Summary
Extramedullary hematopoiesis is the production of blood outside of the bone marrow. While it may normally arise in the liver and spleen during the fetal period, it is considered as a compensatory mechanism in adults. Extramedullary hematopoiesis is seen in patients with chronic anemia such as thalassemia, hereditary spherocytosis, most commonly in the liver and spleen, as in the fetal period. On the other hand, intrathoracic hematopoiesis is quite rare. The aim of this study is to discuss this rare condition.A 42-year-old male patient was examined for a mass incidentally detected in the lung during his routine follow-ups. In our patient with no history of diseases except for external thalassemia intermedia, the scattered homogeneous density increments on the posteroanterior chest x-ray were evaluated and his thoracic tomography revealed soft-tissue increments of 7.5 cm in the vicinity of the rib and vertebrae. Extramedullary hematopoiesis should be kept in mind in the differential diagnosis of patients with bilateral masses by the contiguity of the rib and vertebrae. Hematological studies should be conducted in this regard.
Introduction
Extramedullary hematopoiesis (EMH) is defined as the production of blood cells outside the medulla and is normally seen in the liver and spleen during the fetal period [1,2]. On the other hand, EMH also arises in myeloproliferative diseases or hematological diseases, such as hemolytic anemia in adults.However, the mechanism at the molecular level is not fully known [3]. EMH most commonly arises in the liver and spleen, but it may also be rarely seen in the mediastinum, lymph nodes, breast, and central nervous system. In mediastinum, it is mostly located in the posterior mediastinum [3].Case Presentation
Three years ago, a 42-year old patient with no complaint was referred to Erciyes University, Department of Thoracic Surgery due to multiple homogeneous density increases on posterior-anterior chest x-ray, which had been performed for follow-up. It was learnt from the history that the patient, who was followed up by the Department of Haematology with the diagnosis of thalassemia intermedia and needed erythrocyte suspension once in every 3-4 months, underwent splenectomy in another center 20 years ago. His complete physical examination revealed no additional systemic pathology except for conjunctival pallor and his laboratory test results were as follows; Hgb: 8.7gr/dL, WBC: 10.610/mm3; Plt: 358.000/mm3. His PA chest x-ray showed multiple homogeneous density increments that did not obliterate the cardiac contours (Figure 1).
 Click Here to Zoom |
Figure 1: PA chest x-ray showing multiple homogeneous density increments and not obliterating the cardiac contours. |
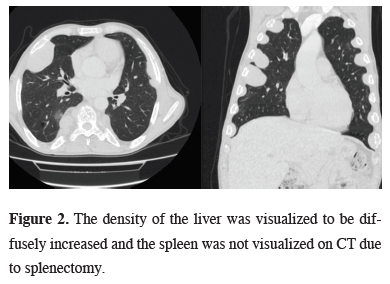
The computed tomography of the thorax showed bilateral irregular soft tissue mass around the rib and adjacent to the vertebrae. The density of the liver was visualized to be diffusely increased and the spleen was not visualized on tomography due to splenectomy (Figure 2).
 Click Here to Zoom |
Figure 2: The density of the liver was visualized to be diffusely increased and the spleen was not visualized on CT due to splenectomy. |
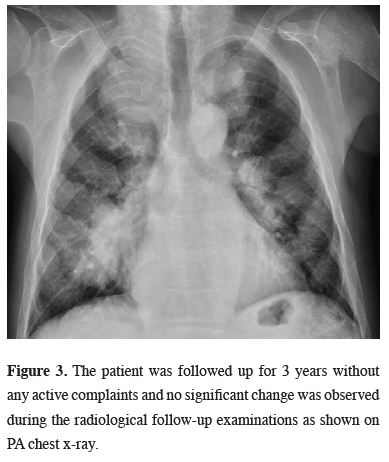
The mass lesions in the thorax were first interpreted in favor of EMH in consultation with hematology and radiology because of the diagnosis of thalassemia. Complications that may arise during the diagnostic procedure were discussed and the patient was informed and no histopathological confirmation was done. The patient was followed up for 3 years without any active complaints and no significant change was observed during the radiological follow-up examinations (Figure 3).
 Click Here to Zoom |
Figure 3: The patient was followed up for 3 years without any active complaints and no significant change was observed during the radiological follow-up examinations as shown on PA chest x-ray. |
Discussion
Extramedullary hematopoiesis is a compensatory mechanism that usually occurs in the case of chronic anemia. Therefore, it is seen in diseases with chronic anemia. It has been reported that EMH is most frequently associated with thalassemia among these diseases [2]. In this case report, the patient had thalassemia intermedia disease, which caused chronic anemia.EMH foci usually remain at a microscopic level and rarely reach a mass size. In terms of incidence, the most common locations of these foci are liver, spleen and mediastinum. These foci show up as symmetric masses when situated in the thorax [5]. Our patient had a history of splenectomy and his liver density was diffusely increased. He had masses in the posterior mediastinum and adjacent to the rib margins.
Most of the time, patients are incidentally diagnosed unless there is a symptom associated with the masses [6]. The diagnosis is usually made by the coexistence of a symmetrical, uniformly demarcated, lobulated, homogeneous mass on CT or MRI, and chronic anemia [1,5-7]. When EMH is situated in the posterior mediastinum, it may be confused with other mediastinal masses.
No diagnostic procedure is recommended since the lesion is prone to bleed [1,4-6]. However, VATS is recommended instead of needle biopsy due to effective bleeding control when the diagnosis is uncertain [6]. The diagnosis in patients with EMH located in the thorax can be made with the presence of symmetric masses along with chronic anemia or a disease leading to anemia. In our presented case, the patient was informed without performing any diagnostic procedure because of the diagnosis of underlying thalassemia intermedia and the presence of symmetrically located masses on the thoracic imaging.
The treatment was planned based on the size and location of the masses and the severity of the symptoms. On the other hand, non-symptomatic patients are followed up without treatment. Meanwhile, there is no standard treatment option. Blood transfusions, radiotherapy, use of fetal hemoglobin, hydroxyurea, and in rare cases, surgery or combination of these may be preferred for the treatment [2,4]. In this case report, the treatment of erythrocyte suspension transfusion was chosen and no growth or complication was observed in the EMH foci located in the thorax for 2 years.
In conclusion, patients with posterior mediastinal or pleural-based masses should be questioned whether there is a symmetrical distribution of the lesions before planning a diagnostic or therapeutic procedure and whether there is a hematological disease such as thalassemia with chronic anemia in the medical history by checking routine hematological parameters. By this means, an incorrect intervention can be prevented in patients with extramedullary hematopoiesis for whom interventional procedures for treatment and even diagnosis are avoided.
Declaration of conflicting interests
The authors declared no conflicts of interest with respect to the authorship and/or publication of this article.
Funding
The authors received no financial support
Reference
1) Ozdemir L, Ozdemir B, Durkaya S, Topal C, Calışkan SN, Ersoy A, Buyukbayram G, Ozbolat Z. A rare cause of posterior mediastinal masses: extramedullary hematopoiesis (two cases). Respir Case Rep 2014; 3: 156-8.
2) Zhang H, Li Y, Liu X, Chen B, Yao G, Peng Y. Extramedullary hematopoiesis: A report of two cases. Exp Ther Med 2016; 12: 3859-62.
3) Kim CH. Homeostatic and pathogenic extramedullary hematopoiesis. J Blood Med 2010; 1: 13-9.
4) Taher A, Isma’eel H, Cappellini MD. Thalassemia intermedia: Revisited. Blood Cells Mol Dis. 2006; 37: 12-20.
5) Alam R, Padmanabhan K, Rao H. Paravertebral mass in a patient with thalassemia intermedia. Chest 1997; 112: 265-7.
6) Park JB, Lee SA, Kim YH, Lee WS, Hwang JJ. Extramedullary Hematopoiesis Mimicking Mediastinal Tumor in a Patient with Hereditary Spherocytosis Case report Int J Surg Case Rep 2017; 41: 223-5.
7) Baert AL, Knauth M, Sartor K. MRI of the Lung. Berlin Heidelberg: Springer-Verlag, 2009: 217-55.






