2Department of Plastic, Reconstructive and Aesthetic Surgery, Selcuk University Medical School, Konya, Turkey DOI : 10.26663/cts.2020.00020
Summary
Many treatment options are available for lung cancer, with the highest mortality among males. Pulmonary malignancies can be addressed by a wide spectrum of treatment approaches. Treatment options can be selected according to tumor localization. Chest wall metastasis, as reported in this study, is a very rare clinical condition in which the chest wall generally requires reconstruction after resection of the tumor.Introduction
Lung cancer causes relatively high mortality among males. Several approaches to diagnosing and treating the disease have been well established. In most cases, a multi-modal approach is the gold standard treatment. However, complete resection and the presence of nodal involvement, particularly at the N2 station, have been reported as poor prognostic factors for non-small-cell lung cancer with chest wall invasion [1]. In the case of isolated chest wall invasion with tumor complication, the resection and reconstruction of the chest wall become inevitable in appropriate cases.Here we aimed to present a rare and interesting chest wall metastasis case of lung cancer.
Case Presentation
A 53-year-old male diagnosed with lung epidermoid cancer was admitted to our emergency room with bleeding from a tumor located on the right chest wall. The patient had been followed up for 3 years for lung cancer and received neoadjuvant chemotherapy. A right superior bilobectomy was performed in 2014. Thereafter, the patient continued to receive radiochemotherapy. In 2015, PET/computed tomography (CT) revealed FDG uptake on the right chest wall. Chemotherapy was continued, but the tumor progressed and invaded the chest wall skin (Figure 1), and bleeding suddenly began. The patient’s general condition and vital signs upon admission were normal.
 Click Here to Zoom |
Figure 1: Tumor located on the right chest wall and skin metastasis. |
Thoracic CT and magnetic resonance imaging (MRI) were performed to evaluate the tumor size and borders (Figures 2, 3), and the patient was advised to consult with the plastic surgery clinic. Tumor resection and chest wall reconstruction were planned.
 Click Here to Zoom |
Figure 2: (a) Primary tumor which was located in the right upper lobe before neoadjuvant chemotherapy, (b) thorax computed tomography of the tumor invading the thoracic wall. |
 Click Here to Zoom |
Figure 3: Magnetic resonance imaging of the tumor mass. |
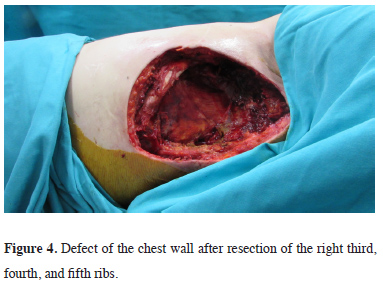
During surgery, the tumor, with the anterior portion of the right third, fourth, and fifth ribs (Figure 4), was resected.
 Click Here to Zoom |
Figure 4: Defect of the chest wall after resection of the right third, fourth, and fifth ribs. |
Tumor invasion into the lung parenchyma was not found. A latissimus dorsi musculocutaneous flap was used for reconstruction (Figures 5, 6).
 Click Here to Zoom |
Figure 5: The latissimus dorsi musculocutaneous flap. |
 Click Here to Zoom |
Figure 6: Reconstruction of the chest wall. |
In the lateral decubitus position, the latissimus dorsi muscle borders are marked and the incisions are planned according to the defect size. The adequate muscle is identified according to the deepness of the defect. Then the pedicle dissection is performed from the inferior angle of the scapula to the inferior. After that, the medial portion and the inferior portion of the flap were dissected, respectively. The flap was tunneled subcutaneously and adapted to the defect area. The patient’s pathology indicated lung epidermoid cancer metastasis. Postoperatively, the patient was followed up for 1 month.
Written informed consent was obtained from the patient for publication of his data.
Discussion
Pulmonary malignancies may be addressed by a wide spectrum of treatment approaches. Treatment options can be selected according to tumor localization. Chest wall metastasis is a very rare clinical condition requiring reconstruction after tumor resection. It remains debatable as to whether adjuvant chemotherapy or radiotherapy is mandatory for patients with completely resected chest-wall-invading, non-small-cell carcinoma without nodal involvement [2].Evaluation of the tumor infiltrating the soft tissues or bones of the chest wall and preparation for complete chest wall resection are necessary to perform radical surgery. Invasion of the thoracic wall region can be evaluated using CT, bone scan, and MRI [3].
Lung cancer invasion of the chest wall is not a common occurrence, and clinical exploration is necessary for approximately 5% of patients who have undergone resection for lung cancer [4]. When complete resection is attempted, surgeons should use anatomical knowledge to choose the optimum route of access and increase the feasibility of radical resection because of the risk of recurrence. Complete resection is defined as a pathological demonstration of negative tissue margins via frozen sections. In the present case, the resection margin was intraoperatively confirmed using frozen sections for complete resection. The patient’s positive cytology findings indicated incomplete resection. Gross residual disease after attempted resection is also classified as palliative resection. If chest wall invasion is preoperatively suspected, chest wall resection including the affected rib should be scheduled.
Resection completeness, nodal status, invasion depth, tumor size, and adjuvant chemotherapy are the prognostic factors for the long-term survival of NSCLC patients with chest wall invasion.
A statistically significant difference in terms of survival rate has been reported among patients who underwent complete resection as compared to the rate among those who received incomplete resection.
The first three ribs are well covered by pectoral muscles and do not need a replacement, primary sutures are adequate. After resection of anterior ribs or more than three ribs to need grafts or free flaps. If you planned to resect ribs, which are located in the backside of the scapula or not enlarged than three ribs, reconstruction is not performed in principle. When necessary, reconstruction of the deficit of the chest wall without synthetic materials should be attempted as soon as possible. In the present case, a latissimus dorsi musculocutaneous flap was created through plastic surgery. Complications were not encountered due to the strength and stability of the mediastinum; neither a graft nor methyl methacrylate was necessary. Successful repair was confirmed by the free flap filling the thorax. Because the lung resection was previously performed, the intercostal spaces were narrowed on the same side and the muscle flap was sufficient for reconstruction. Besides, the mediastinum was stable and fixed due to radiotherapy, so mediastinal flutter and the flail chest were not expected.
The latissimus dorsi muscle obtains its blood supply from the thoracodorsal artery via the subscapular artery system. Thus, this long pedicle elevates this largest flap for the chest wall defects. The upper edge of this flap is the inferior angle of the scapula; when one is dissecting from superior to inferior, it is important to not dissect the serratus anterior muscle fascia [5]. The serratus muscle fascia should be left intact.
The latissimus dorsi flap allows for the inclusion of the required amount of skin and muscle. The latissimus dorsi musculocutaneous flap is a versatile flap for chest wall reconstruction [6].
In conclusion, pulmonary malignancies may be addressed by a wide spectrum of treatment approaches. Treatment options can be selected according to tumor localization. Chest wall metastasis is a very rare clinical condition requiring reconstruction after tumor resection.
Declaration of conflicting interests The authors declared no conflicts of interest with respect to the authorship and/or publication of this article.
Funding
The authors received no financial support.
Acknowledgement
We would like to offer special thanks to deceased Assoc. Prof. Dr. Murat Oncel, although no longer with us, for his support and efforts.
Reference
1) McCaughan BC, Martini N, Bains MS, McCormack PM. Chest wall invasion in carcinoma of the lung. Therapeutic and prognostic implications. J Thorac Cardiovasc Surg. 1985;89:836-41.
2) Piehler JM, Pairolero PC, Weiland LH, Offord KP, Payne WS, Bernatz PE. Bronchogenic carcinoma with chest wall invasion: factors affecting survival following enbloc resection. Ann Thorac Surg. 1982;34:684-91.
3) Glazer HS, Duncan-Meyer J, Aronberg DJ, Moran JF, Levitt RG, Sagel SS. Pleural and chest wall invasion in bronchogenic carcinoma: CT evaluation. Radiology. 1985;157:191-4.
4) Grillo HC. Technical consideration in stage III disease: pleural and chest wall involvement. In: Delarue NC, Eschapasse H, eds. International Trends in General Thoracic Surgery. New York: WB Saunders; 1985:134-8.






