2Department of Pathology, Manisa Celal Bayar University, Faculty of Medicine, Manisa, Turkey DOI : 10.26663/cts.2021.0015
Summary
Pulmonary large cell neuroendocrine carcinoma (LCNEC) is known by its highly aggressive behaviour. General presentation is early spread to both regional lymph nodes and distant sites. Here we present a totally asymptomatic patient with a huge fluid-filled cystic lesion detected incidentally in a chest radiograph.Introduction
Pulmonary large cell neuroendocrine carcinoma (LCNEC) is a rare entity and accounts for 3% of all lung cancers [1]. In the latest 4th lung tumor classification of the World Health Organization (WHO, 2015), large cell neuroendocrine carcinomas were grouped with small cell carcinomas, and typical-atypical carcinoid tumors under a single heading and classified as the “neuroendocrine carcinoma group” of the lung [2]. Due to its aggressive behaviour, it is categorized as a high grade tumor. Most of the LCNECs present as an expanding mass located peripherally [1]. In this study, we are going to present a totally asymptomatic patient with a large fluid-filled pulmonary cystic lesion with a diagnosis of pulmonary LCNEC after resection.Case Presentation
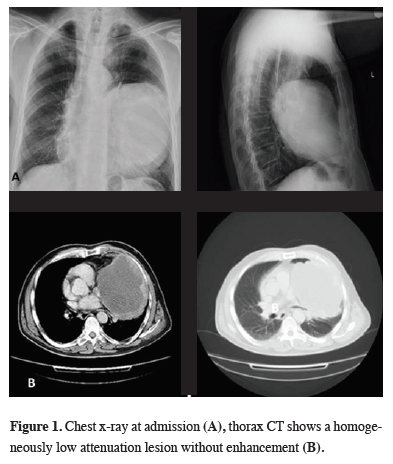
A 67-year-old male patient applied to the hospital with a huge lesion detected incidentally on a chest x-ray (Figure 1a). By profession, he was a butcher at a slaughterhouse. He was totally asymptomatic and routine blood examination was normal. The chest CT scan showed a homogeneously low-attenuation mass replacing the left lower lobe totally without any mediastinal or pleural involvement (Figure 1b).
 Click Here to Zoom |
Figure 1: Chest x-ray at admission (A), thorax CT shows a homogeneously low attenuation lesion without enhancement (B). |
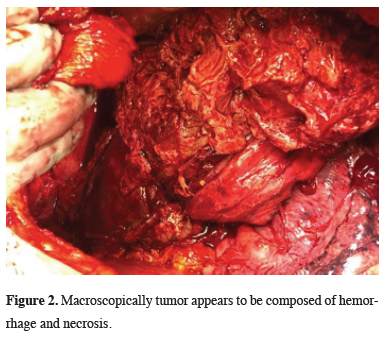
Since the CT showed no hilar or mediastinal lymph node swelling and invasion, malignancy was not considered. Pulmonary echinococcosis was suspected, but no diagnostic intervention was conducted in order to avoid breaking the cyst. Immunodiagnostic tests were also positive and supported the clinical diagnosis of cystic echinococcosis, but a definitive diagnosis could not be made before surgery. Therefore, a muscle-sparing right thoracotomy was performed. At surgery, completely hemorrhagic and necrotic fragile tumoral tissue filling the entire lower lobe was observed (Figure 2). Intraoperative frozen section analysis was consistent with malignancy. Due to extensive hemorrhage from the tumor, lower lobectomy and mediastinal lymph node dissection were performed rapidly and bleeding was controlled. The post-operative course was uneventful.
 Click Here to Zoom |
Figure 2: Macroscopically tumor appears to be composed of hemorrhage and necrosis. |
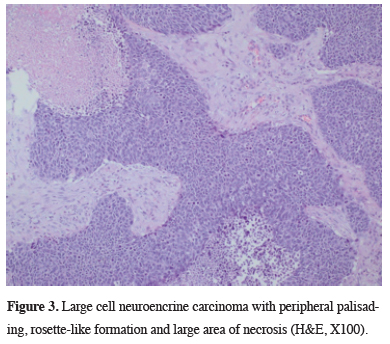
Features of a neuroendocrine morphology such as peripheral palisading and rosette-like structures were present. The tumor cells were large (greater than the diameter of three lymphocytes) with moderate to abundant cytoplasm. The cells had nuclei with vesicular chromatin and the prominent nucleoli were remarkable. All of these features were useful in discriminating large cell neuroendocrine carcinoma from small cell carcinoma. More than 10% of the tumor cells were stained with CD56 and were negative with TTF-1 and p40. As a result of these staining patterns, adenocarcinoma and squamous cell carcinoma were not considered. The tumor was diagnosed as large cell neuroendocrine carcinoma with metastatic mediastinal lymph node. (Figure 3). After the completion of surgical treatment, PET/CT was performed and results were found to be consistent with metastasis in both the liver and adrenal gland. The patient was referred to the oncology department.
 Click Here to Zoom |
Figure 3: Large cell neuroencrine carcinoma with peripheral palisading, rosette-like formation and large area of necrosis (H&E, X100). |
Written informed consent was obtained from the patient for publication of his data.
Discussion
LCNEC generally presents with a peripheral pulmonary mass and patients with LCNEC are less likely to present with symptoms [1]. This is because the majority of reported LCNEC cases were under 5 cm in diameter. İncekara et al reported 25 LCNEC cases in 10 years and the average size of the tumors was about 3 cm. The tumor was large in only one patient (10x13x17 cm) [3]. The majority of LCNEC cases were also under 5 cm. in a series published by Gürsoy et al [4]. In another report by Lee et al, the mean tumor diameter was 3.8 ± 2.1 cm [5]. In our patient, the tumor replaced the entire lower lobe and the patient was fully asymptomatic. It occurred to us that pulmonary LCNEC can reach a very large size and remain in pleural reflection without local invasion. Since the aggressive clinical behaviour and poor prognosis of LCNEC are well documented, it was challenging.It is reported that many types of lung cancer undergo necrosis and areas of haemorrhage [6]. In particular, squamous cell and large cell types are most frequently necrotic [7]. Rapid growth exceeding blood supply results with tumor necrosis and completely necrotic tumors may be indistinguishable from cysts [7]. Yoshida et al reported a 10 cm LCNEC that ruptured into the pleural cavity with the extensive necrotic and hemorrhagic content causing hemorrhagic shock [6]. In our case, the fragile huge mass gave evidence of significant hemorrhage and necrosis at thoracotomy. Histopathological evaluation revealed the tumor mostly consisted of hemorrhage and extensive necrosis. Oshiro et al analyzed the CT findings and pathological specimens of the 38 pulmonary LCNEC cases and reported that in large-diameter large cell neuroendocrine carcinoma, the tumors contained extensive necrosis and the necrotic areas seemed to be confluent and more extensive [8]. Necrotic lung cancers sometimes also mimic an abscess or other cystic lesions when cavitated [7].
This case demonstrates a rare presentation and a diagnostic challenge. Firstly, the disease was advanced and the patient did not manifest any symptoms. Secondly, despite being so large, it didn’t invade the pericardium, chest wall or diaphragm. Thirdly, the patient was a butcher by profession. ELISA was positive and presented with a large fluid-filled cystic mass in an endemic country. So malignancy was not suspected. Although a transthoracic biopsy would have broken the lesion, the possibility of a cystic echinococcosis could not be excluded pre-operatively.
In conclusion, although large cell neuroendocrine carcinoma is known as an aggressive neoplasm, it can reach giant sizes and can feature massive necrosis without any symptoms. This case presents an atypical presentation of an asymptomatic patient with pulmonary large cell neuroendocrine carcinoma.
Declaration of conflicting interests
The authors declared no conflicts of interest with respect to the authorship and/or publication of this article.
Funding
The authors received no financial support.
Authors’ contributions
DY, MSY, AT; Collected the data, performed the analysis, co-wrote the paper.
Reference
1) Takei H, Asamura H, Maeshima A, Suzuki K, Kondo H, Niki T, Yamada T et al. Large cell neuroendocrine carcinoma of the lung: a clinicopathologic study of eighty-seven cases. J Thorac Cardiovasc Surg 2002; 124: 285-92.
2) Travis WD, Brambilla E, Nicholson AG, Yatabe Y, Austin JHM, Beasley MB, Chirieac LR et al. The 2015 world health organization classification of lung tumors: impact of genetic, clinical and radiologic advances since the 2004 classification. J Thorac Oncol 2015; 10: 1243-60.
3) İncekara F, Aydoğdu K, Sayılır E, Gülhan SŞE, Demirağ F, Kaya S, Fındık G. Surgical management of large-cell neuroendocrine lung carcinoma: an analysis of 25 cases. Turk J Med Sci 2016; 46: 1808-15.
4) Gürsoy S, Usluer O, Üçvet A, Yazgan S, Yoldaş B, Yağcı T. Factors effecting long-term survival in operated large cell carcinoma of the lung. UHOD 2015; 25: 254-62.
5) Lee KW, Lee Y, Oh SW, Jin KN, Goo JM. Large cell neuroendocrine carcinoma of the lung: CT and FDG PET findings. European Journal of Radiology 2015; 84: 2332-8.
6) Yoshida K, Takasuna K, Hamanaka K, Saito G, Haniuda M, Amano J. Rupture of a large cell neuroendocrine carcinoma, causing early local recurrence. Ann Thorac Cardiovasc Surg 2006; 12: 56-9.






