Summary
Congenital diverticula of the left main bronchus are extremely rare in the adult. Bronchial diverticula could act as a reservoir for bronchial secretions and theoretically predispose to repeated respiratory infections. We reported a diverticulum originating from the left main bronchus with recurrent bronchopneumonia and whistling since 15 years of age. Additionally, our case had a paraaortic mediastinal bronchogenic cyst. Physical examination demonstrated whistling in the expiratory phase, which appeared when he was lying on his back or his left side. Flexible bronchoscopy showed a round-shaped lumen of the left main bronchus and bubbling from slits or indentations of the bronchial mucosa in the left main bronchus. Because our patient complained of whistling and history of recurrent bronchopneumonia infection due to bronchial diverticulum, he was operated. To the best of our knowledge, there has been no case of congenital bronchial diverticula localized in the left main bronchus associated with a paraaortic mediastinal bronchogenic cyst in the medical literature.Introduction
Diverticula of the main bronchus is a rare condition that was first described by Rocitansky in 1846 [1]. Diverticula of the main bronchus is usually asymptomatic and not a pathologic condition. However, in some cases, therapeutic interventions might be considered. Bronchogenic cysts are congenital lesions derived from abnormal budding of the embryonic foregut. The mediastinum or lung location of bronchogenic cysts are related to the time of separation from the tracheobronchial tree [2].Here we encountered the case of an enlarged subcarinal air cyst accompanied by bronchial diverticula and paraaortic mediastinal bronchogenic cyst. This is the first case wherein the diagnosis and treatment of left main bronchial diverticula with the paraaortic mediastinal bronchogenic cyst is reported.
Case Presentation
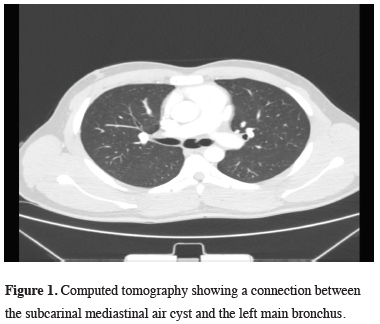
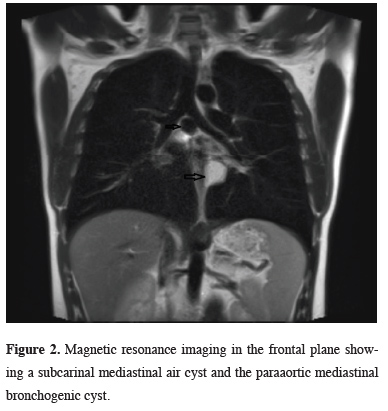
The patient was a 20-years-old male. He had recurrent bronchopneumonia and whistling for 15 years of age. Whistling had occasionally occurred when he was in the recumbent position during sleep at night. There was no clubbing in the fingers and no complaints of dyspnea at rest or with slight effort. Physical examination demonstrated wheezing in the expiratory phase, which appeared when he was lying on his back or his left side. When the patient was admitted to the hospital, there was no bronchopneumonia. The patient did not have a smoking history. Pulmonary function test showed the following results; forced expiratory volume in 1 second (FEV1), 3.32 L and FEV1/FVC, 80%. Chest CT and MRI demonstrated an air cyst (size, 25 mm) connected to the lumen of the left main bronchus and paraaortic mediastinal bronchogenic cyst (Figures 1, 2).
 Click Here to Zoom |
Figure 1: Computed tomography showing a connection between the subcarinal mediastinal air cyst and the left main bronchus. |
 Click Here to Zoom |
Figure 2: Magnetic resonance imaging in the frontal plane showing a subcarinal mediastinal air cyst and the paraaortic mediastinal bronchogenic cyst. |
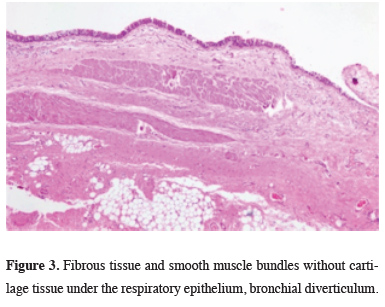
Flexible bronchoscopy showed a round-shaped lumen of the left main bronchus and bubbling from slits or indentations of the bronchial mucosa in the left main bronchus. A small orifice was located on the medial wall of the left main bronchus. The diverticulum at the left main bronchus was resected with right thoracotomy. Histologically, it was characterized by a lining wall of stratified columnar ciliated epithelium and the presence of smooth muscle and cartilage in the wall (Figure 3).
 Click Here to Zoom |
Figure 3: Fibrous tissue and smooth muscle bundles without cartilage tissue under the respiratory epithelium, bronchial diverticulum. |
After 15 days, the left paraaortic mediastinal bronchogenic cyst was completely resected with small left thoracotomy. Histologic examination showed a cyst filled with viscid and turbid fluid formed by ciliated columnar epithelial, hyaline cartilage and smooth muscle (Figure 4).
 Click Here to Zoom |
Figure 4: Cartilage tissue under the respiratory epithelium, bronchogenic cyst. |
The postoperative course was uneventful and the whistling disappeared. The patient was discharged on the 6th postoperative day. No recurrence or bronchopneumonia has been observed for the last 3 years.
Written informed consent was obtained from the patient for publication of his data.
Discussion
Diverticula of the trachea and bronchus are usually classified into two types, congenital and acquired. Congenital diverticula are thought to correspond to a rudimentary accessory bronchus that is usually located in the posteromedial border of the right main bronchus or the posterolateral border of the lower trachea. Therefore, most reported congenital diverticula have been located in these sites [3]. In our young patient, bronchial diverticulum was in the left main bronchus and associated with recurrent infections of the lower airways, which were more severe in the left lung. We considered the diverticulum to be congenital in our patient as the patient was young and symptomatic for a long time. The acquired type is thought to be associated with some inherent weakness in the tracheal or bronchial walls. Previous studies have demonstrated that acquired bronchial diverticula have a significant association with chronic obstructive pulmonary disease and smoking-related lung disease [4].Mediastinal air cysts due to bronchogenic diverticulum are extremely rare, and their differential diagnosis may include tracheocele (also known as paratracheal air cyst or tracheal diverticulum), bronchogenic cyst, and bronchopulmonary foregut duplication cyst [5].
A bronchial diverticulum is usually asymptomatic. If it becomes a large cavitary lesion filled with secretions, it can cause chronic cough, recurrent respiratory tract infections, hemoptysis, dyspnea or stridor [6]. Bronchial diverticula could act as a reservoir for bronchial secretions and theoretically predispose to repeated respiratory infections. In our case, whistling was audible and recorded only on the left side of the sternum. Flexible bronchoscopy demonstrated the airflow through a small orifice. From this observation, it was concluded that this diverticulum caused the whistling.
There is no indication for resection since most diverticula have no symptoms and complications. When infection occurs repeatedly in such a diverticula, however, resection should be done [3]. Because our patient complained of whistling and history of recurrent bronchopneumonia infection due to bronchial diverticulum, the operation was performed.
Bronchogenic mediastinal cysts are congenital lesions located usually in the middle or posterior areas of the mediastinum. The mediastinum or lung locations of bronchogenic cysts are related to the time of separation from the tracheobronchial tree. Both congenital diverticulum and bronchogenic cyst originate from the tracheobronchial tree. Therefore, we believe they are seen together. The bronchogenic cysts are usually asymptomatic and often diagnosed incidentally during routine chest roentgenogram for other reasons. The treatment options depend on the patients’ age and symptoms at presentation [2]. In young patients the surgical resection of cysts is the only treatment of choice, however, in asymptomatic adult patients remains controversial owing to the unpredictability complications or degeneration.
In conclusion, we reported a diverticulum originating from the left main bronchus with recurrent bronchopneumonia and whistling since 15 years ago. When a patient displays signs of whistling, we have to consider bronchial lesions, such as bronchial diverticulum. When infection occurs repeatedly in such diverticula, resection should be done. To the best of our knowledge, there has been no case of congenital bronchial diverticula localized in the left main bronchus associated with a paraaortic mediastinal bronchogenic cyst in the medical literature.
Declaration of conflicting interests
The authors declared no conflicts of interest with respect to the authorship and/or publication of this article.
Funding
The authors received no financial support.
Acknowledgments
We would like to thank İlknur Küçükosmanoğlu for helping in histopathological evaluation.
Reference
1) Von Rokitansky K. Handbuch der pathologischen anatomie. Vol. 3. Vienna: Braumüller & Seidel, 1984: 6-7, 11.
2) Caterino U, Amore D, Cicalese M, Curcio C. Anterior bronchogenic mediastinal cyst as priority procedure for robotic thoracic surgery. J Thorac Dis 2017;9:674-6.
3) Oizumi S, Ishida T, Kamachi M, Takahashi T, Ogura S, Manakata M, Kawakami Y. Congenital bronchial diverticulum. J Bronchology 1999;6:101-3.
4) Sverzellati N, Ingegnoli A, Calabro E, Randi G, La Vecchia C, Marchiano A, Kuhnigk JM et al. Bronchial diverticula in smokers on thin- section CT. Eur J Radiol 2010;20:88-94.






