7].
In this study, the Turkish Society of Thoracic Surgery reports a consensus reached by the members of society on the best possible strategy for providing thoracic surgery safely during the COVID-19 pandemic.
Methods
A questionnaire was designed on the Google Forms platform. The survey was designed by the Istanbul Branch of the Turkish Association of Thoracic Surgery. It included categories of questions that aimed to explore prerequisites of thoracic surgery during the pandemic, safety considerations when offering operations, and the setting where thoracic surgical services should be provided. Multiple-choice answers were offered for the members to select from. The survey was distributed through the email platform of the National Association which includes active members of the society. The survey was kept open between the 8th of April and the 7th of May 2021. Every survey could be answered by every member only once based on the email that is used by the member. Multiple-choice answers were offered for the experts to select from. Survey questions aimed to define the decision for operation, preoperative work-up and taken precautions, surgical planning, and postoperative course.Results from the survey formed the basis of the current Consensus Statement. The consensus was described as more than 50% agreement among the panel of experts [8]. Clinical practice was described as “recommended” if 50%-74% of the members reached an agreement.
Statistical Analysis
Data analysis was performed using IBM® SPSS Statistics 25.0(NY, USA) software. The chi-square statistics were used. Yates’ correction was made in certain comparisons. A p-value of less than 0.05 was considered statistically significant.
Results
Eighty members of the national association completed the survey. Most of the respondents were members who have been working at university hospitals (43.8%) or teaching hospitals for thoracic surgery (36.3%) (Figure 1). Professors comprised 36.3% of respondents whereas 68.8% of respondents have at least an assistant professor post (Figure 2).
 Click Here to Zoom |
Figure 1: Distribution of affiliations of the respondents. |
 Click Here to Zoom |
Figure 2: Distribution of academic titles of the respondents. |
Almost all respondents agreed that patients with lung cancer and prolonged air leaks should be operated during the pandemic (98.8% and 96.3% respectively). Ninety percent of surgeons indicated that tracheal surgery should be done during the COVID-19 era. Most members recommended surgery for mediastinal diseases (Table 1).
Table 1: Summary of responses regarding surgical indications during the COVID-19 pandemic.
The majority of respondents required that patients should be quarantined at the hospital or home up to 1 week before surgery while 25.0% of surgeons declared that it is unnecessary (Table 2). Associate professors and professors statistically significantly more frequently thought that the quarantine period was unnecessary (p = 0.045) (Table 3). There was a consensus regarding the operable stages of lung cancer: Most respondents indicated that stage IA to IIIA patients should be operated. More non-professor respondents indicated that even patients with stage IIIB and stage IV lung cancer could be operated (p = 0.066) (Table 3).
Table 2: Summary of responses regarding patient workup and safety during the COVID-19 pandemic.
Table 3: Comparison of certain responses from professors and others
All respondents agreed that patients can be operated on provided a PCR-negative swab test. There is a consensus that (i.e., 80%) patients should have negative thorax CT for COVID-19 before surgery (Table 2). There was no statistically significant difference among participants (p = 0.938) (Table 3).
Most of the members of the society agreed that FFP3 masks should be used during surgery, whereas other protective measures were deemed to be unnecessary (Table 2). Yet 23% of the surgeons believed that standard surgical gowns and surgical masks might be enough for protection (Table 3).
Minimally invasive surgical procedures were recommended to be performed by 42.5% of respondents while 53.8% of surgeons pointed out that there should be no surgical approach preference (Table 1). Professors were in favor of minimally invasive approaches and there was statistical significance compared to other surgeons (p = 0.031) (Table 3).
Eighty-one percent of respondents indicated that a patient’s companion was necessary after surgery (Table 4). Only seven participants were strictly against it during this period. More than half of the respondents (64%) thought that patients should be kept in quarantine after surgery to avoid post-operative COVID-19 infections (Table 3). One-fifth of surgeons recommended 3-day quarantine. Sixty percent of members required that patients should be discharged as early as possible during the pandemic (Table 4).
Table 4: Summary of responses regarding post-surgical care during the COVID-19 pandemic.
In addition, almost all respondents recommended that (95.7%), some period of time should be passed after COVID-19 infection in patients with COVID-19 infection (Table 2). Ten percent of respondents recommended at least 7 weeks of waiting time after negative COVID-19 PCR. Most of the professors responded as 1 to 4 weeks would be enough while more than half of the other surgeons believed the delay should be more than a month to avoid any complications due to the infection (p = 0.028) (Table 3).
Discussion
This study represents a collective definition of how to provide thoracic surgical services to patients with thoracic surgical diseases during the COVID-19 pandemic. The survey was conducted during the peak stage of the Omicron-variant surge across the world and Turkey and reflects the real-time and real-world decisions being taken in Turkish thoracic surgical units. It has been well recognized that healthcare resources including surgical wards and operation rooms due to reclaiming some operation rooms into the intensive care units stretched thin [9]. For this reason, a balance may have to be reached between the necessity to manage patients with COVID-19 and the need to treat patients with operable lung cancer.In our survey, there was a consensus that resectional surgery should proceed for treating lung cancer, mediastinal tumors, and tracheal lesions. Similarly, ASCVTS recommended by consensus that those patients should be operated during the pandemic [7,10]. Most respondents agreed that thoracic surgery should be performed after a period of quarantine. No thoracic surgery publication recommended a quarantine. However, Ralhan and colleagues stated that high-risk contacts should be tested for COVID-19 using RT-PCR after 7 days of quarantine [11]. Quarantine followed by a COVID-19 test theoretically decreased the COVID-19 infection that may develop perioperatively.
Covid-Surg collaborative study showed that COVID-19 infection developed perioperatively resulting in almost 25% of mortality [4]. For this reason, every effective measure should be taken before planned surgery. However, more members of the thoracic surgery society with high academic ranking (i.e., professors and associate professors) tended to perform surgery without any quarantine period. This statistically significant difference in strategy might be attributed to having a better and established multidisciplinary care system such as infectious diseases and multidisciplinary intensive care units by high-ranking academic personnel.
On the other hand, patients who had NSCLC and cases who might be considered marginally operable might be treated with chemoradiation followed by immunotherapy as suggested by the PACIFIC trial [12]. A fraction of patients with stage 1 NSCLC had delayed operation assuming the delay could not affect the survival of those patients [13].
Most respondents preferred to perform surgery for lung cancer patients provided certain requirements such as quarantine, negative PCR of nasal swabs, and a negative thorax CT for COVID-19. The consensus was also reached that FFP3 masks should be used during surgery, whereas other protective measures were deemed to be unnecessary. This selection of protective measures was also recommended before [10]. It should be highlighted that; the majority of respondent surgeons indicated that there was no selection of surgical approach (i.e., VATS or thoracotomy) whereas more than 40% of surgeons preferred VATS over thoracotomy during the pandemic. The experts of ASCVTS concluded that open surgery was not deemed to be safer than a minimally invasive surgery [10], however, other surgical specialties suggested a higher risk for laparoscopy due to the use of high-pressure carbon dioxide during the operation [10]. However, carbon dioxide is rarely used by thoracic surgeons. Of note, shorter hospital stays, and shorter drainage time associated with VATS procedure may be helpful in decreasing the postoperative exposure of the patients to hospital cross-infection [14].
The necessity of quarantine after thoracic surgery is yet to be described in the literature [15]. However, in our study, the majority of respondents suggested a quarantine period after surgery in order to prevent possible contamination. It has been well established that perioperative COVID-19 leads to very high mortality as high as 23.8% in 30 days. For this reason, every attempt should be made to prevent such a perioperative COVID-19. However, a national surgical guideline did not recommend any type of postoperative quarantine [16]. Nevertheless, it is preferable that the patients should be hospitalized for as short as possible. Of note, it has been well established that the implementation of enhanced recovery after thoracic surgery allows a reduction of postoperative stay and complication [17,18]. However, the effectiveness and safety of enhanced recovery after surgery protocols in the COVID-19 era are yet to be established.
In our study, a survey indicated that, for the surgical patients who had COVID-19 before planned surgery, there is a consensus that surgery should be delayed. Almost all thoracic surgeons agreed on the delay before planned surgery. In a very large study that analyzed 140,231 patients from 116 countries [19], authors concluded that surgery should be delayed for at least 7 weeks following COVID-19 in patients. It has been found that, if surgery was performed more than 7 weeks after COVID-19, mortality risk was associated with a similar mortality risk to baseline (i.e., OR: 1.5) whereas it was 4.1 in patients having surgery within 0-2 weeks of the diagnosis. However, the impact of delay on the mortality and survival of patients with cancer has been well investigated [20]. Even a four-week delay in cancer treatment was found to be associated with increased survival in surgical treatment [20]. It could be proposed that neoadjuvant therapy can be initiated in those patients with SARS-CoV-2 infection. However, many patients could not be fit for even neoadjuvant chemotherapy during this period.
There are some limitations of the study. Survey respondents were the members of the national society who accepted to answer the questionnaire. The experience and seniority of the respondents varied. We did not use a well-established model such as the Delphi process due to a large number of participants. Nevertheless, it would be reasonable to suggest that the size of respondents was large as it could have been. In the study, decisions were made as the interpretations of the responses.
The take-home message here is to evaluate the conditions and risks regarding the current pandemic. Since the survey took place in the beginning period of the global recovery from the pandemic and the first applications of vaccinations, the responses should be valid until this day when we are still discussing new waves, variants, and any possible precautions such as masks to be mandatory again. WHO did not still remove the ‘pandemic’ status of the disease. Probably, SARS-CoV-2 will continue to infect humans although the preventive measures have been effective for the last year [21]. In addition to that, there may be additional viral threats that may cripple the caregiving system and force us to make critical decisions once again [21]. This statement is therefore crucial in showing an example of a collaborative effort to fight against a pandemic and give thoracic surgical care to those who need them the most.
In conclusion, the results of the survey that were described here should provide thoracic surgeons a guideline when representing how patients can be operated for lung diseases. During the pandemic, patients who are to undergo thoracic surgery rely on thoracic surgeons to not only implement appropriate surgical treatment but to advocate for their right to receive it.
Declaration of conflicting interests
The authors declared no conflicts of interest with respect to the authorship and/or publication of this article.
Funding
The authors received no financial support for the research and/or authorship of this article.
Authors’ contributions
AT,IS: qualify for authorship according to the following criteria, analyzed and interpreted data, final approval.AT: contributed to concept and design, revised the manuscript, IS: acquired data, drafted the manuscript, AD,KB,DS,MY: administration and mentoring the study.
Availability statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.
Reference
1) WHO announces COVID-19 outbreak a pandemic. March 12, 2020. http://www.euro.who.int/en/health-topics/health-emergencies/coronavirus-covid-19/news/news/2020/3/who-announces-covid-19-outbreak-a-pandemic (accessed April 19, 2020).
2) Coccolini F, Perrone G, Chiarugi M, Di Marzo F, Ansaloni L, Scandroglio I et al. Surgery in COVID-19 patients: operational directives. World J Emerg Surg 2020; 15: 25.
3) Global guidance for surgical care during the COVID-19 pandemic. COVIDSurg Collaborative Br J Surg 2020; 107: 1097-103.
4) Mortality and pulmonary complications in patients undergoing surgery with perioperative SARS-CoV-2 infection: an international cohort study. COVIDSurg Collaborative. Lancet 2020; 396: 27-38.
5) Ficarra V, Novara G, Abrate A, Bartoletti R, Crestani A, De Nunzio C et al. Urology practice during COVID-19 pandemic. Minerva Urol Nefrol 2020; 72: 369-75.
6) Pellino G, Spinelli A. How coronavirus disease 2019 out- break is impacting colorectal cancer patients in Italy: a long shadow beyond infection. Dis Colon Rectum 2020; 63: 720-2.
7) Jheon S, Ahmed AD, Fang VW, Jung W, Khan AZ, Lee JM et al. General thoracic surgery services during the 2020 COVID-19 pandemic. Asian Cardiovasc Thorac Ann 2020; 28: 243-9.
8) Keeney S, Hasson F, McKenna H. Consulting the oracle: ten lessons from using the Delphi technique in nursing research. J Adv Nurs 2006; 53: 205-12.
9) Emanuel EJ, Persad G, Upshur R, Thome B, Parker M, Glickman A et al. Fair allocation of scarce medical resources in the time of Covid-19. N Engl J Med 2020; 382: 2049-55.
10) Jheon S, Ahmed AD, Fang VWT, Jung W, Khan AZ, Lee JM et al. Thoracic cancer surgery during the COVID-19 pandemic: a consensus statement from the Thoracic Domain of the Asian Society for Cardiovascular and Thoracic Surgery. Asian Cardiovasc Thorac Ann 2020; 28: 322-9.
11) Ralhan S, Arya RC, Gupta R, Wander GS, Gupta RK, Gupta VK et al. Cardiothoracic surgery during COVID-19: Our experience with different strategies. Ann Card Anaest 2020; 23: 485-92.
12) Antonia SJ, Villegas A, Daniel D, Vicente D, Murakami S, Hui R et al. Durvalumab after chemoradiotherapy in stage III non-small-cell lung cancer. N Engl J Med. 2017; 377: 1919- 29.
13) Yurdakul AS, Kocatürk C, Bayiz H, Gürsoy S, Bircan A, Özcan A et al. Patient and physician delay in the diagnosis and treatment of non-small cell lung cancer in Turkey. Cancer Epidem 2015; 39: 216-21.
14) Cao C, Manganas C, Ang SC, Peeceeyen S, Yan TD. Video-assisted thoracic surgery versus open thoracotomy for non-small cell lung cancer: a meta-analysis of propensity score-matched patients. Interact Cardiovasc Thorac Surg 2013; 16: 244-9.
15) Li YK, Li LQ, Wang Q, Ping W, Zhang N, Fu XN. Clinical and transmission characteristics of Covid-19- A retrospective study of 25 cases from a single thoracic surgery department. Current Med Sci 2020; 40: 1-6.
16) Covid-19 ile enfekte bir hastanın operasyona ihtiyacı olduğunda ne yapmalıyız: Cerrahi Öncesi cerrahi sırası ve cerrahi sonrası rehberi. Turk J Colerectal Dis 2020; 20: 1-8.
17) Batchelor TJP, Rasburn NJ, Abdelnour-Berchtold E, Brunelli A, Cerfolio RJ, Gonzalez M et al. Guidelines for enhanced recovery after lung surgery: recommendations of the Enhanced Recovery After Surgery (ERAS®) Society and the European Society of Thoracic Surgeons (ESTS). Eur J Cardiothorac Surg 2019; 55: 91-115.
18) Khoury AL, Kolarczyk LM, Strassle PD, Feltner C, Hance LM, Teeter EG et al. Thoracic Enhanced Recovery After Surgery: Single Academic Center Observations After Implementation. Ann Thorac Surg. 2021 Mar; 111: 1036-43.
19) Timing of surgery following SARS-CoV-2 infection: an international prospective cohort study. COVIDSurg Collaborative; GlobalSurg Collaborative. Anaesthesia 2021; 76: 748-58.



