

2Department of Thoracic Surgery, Okan University, Istanbul, Turkey DOI : 10.26663/cts.2017.0021
Summary
Pulmonary venous thrombosis is a rare condition, often seen after lung transplantation, malignancies, fungal infections and sclerosing mediastinitis. It is a life threatening complication which may develop after a thoracic surgery operation. Here we present a patient who underwent a right lower bilobectomy for bronchiectasis, and developed postoperative thrombosis of the right upper pulmonary vein which resulted in a lober gangrene. The patient was discharged uneventfully three weeks after a completion pneumonectomy. This case report aims to discuss the possible cause of this condition, which was not related to a surgical complication, and also to emphasize the importance of rapid a diagnosis and management.Introduction
Pulmonary venous thrombosis (PVT) is a rare and life threatening complication that may develop after a lobectomy or bilobectomy [1,2]. An increased radiologic opacity following an operation in addition to an increased secretion, may often be misinterpreted as an aspiration pneumonia or atelectasis. Whereas the increased opacity, and sudden deterioration in the overall medical status and laboratory values may be the signs of complications with high mortalities, such as PVT and pulmonary gangrene (PG).We report the case of a pulmonary vein thrombosis following a right lower bilobectomy for bronchiectasis as it"s a very rare complication.
Case Presentation
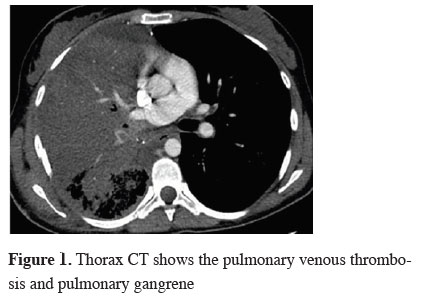
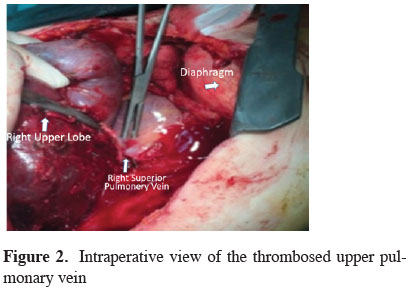
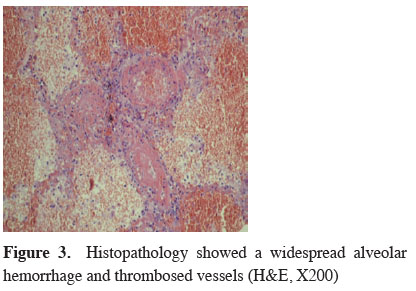
A 24-year-old female had been diagnosed with bronchiectasis of both lower lobes seven years ago, and received medical treatment for the condition. She was referred to our department due to an increase in her sputum production that affected her social life, and for a rapid progression of the bronchiectatic fields in the right lung, as noted on radiographs. A lower lobectomy was planned as the condition was more disseminated in the right lower lobe. A detailed history was taken before the operation and revealed that she was under follow up by the rheumatology department at the university hospital due to cryoglobulinemic vasculitis. A consultation was made with the rheumatologists and the patient was found to have no contraindications to surgery.Although a right lower lobectomy was planned, it"s observed that the middle lobe was also severely destroyed. Therefore, a lower bilobectomy was performed. The patient was uneventful after the operation and her chest radiograph was normal, with the exception of a lack of expansion in the right lung and minimal paracardiac infiltration. At postoperative day one, a blood gas analysis at rate of 2 L/min through a nasal oxygen cannula were; PCO2 34.5 mmHg, PO2: 134.4 mmHg, and SaO2: 98.4%. The patient was transferred to the regular ward the same day. Although she had no complaints on the first day after the operation, the second postoperative day presented progressive dyspnea, chest pain, and expansion of the infiltration on the chest radiograph. Opacification of the right upper lobe on the chest radiography was interpreted as an atelectasis and a fiberoptic bronchoscopy was performed on postoperative day 3. The bronchoscopic evaluation was normal, except for the presence of secretions. The patient"s overall condition detoriated on day 4, with an increase in the opacity on the radiography, leukocytosis (40,000/uL), and a rapid decline in the hematocrit level. Control blood gas analysis at rate of 10 L/min through a nasal oxygen cannula showed pH 7.40, PCO2 48.6 mmHg, PO2 33.2 mmHg and SaO2 63.2%. A nosocomial pneumonia and/or a possible infection were suspected, and the patient was started on intravenous fluoroquinolone and a second generation cephalosporin treatment. A contrast computer tomography scan of the chest was taken on day 4 showed a patent pulmonary artery on the right, widespread pulmonary hemorrhage and pleural effusion (Figure 1). A possible PG was diagnosed, and urgent intrapericardial completion pneumonectomy was performed. Intraoperative evaluation showed an excessive enlargement of the upper lobe due to congestion, with thrombosis in the upper vein without an obstruction (Figure 2). The upper lobectomy specimen showed widespread parenchymal hemorrhage predominantly in the apical area. Microscopic examination showed vasculitis in the small and medium sized vessels, alveolar hemorrhage, and thrombosed vascular structures (Figure 3). The patient"s condition and laboratory parameters improved significantly after completion pneumonectomy. One month after the operation, the patient was stable and under follow up for left lower lobe bronchiectasis.
 Click Here to Zoom |
Figure 1: Thorax CT shows the pulmonary venous thrombosis and pulmonary gangrene |
 Click Here to Zoom |
Figure 2: Intraperative view of the thrombosed upper pulmonary vein |
 Click Here to Zoom |
Figure 3: Histopathology showed a widespread alveolar hemorrhage and thrombosed vessels (H&E, X200) |
Discussion
PVT is a rare condition, often seen after lung transplantation, malignancies, fungal infections and sclerosing mediastinitis [3]. Thrombus in the stump of the pulmonary vein (PV) after lung resection is a rare but lethal complication. Thrombus in the systemic circulation can result in infarction of the brain, kidneys. There were only few cases describe thrombus in the stump of the pulmonary vein after the lung resection.Sudden deterioration in the general status of a patient, unilateral increase in radiologic opacity, and sudden decline in hemotocrit values, as in our patient, should suggest PVT and PG, which are emergency conditions. A transesophageal echocardiography or pulmonary angiography may be performed if the patient"s general condition is suitable [4]. On the other hand, our patient was diagnosed after a contrast CT scan was taken under emergency conditions and due to a sudden deterioration in her general condition, desaturation and unresponsiveness to oxygen, and a decline in hematocrit values. The patient was taken to the operating room within hours. There was also a rapid desaturation because she had bronchiectatic areas in the contralateral lung. Sudden deterioration in her general condition mandated rapid and radical diagnosis and treatment. A second operation had been planned previously due to the bronchiectasis in the left lower lobe; however, it was abandoned due to this unexpected condition and subsequently conservative management was chosen.
According to previous reports, torsion-angulation and thrombosis are the two underlying mechanisms for the development of thrombosis in the superior pulmonary vein. Thrombosis in the upper vein generally develops in association with middle lobe ligation [1]. In our patient, the thrombosis developed without a ligation or torsion. In addition, our patient did not have a condition such as hypercoagulability or leukemia, which would increase the tendency towards thrombosis [1]. A possible relationship with the patient"s vasculitis was considered. In a case report, Genta et al. stated that the circulation was provided by the intercostal venous collaterals in a limited number of patients who responded to medical treatment [2]. ALI, ARDS or cardiogenic pulmonary edema were excluded because the opacity was unilateral. Antibiotic treatment was initiated due to possible nosocomial pneumonia. Although thrombolytic treatment is recommended as the first line treatment in PVT which develops due to various causes, we considered that surgical treatment would be appropriate in this patient due to her high mortality risk [2].
All systemic vasculitis conditions, such as Wegener"s granulomatosis, Churg-Strauss syndrome, and cryoglobulinemic vasculitis (CV), may affect the respiratory system in a wide spectrum of conditions (asthma, pulmonary opacities, pleural effusion, alveolar hemorrhage, etc.) [5]. In their review on the respiratory involvement in systemic vasculatures, Manganelli et al. reported that CV affected small and medium sized vessels in the respiratory system. Those authors also stated that, while CV could result in asthma, pleural effusion, alveolar hemorrhage, and acute lung injury, there were no cases where it resulted in pulmonary artery or venous thrombosis [5]. In patients who develop such unexpected complications, the coexistence of thrombosis and vasculitis may be investigated.
In conclusion, previous reports show that PVT develops on the basis of ligation or torsion. However, our patient demonstrated that PVT could occur on the basis of CV. Although medical treatment may be applied initially, when a patient"s general health status deteriorates and PG develops, urgent surgery can be lifesaving.
Declaration of conflicting interests
The authors declared no conflicts of interest with respect to the authorship and/or publication of this article.
Funding
The authors received no financial support.
Reference
1) Hovaguimian H, Morris JF, Gately HL, Floten HS. Pulmonary vein thrombosis following bilobectomy. Chest 1991; 99: 1515-6.
2) Genta PR, Ho N, Beyruti R, Takagaki TY, Terra-Filho M. Pulmonary vein thrombosis after bilobectomy and development of collateral circulation. Thorax 2003; 58: 550-1.
3) Chopra T, Gibbons W, Provost K. Pulmonary Vein Thrombosis: A Rare and a Potentially Life Threatening Condition. Chest 2012; 142: 1011A.



