Summary
Background: Bronchoscopy is a safe and reliable intervention for the management of airway diseases. Airway patency is particularly important for patients with endobronchial tumors. The aim of this study was to report the effects of rigid bronchoscopy on the prognosis of endobronchial lung tumors causing bronchial obstruction.Materials and Methods: The study included 38 patients who were referred to our clinic during 2009– 2019 following radiological or bronchoscopic diagnosis of endobronchial lesions and who were at the stage of diagnosis and treatment for lung malignancy. Their demographic characteristics, clinical complaints, pathologic diagnoses, stages of primary lung cancer, preoperative and postoperative radiological findings, and bronchoscopy results were retrospectively evaluated and recorded.
Results: A total of 29 males and 9 females were included in the study. The most common complaints observed were cough in 16 patients (42.1%) and shortness of breath in 12 (31.5%). Overall, 28 patients (73.6%) had primary pulmonary malignancy, 6 (15.7%) had benign diseases, 2 (5.2%) had primary tracheal malignancy, and 2 (5.2%) had metastasis of non-pulmonary malignancy. Full endobronchial patency was achieved in 23 patients (60.5%), whereas partial patency was achieved in 10 (26.3%). Radiological regression of opacities was observed with symptomatic relief of clinical complaints in all patients who achieved partial or full patency.
Conclusion: Bronchoscopic destruction of an endobronchial lesion causing tracheobronchial obstruction is critical for improving acute respiratory distress, avoiding the development of lung damage, and preventing delayed treatment in malignant cases.
Introduction
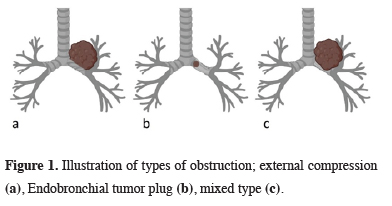
Bronchoscopy is a safe surgical method for the diagnosis, treatment, and management of airway diseases and has been practiced for more than a century [1]. It can be performed as a rigid or flexible procedure, but the advantageous aspects of flexible bronchoscopy is the reason why it is more commonly used in some areas. Nevertheless, rigid bronchoscopy is still the most reliable intervention for foreign body aspirations, central airway obstructions, and tracheobronchial stenting [2,3].Problems related to airway obstruction are encountered in approximately 30% of lung cancer patients [4]. In such patients, this obstruction occurs in three ways: as an endobronchial tumor plug, as external compression, or as a mixed type (Figure 1). The majority of lung cancer patients are at an advanced disease stage at the time of diagnosis [5]. However, the current use of targeted therapies, chemotherapy and radiotherapy protocols, and implementation of immunotherapy, has significantly improved the survival rate, even in patients whose tumors have not completely disappeared. Restoration of airway patency, which we consider as a part of these multimodal approaches, has therefore become obligatory in patients with endobronchial tumors.
 Click Here to Zoom |
Figure 1: Illustration of types of obstruction; external compression (a), Endobronchial tumor plug (b), mixed type (c). |
In some cases, bronchial obstruction caused by systemic tumor metastasis is also encountered. These obstructions may occur as a result of external compression of the tumors on adjacent organs, or the tumors may have a direct endobronchial location. In addition, obstruction can occur due to benign lung pathologies, which constitute 2%–5% of all lung tumors and include adenomas, hamartomas, lipomas, and hemangiomas [6]. These benign tumors may be preliminarily diagnosed as a malignancy due to their presentation with similar clinical and radiological findings but may later be diagnosed correctly through bronchoscopy. The present study aimed to report the effects of rigid bronchoscopy on the prognosis of endobronchial lung tumors causing bronchial obstruction.
Methods
This study included 38 patients who were referred to our clinic during 2009-2019 following the diagnosis of endobronchial lesions radiologically or by bronchoscopy and who were at the diagnosis and treatment stage for lung malignancy. Patients who had post-intubation and post-tracheostomy stenoses, traumatic stenoses, and obstructions caused by external compression of the bronchus were excluded from the study.
Bronchoscopic tumor destruction
All bronchoscopic procedures were performed using a rigid bronchoscope (Karl Storz™, Germany), and all patients underwent rigid bronchoscopy under general anesthesia. If the structure of the tumor allowed its resection from the mucosa, mechanical destruction was performed with forceps. After determining localization and type of the tumor, forceps was used for direct tumor destruction. If the bronchial mucosa had cleavage next to the tumor, we aimed for luminal opening through it. If the tumor had a peduncle on the mucosa, it was excised completely due to tumor mobility. The bleeding control was done with endobronchial cold saline lavage and aspiration.
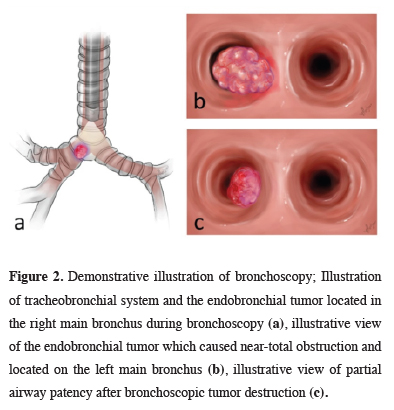
Cases where 100% of the airway became patent during bronchoscopy were considered to have achieved “full patency.” Cases provided with ventilation but with airway patency under 100% were considered to have achieved “partial patency” (Figure 2).
 Click Here to Zoom |
Figure 2: Demonstrative illustration of bronchoscopy; Illustration of tracheobronchial system and the endobronchial tumor located in the right main bronchus during bronchoscopy (a), illustrative view of the endobronchial tumor which caused near-total obstruction and located on the left main bronchus (b), illustrative view of partial airway patency after bronchoscopic tumor destruction (c). |
Airway patency was checked through chest X-rays and computed tomography (CT) scans performed postoperatively.
The demographic characteristics, clinical complaints, previous diagnoses (if any), stages of cancer in primary lung cancer patients, preoperative and postoperative radiological findings, bronchoscopy results, and postoperative pathology diagnoses were retrospectively evaluated and recorded after approval by the Institutional Ethics Committee (Approval number: 2020/262).
Results
The 38 patients (29 males and 9 females) had a mean age of 58.89 ±9.93 years (range 31-78 years). The most common complaints were cough in 16 patients (42.1%) and shortness of breath in 12 patients (31.6%) (Table 1).Table 1: Complaints of patients
Overall, 16 patients (42.1%) were undiagnosed prior to rigid bronchoscopy. Of the 38 patients, 28 had primary lung malignancy (Table 2).
Table 2: Histopathological results of the lesions.
The staging of the primary lung cancer patients at the time of bronchoscopy was performed in accordance with the 8th edition of the Tumor, Node, and Metastasis staging system for lung cancer. Accordingly, 11 patients (39.3%) were classified as stage III, 8 (28.6%) as stage IV, 7 (25%) as stage I, and 2 (7.1%) as stage II (Table 3).
Table 3: Stages of the patients who were diagnosed with primary lung cancer.
Thoracic CT scans performed preoperatively revealed an endobronchial lesion that did not negatively affect ventilation in the distal parenchyma but caused bronchial obstruction in 23 patients (60.5%). Six patients (15.8%) presented at our clinic with complete atelectasis of the right lung, three patients (7.9%) with complete atelectasis of the left lung, three patients (7.9%) with lobar and segmental atelectasis, two patients (5.3%) with increased aeration in the left lung, and one patient (2.6%) with increased aeration in the right lung.
Bronchoscopy revealed endobronchial-type bronchial obstruction in 27 patients (71%) and mixed-type bronchial obstruction in 11 patients (29%). The tumor localization in the CT was on the right in 25 patients (65.8%) and on the left in 13 patients (34.2%). Obstruction of the main bronchus was observed in 30 patients (78.9%); 19 of whom had obstruction on the right and 11 on the left main bronchus. Eight patients (21.1%) had lobar and segmental bronchial obstruction.
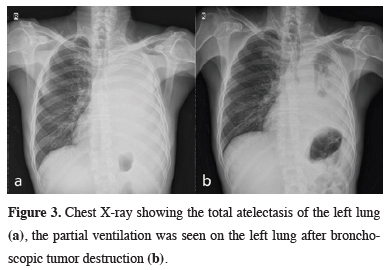
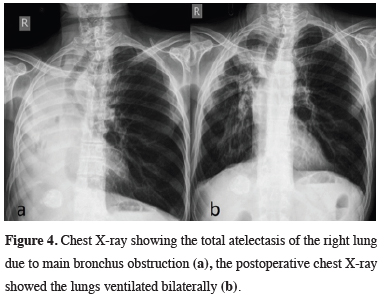
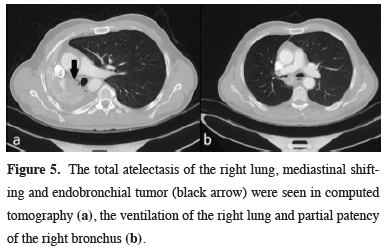
After bronchoscopy, full endobronchial patency was achieved in 23 patients (60.5%), whereas partial patency was achieved in 10 patients (26.3%) (Figures 3 and 4). In five patients, the distal endobronchial part of the tumor could not be observed safely (13.2%). All endobronchial hemorrhages were controlled locally after tumor resection, and no patient required thoracotomy. There were no intraoperative and postoperative complications. Radiological regression of opacities were observed with symptomatic relief of clinical complaints were established in all patients who achieved partial or full patency (Figure 5).
 Click Here to Zoom |
Figure 3: Chest X-ray showing the total atelectasis of the left lung (a), the partial ventilation was seen on the left lung after bronchoscopic tumor destruction (b). |
 Click Here to Zoom |
Figure 4: Chest X-ray showing the total atelectasis of the right lung due to main bronchus obstruction (a), the postoperative chest X-ray showed the lungs ventilated bilaterally (b). |
 Click Here to Zoom |
Figure 5: The total atelectasis of the right lung, mediastinal shifting and endobronchial tumor (black arrow) were seen in computed tomography (a), the ventilation of the right lung and partial patency of the right bronchus (b). |
Obstruction occurred in three patients, and two patients underwent tracheobronchial stenting. In one patient, tumor destruction was completed with two rigid bronchoscopy procedures conducted at one-month intervals. In one patient with a hamartoma, an upper lobectomy was performed due to the development of bronchiectasis over time. Two patients with typical carcinoid tumors, one located in the lingula and the other in the left main bronchus, recovered following total bronchoscopic excision. Anatomical pulmonary resections were performed following bronchoscopy in three patients with malignant pathologies.
In two patients with atypical carcinoid tumor, left upper lobectomy was performed due to the continuity of the tumor in the bronchial wall in one, and bilobectomy inferior due to accompanying bronchiectasis in the other one. Additionally, one patient who had an adenoid cystic carcinoma located in the right main bronchus underwent pneumonectomy.
Death occurred within the first week in two patients diagnosed with stage IVA squamous cell carcinoma (SCC) and stage IVB adenosquamous carcinoma, respectively. Both these patients had total obstruction of the right main bronchus, and the distal endobronchial part of the tumor could not observed safely. Three patients diagnosed with SCC who achieved full endobronchial patency also died due to acute renal failure during the course of chemotherapy in the first (stage IIB), sixth (stage IVB), and seventh month (stage IIIA), respectively. Four patients who achieved full patency and completed their treatment protocols had one- to three-year survivals (stage IIIB SCC, 1.5 years; stage IIA SCC, 2 years; stage IB SCC, 2.5 years; and stage IIIA SCC, 3 years, respectively). Follow-up and treatment of the other patients continued.
Discussion
Respiratory pathologies lead to serious morbidity and mortality, and early diagnosis plays a vital role in the course and control of these diseases [7]. The basic and most commonly practiced radiological examination is the chest X-ray, but low-dose thoracic CT is also used in screening programs and is now more commonly recommended [5]. If the radiological results detect an intrapulmonary pathology, the pathology is quickly diagnosed and treatment is commenced.Patient complaints due to endobronchial pathologies are usually related to effects on the distal parenchyma and/or irritation of the airway. Symptoms include shortness of breath, cough, hemoptysis, sputum production, and wheezing. Patients presenting with these complaints should be screened for an intrapulmonary pathology upon their initial arrival at the clinic or during follow-up. The delayed diagnosis of an airway obstruction may lead to secondary effects, such as atelectasis, pneumonia, abscess, bronchiectasis, and tracheobronchial stricture in the affected lung, even if the tumor is diagnosed as benign [8].
The presence of airway obstruction in an oncological patient may disrupt the patient’s comfort and stable course and can cause delays in the administration of medical or surgical treatments required in the event of a possible secondary infection. The major airway obstruction associated with lung cancer is a life-threatening clinical condition that rapidly deteriorates. For example, Daneshvar et al have reported a prevalence of central airway obstruction of 13% and that the majority of lung cancer patients who developed airway obstruction were in the stage III and IV groups [9]. In our study, 67.9% of patients diagnosed with primary lung cancer were in stage III and IV. This prevalence can be explained by the large-sized masses that cause metastatic conglomerated lymph nodes. These nodes are centrally localized and close to the central airways, resulting in a more pronounced pressure effect and tumor invasion. Chemotherapy and radiotherapy treatments usually continue in these patients, leaving them with limited tolerance to complications secondary to bronchial obstruction due to their medical condition. Airway obstruction due to malignancy also increases mortality. Mechanical elimination of obstructions in the airway by bronchoscopy, therefore, improves the clinical course of the disease. For this reason, intervention with bronchoscopy should not be delayed in patients for whom it may be indicated.
In the present study, all patients who achieved full patency or partial patency by endobronchial intervention were able to continue their treatment protocols. However, in five patients, the distal part of the tumor could not be reached and luminal patency could not be achieved, and two of them with total obstruction of the right main bronchus died within the first week. We concluded that mechanical elimination of endobronchial obstruction through bronchoscopy reduces mortality.
The diagnosis and treatment of airway pathologies and tracheobronchial foreign body aspirations and the need for provision of airway safety in acute respiratory distress constitute the main indications for rigid bronchoscopy [1]. The wide lumen and fixed rigidity of this procedure permits surgical manipulations, such as those performed using an aspirator and various tools, while providing lung ventilation. The approach and treatment plan in malignancy-induced endobronchial obstruction should be decided by evaluating the characteristics of the lesion, the patient’s medical condition, whether the obstruction is endobronchial or caused by external compression, and the stage of the treatment process. In the case of a tumor that decreases or does not grow in size in response to chemotherapy or radiotherapy lung cancer treatments, the obstruction may not recur after mechanical destruction with bronchoscopy.
Additional options available for management of tumors causing endobronchial obstruction include cryo-canalization, brachytherapy, argon plasma coagulation, and laser and electro-cauterization, and these interventions can be successfully implemented with appropriate equipment [10,11]. The advantage of mechanical destruction with rigid bronchoscopy over these other procedures is that bronchoscopy does not require additional devices and equipment, making it less costly. Mechanical destruction can also be easily be performed by a surgeon experienced in rigid bronchoscopy manipulations to provide quick and effective intervention in emergencies. In the case of external compression, tracheobronchial stents can be safely inserted to prevent recurrence of the obstruction by providing a mechanical barrier and ensuring airway patency [12]. Stent insertion is also an alternative for patients with recurrent obstruction. In the present study, a stent was inserted in two patients, but bronchoscopy had to be performed three times in a row in one patient. The waiting time to obtain supplies and the urgency of bronchoscopy were considered when repeated bronchoscopy was performed. The patient is not subjected to serious harm in repeating this procedure, as bronchoscopy can be considered a minimally invasive procedure. Furthermore, tumor destruction by bronchoscopy in malignancy-induced endobronchial obstruction to provide airway improves the survival and treatment compliance of patients [11]. This approach is also a palliative intervention for patients with advanced stage or technically unresectable clinical conditions.
In addition to primary lung cancers, metastatic lesions of the lung can also present with endobronchial obstruction. Thyroid, colon, breast, esophagus, and kidney cancers are among the malignancies that lead to endobronchial lung metastasis [13]. In the present study, two patients had an extrapulmonary malignancy (renal cell carcinoma and plasmacytoma). The bronchoscopic approach in these patients did not differ from primary lung malignancies in the other patients.
Benign lung tumors are less common when compared with all other lung tumors. Although hamartoma and adenoma are the most frequently occurring benign lung tumors, endobronchial polyps, inflammatory polyps, and, more rarely, granulomas and lipomas are also considered benign lung tumors. Endobronchial presentation of benign lung tumors is quite rare, but rigid bronchoscopy is sufficient for the diagnosis and treatment of approximately 95% of patients with benign tumors [14]. Recurrence rarely occurs. In the present study, lesions having a benign pathology were excised using rigid bronchoscopy in six patients. In addition to being a palliative procedure, endobronchial tumor destruction by bronchoscopy is curative for low-grade tumors, such as typical carcinoids and benign lesions. Additional surgical treatment was not implemented in two patients diagnosed with typical carcinoids in this study, and their follow-up treatment continued.
In conclusion, bronchoscopic destruction of endobronchial lesions causing tracheobronchial obstruction is of critical significance in improving acute respiratory distress, preventing the development of lung damage, and preventing delayed treatment in malignant cases, regardless of the clinical course, stage, and diagnosis of the patient.
Acknowledgement
We thank Merve Evren, PhD, for the artwork in Figure 2.
Declaration of conflicting interests
The authors declared no conflicts of interest with respect to the authorship and/or publication of this article.
Funding
The authors received no financial support for the research and/or authorship of this article.
Ethics Approval
The study was approved by the institutional ethical board of Selcuk University Medical Faculty (Approval number: 2020/262).
Authors’ contributions
HY; collected the data, co-wrote the paper, performed the analysis, GSS; co-wrote the paper, conceived and designed the analysis, AC; collected the data, contributed data/analysis tools.
Reference
1) Batra H, Yarmus L. Indications and complications of rigid bronchoscopy. Expert Rev Respir Med 2018; 12: 509-20.
2) Sunam GS, Oncel M, Yildiran H. Bronchoscopy in Benign Tracheal Stenosis. Ann Thorac Surg 2016; 102: 2133.
3) Oncel M, Sunam GS, Ceran S. Tracheobronchial aspiration of foreign bodies and rigid bronchoscopy in children. Pediatr Int 2012; 54: 532-5.
4) Yarmus L, Feller-Kopman D. New Bronchoscopic Instrumentation: A review and update in Rigid Bronchoscopy. In: Beamis JF, Mathur PN, Mehta AC, editors. Interventional pulmonary medicine. Lung biology in health and disease 230. New York: Informa Healthcare; 2010. pp. 1-9.
5) Huang KL, Wang SY, Lu WC, Chang YH, Su J, Lu YT. Effects of low-dose computed tomography on lung cancer screening: a systematic review, meta-analysis, and trial sequential analysis. BMC Pulm Med 2019; 19: 126.
6) Madana K, Agarwala R, Bala A, Gupta D. Bronchoscopic management of a rare benign endobronchial tumor. Rev Port Pneumol 2012; 18: 251-4.
7) Jois DS, Mutreja D, Handa A, Moorchung N. Correlation between transbronchial lung biopsy and lung cytology. Rev Esp Patol 2020; 53: 75-8.
8) Lamprecht B, Hutarew G, Porsch P, Wegleitner B, Studnicka M. Successful bronchoscopic cryorecanalization in a case of endobronchial lipoma. Diagn Ther Endosc 2011; 2011: 845686.
9) Daneshvar C, Falconer WE, Ahmed M, Sibly A, Hindle M, Nicholson TW, et al. Prevalence and outcome of central airway obstruction in patients with lung cancer. BMJ Open Respir Res 2019;6:e000429. doi: 10.1136/bmjresp-2019-000429.
10) Schumann C, Hetzel M, Babiak AJ, Hetzel J, Merk T, Wibmer T, et al. Endobronchial tumor debulking with a flexible cryoprobe for immediate treatment of malignant stenosis. J Thorac Cardiovasc Surg 2010; 139: 997-1000.
11) Stanopoulos IT, Beamis JF Jr, Martinez FJ, Vergos K, Shapshay SM. Laser bronchoscopy in respiratory failure from malignant airway obstruction. Crit Care Med 1993; 21: 386-91.
12) Huang IA, Hsia SH, Wu CT, Jaing TH, Lai SH, Liu YH. Combined chemotherapy and tracheobronchial stenting for life-threatening airway obstruction in a child with endobronchial non-Hodgkin lymphoma. Pediatr Hematol Oncol 2004; 21: 725-9.






