

Summary
A 48-year-old female with tuberous sclerosis admitted with shortness of breath. The chest radiography revealed a left sided hydropneumothorax. A tube thoracostomy was and 2000 cc of chylous fluid was drained. As the daily drainage was not reduced, ligation of the thoracic duct was performed. The patient was discharged uneventfully. In cases of tuberous sclerosis presenting with chylothorax, a successful treatment can be applied with early thoracic duct mass ligation.Introduction
Tuberous sclerosis is a rare autosomal dominant inherited disorder characterized by classic triad of epilepsy, mental retardation, and angiofibroma. It affects kidneys, heart, liver, bones, lungs, as well as central nervous system and skin. Lung involvement is usually similar to that seen in lymphangiomatosis, and characterized by alveolar smooth-muscle proliferation, and cystic destruction of lung parenchyma. All of these cases reported are female, and are often manifested by spontaneous pneumothorax, lymphadenopathy, angiomyolipomas and chylothorax. Chylothorax occurs when lymphatic fluid accumulates in the pleural cavity due to the impairment or obstruction of the thoracic duct and is a life-threatening condition. Chylothorax develops during tuberous sclerosis can be refractory and difficult to treat [1].Here, we present the treatment process of chylothorax in a female patient diagnosed with tuberous sclerosis along with literature data.
Case Presentation
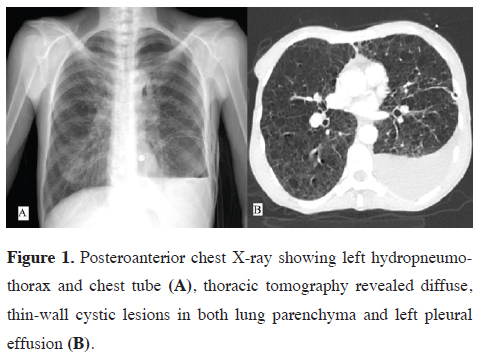
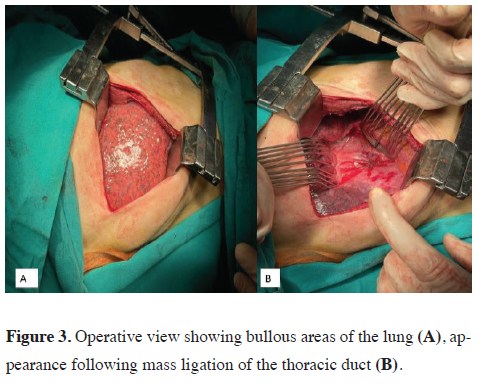
A 48-year-old woman was admitted to our clinic with shortness of breath and chest pain. The patient history included 8 years of follow-up and treatment with the diagnosis of tuberous sclerosis. Physical examination showed decreased breathing sounds in the left hemithorax. The patient underwent left tube thoracostomy due to the left hydropneumothorax on the posteroanterior chest X-ray, and 2000 cc chylous fluid was drained (Figure 1A). Thoracic tomography showed diffuse, well circumscribed, thin-wall cystic lesions in both lung parenchyma and left pleural effusion (Figure 1B). Biochemical testing of the fluid showed that triglyceride value was 435 mg/dL. Oral intake of the case discontinued and total parenteral nutrition was initiated. Daily drainage ranged from 800-1000 cc. Ultrasound and fluoroscopy- guided lymphangiography carried out on day 4 did not show lymphatic leakage in the thoracic duct (Figure 2). Since the daily drainage was not reduced, right posterior thoracotomy was performed under general anesthesia on day 7. In exploration, multiple bullous regions on the visceral pleura were seen and then ligation of the thoracic duct was performed (Figure 3A and 3B). The patient who did not develop complications was discharged on 3rd postoperative day. Postoperative follow up of 6 months was clinically and radiologically uneventful. Written informed consent was obtained from the patient for the publication of her data.
 Click Here to Zoom |
Figure 1: Posteroanterior chest X-ray showing left hydropneumothorax and chest tube (A), thoracic tomography revealed diffuse, thin-wall cystic lesions in both lung parenchyma and left pleural effusion (B). |
 Click Here to Zoom |
Figure 2: Lymphangiography showed an intact thoracic duct. |
 Click Here to Zoom |
Figure 3: Operative view showing bullous areas of the lung (A), appearance following mass ligation of the thoracic duct (B). |
Discussion
Although chylothorax is a benign condition, it can cause severe morbidity and mortality due to malnutrition, dehydration, metabolic acidosis, cachexia and immunodeficiency [2]. In recent years, somatostatin and its analog, octreotide, have been used in the treatment of chylothorax [3]. It is crucial to determine the etiology immediately and to plan conservative and/or surgical intervention. As in this case, in patients with severe comorbid diseases including tuberous sclerosis, if there is no response to conservative treatment in the early period, it should not be persisted and invasive interventions should be considered. In fact, since the patient had a diagnosis of tuberous sclerosis, fluoroscopic percutaneous thoracic duct embolization was first considered. Under normal circumstances, the success rate of this minimally invasive procedure varies between 45-100% with low morbidity, and it can be safely performed at an earlier period compared to surgery even in debilitated person [2]. Thoracic duct embolization is particularly used in traumatic chylothorax with success rates above 90% as first-line therapy. However, the success rate in non-traumatic chylothorax is lower, especially in cases with no thoracic duct occlusion or extravasation on lymphangiography [4]. In our case, embolization was not performed by invasive radiology team since lymphangiography did not show thoracic duct leak.Thoracic duct ligation remains the gold standard in the surgical treatment of chylothorax. This procedure involves application of mass ligation of the tissue between the aorta and the azygos vein above the aortic hiatus allowing optimal exposure by thoracoscopic approach or by posterior mini-thoracotomy through the 7th or 8th intercostal space on the right. Non-absorbable sutures are usually used in this technique [5]. However, we preferred absorbable polyglactin sutures because they reported to cause less tissue reaction. To reduce the risk of recurrence, the surrounding parietal pleura was bilaterally sutured into the corresponding sides to produce a regional adhesion following mass ligation.
In conclusion, chylothorax may occur during the course of tuberous sclerosis. Surgical thoracic duct ligation in the early period will prevent worsening of the general condition of the patients.
Declaration of conflicting interests
The authors declared no conflicts of interest with respect
to the authorship and/or publication of this article.
Funding
The authors received no financial support.
Author Contributions
B.O.G., S.K. and O.T. have given substantial contributions
to the literature search, data collection, study
design, analysis of data, manuscript preparation and
review of manuscript, author B.O.G., S.K., O.T. and
A.T., analysis interpretation of the data and review of
manuscript. All authors have participated to drafting
the manuscript, author B.O.G., S.K. and O.T. revised
it critically. All authors read and approved the final version
of the manuscript. All authors contributed equally
to the manuscript, read and approved the final version
of the manuscript.
Reference
1) Curatolo P, Bombardieri R, Jozwiak S. Tuberous sclerosis.
Lancet 2008; 372: 657-68.
2) Talwar A, Lee HJ. A contemporary review of chylothorax. Indian
J Chest Dis Allied Sci 2008; 50: 343-51.
3) Şahin E, Çelik B, Nadir A, Kaptanoğlu M. A case of non-Hodgkin's
lymphoma presented with tension chylothorax. Turk Gogus
Kalp Dama. 2011; 19: 660-3.



