

Summary
Background: Up to 50% of lung cancer patients develop pleural effusion during the course of the disease. Dyspnea is the primary indication for intervention. After drainage, chemical pleurodesis may be applied. Talc is the most effective sclerosing agent, and sometimes the procedure may not be successful. Adults, histologically confirmed lung cancer patients with pleural effusion who had talc pleurodesis through pleural catheter between 2014 and 2019 were included. The aim was to clarify whether lung cancer histological type and talc pleurodesis efficacy were correlated or not.Materials and Methods: A total 222 patients were enrolled retrospectively. Through the study; age, sex, cancer histological type, pleural/pleural effusion FDG uptake in PET/CT, pleural effusion’s location, amount, biochemical property, and pleurodesis efficacy were recorded.
Results: Mean age was 65.52 years, 22.9% of them were women, and 73.3% were men. Lung cancer histological types were; small cell lung cancer (13.1%), adenocarcinoma (72.1%), squamous cell carcinoma (9.5%), and not specified non-small cell lung cancer (5.4%). In 22.1% of the patients, pleurodesis was efficient, in 50% partially efficient, and in 27.9% inefficient. The only independent factor affecting pleurodesis efficacy was found as cancer histological type (p < 0.05). Pleurodesis efficacy was found higher in the squamous cell carcinoma group (p < 0.05).
Conclusions: As far as we know, this is the first study on correlation between efficacy of talc pleurodesis through the pleural catheter and the lung cancer histological types. Pleurodesis was significantly more efficient in patients with squamous cell carcinoma, possibly due to its immunohistochemical behavior.
Introduction
Malignant pleural effusion (MPE) represents 660 million incidence and almost half of the cases are caused by lung cancer, which is the most common cause. Up to 15% of lung cancer patients have MPE, and up to 50% will develop it during the course of [1]. When the effusion is massive, depending on the patients’ respiratory reserve, it might cause or aggravate dyspnea symptom which worsens the life quality and hospital admissions. Malignant pleural effusion also affects these patients’ prognosis and survival in a bad way [2]. Especially in recurrent and massive malignant pleural effusion, drainage is made for symptom palliation, and sclerosing agents may be applied into the pleural space to prevent recurrence. Chemical pleurodesis is a procedure which is applied to create symphysis between visceral and parietal pleura. Almost all agents induce a nonspecific organizing pleuritis that leads to pleural fibrosis, talc also elicits histolytic and granulomatous foreign body reaction [3,4]. Talc is the most effective and most well studied sclerosing agent [4,5]. Talc may be applied via thoracoscopy, through the chest tube, and through the pleural catheters [6-8]. However, sometimes the procedure does not succeed and patients admit to hospital with recurrent pleural effusions. To evaluate the pleurodesis efficacy complete response/efficacy, partial response/efficacy and no response/poor efficacy terms are identified. Complete response/efficacy is when no pleural effusion is observed again, partial response/ efficacy is when pleural effusion is significantly (>50%) decreased, no response/poor efficacy is when effusion is larger than defined by the partial response [9]. In a study of Rafei et al, pleurodesis efficacy was found as 17.7%, partial success as 12.9% and inefficacy as 40.3% [10]. Chen et al found that thoracoscopic talc pleurodesis was less successful in patients with lung adenocarcinoma than other histological types [9]. No other published study was found in the literature that focuses on correlation between histologic lung cancer type and pleurodesis efficacy.In general clinical practice in our center, talc pleurodesis is applied through a small diameter pleural drainage catheter (Pleuracan®) in patients diagnosed with malignant pleural effusion due to lung cancer. There is no published study about the correlation between lung cancer histopathologic type and the efficacy of talc pleurodesis through pleural catheter. Aim of this study is to clarify whether histological lung cancer type and pleurodesis efficacy/inefficacy are correlated or not.
Methods
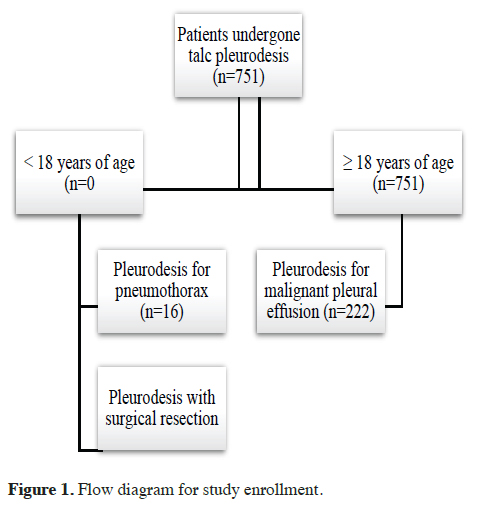
Adults, histologically confirmed lung cancer patients with pleural effusion who had talc pleurodesis through a small diameter pleural drainage catheter (Pleuracan®, B. Braun, Melsungen Germany) in our center between 2014 and 2019 were included in the study. Patients under 18 years of age, not have pathologically confirmed lung cancer, not develop pleural effusion, not have pleural catheter applied, not have talc pleurodesis applied for malignant pleural effusion, and patients who had pleurodesis because of indications other than pleural malignant pleural effusion (such as pneumothorax and surgical resection), were excluded. The flow diagram for patient selection is shown in Figure 1.
 Click Here to Zoom |
Figure 1: Flow diagram for study enrollment. |
A total of 222 patients who had inclusion criteria were researched from the hospital database and patient files retrospectively. Age, sex, histological type of lung cancer (adenocarcinoma, squamous cell carcinoma, small cell carcinoma, and not specified non-small cell lung cancer), pleural/pleural effusion FDG uptake in PET/CT (>2.5, <2.5), pleural effusion location (right, left), pleural effusion amount (moderate, massive), biochemical property of effusion (exudate, transudate), and pleurodesis efficacy (efficacy, partial success, inefficacy) were recorded.
Pleurodesis was applied when pleural fluid drainage through a small diameter pleural drainage catheter (Pleuracan®) was less than 100 ml for last the 24 hours, as talc slurry through Pleuracan®, with 4 grams of in 50 cc 0.9% NaCl solution to all study population. The catheter was clamped for 1 hour after the procedure and removed when radiological re-expansion was seen.
To define pleurodesis efficacy, like other studies in literature, these criteria were used; successful/efficient pleurodesis: No recurrent pleural effusion develops after pleurodesis, partial efficiency: 50% and less amount of previous pleural effusion recur after pleurodesis, unsuccessful/ inefficient pleurodesis: More than 50% amount of previous pleural effusion recurs after pleurodesis [9,10].
Patients were grouped in three due to their pleurodesis efficacy, and in four due to their histological lung cancer type.
The patients were checked for pleurodesis efficacy firstly on the 30th, 60th, 90th days after the procedure, and also before chemotherapy, at routine cancer control dates, and/or in case of any pulmonary symptom for their all lifelong. The study was approved by the Ethics Committee of University of Health Sciences, Ankara Atatürk Sanatorium Training and Research Hospital.
Statistical Analysis
The Statistical Package for the Social Sciences (SPSS)
for Windows, Version 22.0. Armonk, NY: IBM was used
for the statistical analysis. Quantitative variables’ mean,
standard deviation, median, lowest and highest values,
frequency and rate of the categorical variables were
calculated by descriptive statistics. The distribution of variables was controlled with the Kolmogorov-Smirnov
test. ANOVA test was used for the analysis of lung cancer
histological types’ and other categorical parameters’
effect, Independent samples T test was used for effect of
age on pleurodesis efficacy. Finally, logistic regression
analysis (LRA) was performed to find out independent
factors for pleurodesis efficacy. P < 0.05 was accepted
as statistically significance for all statistical analyzes.
Results
The mean age of 222 patients was 65.52 years (min 30, max 88). Fifty-three of them (22.9%) were women, 169 were (73.3%) men. 13.1% of the patients had small cell lung cancer (SCLC), 72.1% of them had adenocarcinoma, 9.5% had squamous cell carcinoma, and 5.4% had not specified non-small cell lung cancer (NOS). Demographic data of the study population is shown in table 1.Table 1: Demographic data of the patients enrolled.
The pleurodesis efficiency rate was found 22.1%, in 50% (n = 111) of patients it was partially efficient and in 27.9% (n=62) the pleurodesis was found inefficient. ANOVA and independent T-test were performed to determine the parameters’ effect on pleurodesis efficiency. Lung cancer histological type was found to be the only factor that affects pleurodesis efficiency (p = 0.002) (Table 2).
Table 2: Risk factors for pleurodesis efficiency.
In regression analysis, the only independent factor affecting pleurodesis efficacy was found out as the cancer histological type (p = 0.006).
Post-hoc regression test was used to find out which histological type/s was/were prognostic for pleurodesis efficiency. Pleurodesis was found to be two times more efficient in patients with squamous cell carcinoma (p = 0.038). The worst pleurodesis efficiency was found in the NOS group (p = 0.029). The statistical results are shown in table 3.
Table 3: Predictive histological factors for pleurodesis efficiency.
Discussion
Patients in this study mostly had adenocarcinoma (72.1%), 13.1% of the patients had small cell lung cancer (SCLC), 9.5% of them had squamous cell carcinoma, and 5.4% had no NOS diagnosis, histologically. This result was also compatible with the literature. Duzcu and Ozturk found that lung adenocarcinoma was the most common etiology in malignant pleural effusion, lung small cell carcinoma was the second, and lung SCC came in third place in their seven-year retrospective study on pleural fluid cytology [11]. Also in a review of MPE studies, histological type distribution in MPE complicating lung cancer was found as adenocarcinoma 78-82%, squamous cell carcinoma 14-25%, small cell carcinoma 44-53%, and miscellaneous 0-47% [12].In the study of Rafei et al, pleurodesis efficacy was found to be 17.7%, partial success was 12.9% and inefficacy was 40.3% [10]. Our sample’s pleurodesis success was higher than that. In our study, in 22.1% of patients, pleurodesis was efficient, 50% had partial success, and pleurodesis was inefficient in 27.9%. In a meta-analysis, no difference in pleurodesis success was found between large and small chest tubes [13]. While our sample included only patients with lung cancer, patients in Rafei’s study had primary tumors in several organs. Tumor origin might be the main cause of different success rates.
Chen et al found that thoracoscopic talc pleurodesis was less successful in patients with lung adenocarcinoma than other histological types [9]. We found out that patients with squamous cell carcinoma had a significantly higher efficient pleurodesis rate. In patients with nonsquamous histological types, pleurodesis was less successful and the least successful pleurodesis was in the NOS group, but we did not find a significant difference in the adenocarcinoma group. However, the techniques of pleurodesis were different in the studies.
To the best of our knowledge, this is the first study that researches the correlation between the efficacy of talc pleurodesis through the pleural catheter and the lung cancer histological types. Pleurodesis was 2 times more efficient in patients with squamous cell carcinoma, possibly due to immunohistochemical behavior.
The limitations of the study were its retrospective nature and the absence of analysis about the effect of patients’ comorbidities and medications on pleurodesis efficacy.
In conclusion, this study investigates the correlation between the efficacy of talc pleurodesis through a pleural catheter and lung cancer histological types. The only independent factor affecting pleurodesis efficacy was the lung cancer histological type, and pleurodesis was 2 times more efficient in patients with squamous cell carcinoma compared to other histological types, possibly due to immunohistochemical behavior differences. With those evidences and the literature data, we strongly believe that immunohistochemical studies defining efficient and safe biological or targeted agents are needed to improve talc pleurodesis efficacy in different types of lung cancer patients with MPE.
Declaration of conflicting interests
The authors declared no conflicts of interest with respect
to the authorship and/or publication of this article.
Funding
The authors received no financial support for the research
and/or authorship of this article.
Ethics approval
The study was approved by Ethics Committee of University
of Health Sciences, Ankara Atatürk Sanatoryum
Training and Research Hospital (Approval number
2012-KAEK-15/2687, on 26.04.2023).
Authors’ contribution
MB: Concept, design, definition of intellectual content,
literature search, clinical studies, experimental studies,
data acquisition, data analysis, statistical analysis, manuscript
preparation, manuscript editing and manuscript
review, HB: Data acquisition, data analysis, manuscript
editing and manuscript review
Reference
1) Koegelenberg CFN, Shaw JA, Irusen EM, Lee YCG. Contemporary
best practice in the management of malignant pleural
effusion. Ther Adv Respir Dis 2018; 12: 1753466618785098.
2) Porcel JM, Gasol A, Bielsa S, Civit C, Light RW, Salud A.
Clinical features and survival of lung cancer patients with pleural
effusions. Respirology 2015; 20:654-9.
3) Mierzejewski M, Korczynski P, Krenke R, Janssen JP. Chemical
pleurodesis: a review of mechanisms involved in pleural
space obliteration. Respir Res 2019; 20: 247.
4) Dipper A, Jones HE, Bhatnagar R, Preston NJ, Maskell N,
Clive AO. Interventions for the management of malignant pleural
effusions: a network meta-analysis. Cochrane Database Syst
Rev 2020; 4: CD010529.
5) Shaw P, Agarwal R. Withdrawn: pleurodesis for malignant
pleural effusions. Cochrane Database Syst Rev 2013; 11:
CD002916.6.
6) Bhatnagar R, Piotrowska HEG, Laskawiec-Szkonter M, Kahan
BC, Luengo-Fernandez R, Pepperell JCT et al. Effect of
Thoracoscopic Talc Poudrage vs Talc Slurry via Chest Tube on
Pleurodesis Failure Rate Among Patients With Malignant Pleural
Effusions: A Randomized Clinical Trial. JAMA 2020; 323: 60-9.
7) Ost DE, Niu J, Zhao H, Grosu HB, Giordano SH. Quality Gaps
and Comparative Effectiveness of Management Strategies for Recurrent
Malignant Pleural Effusions. Chest 2018; 153: 438-52.
8) Bhatnagar R, Keenan EK, Morley AJ, Kahan BC, Stanton AE,
Haris M et al. Outpatient Talc Administration by Indwelling
Pleural Catheter for Malignant Effusion. N Engl J Med 2018;
378: 1313-22.
9) Chen J, Li Z, Xu N, Zhang X, Wang Y, Lin D. Efficacy of medical
thoracoscopic talc pleurodesis in malignant pleural effusion
caused by different types of tumors and different pathological
classifications of lung cancer. Int J Clin Exp Med 2015; 8:
18945-53.
10) Rafei H, Jabak S, Mina A, Tfayli A. Pleurodesis in malignant
pleural effusions: outcome and predictors of success. Integr
Cancer Sci Therap 2015; 2: 216-21.
11) Erdogan Duzcu S, Ozturk S. Seven-year retrospective analysis
of pleural effusion cytologies and cytohistopathological correlation.
Curr Thorac Surg 2023; 8: 008-015.



