2Department of Thoracic Surgery, University of Health Sciences, Dr. Suat Seren Chest Diseases and Surgery Medical Practice and Research Center, İzmir, Turkey DOI : 10.26663/cts.2021.0023
Summary
Hydatid cyst is a zoonotic disease that is common worldwide. Turkey is an endemic region for hydatid cyst due to the widespread farming and animal husbandry. Echinococcus granulosus is the most common infestation species in humans, and humans are the incidental intermediate host. The cyst formed by this zoonotic cause is expected to be localized in either lungs or the liver, depending on the part of the life cycle in humans. Soft tissue or intramuscular presence of the cyst is rare. Herein, we present a hydatid cyst case with an unusual localization.Introduction
Hydatid cyst is a commonly seen zoonotic disease. Turkey is an endemic region for hydatid cyst due to the widespread farming and animal husbandry [1]. Echinococcus granulosus is the most common infestation species in humans, and humans are the incidental intermediate host [2]. The cyst formed by this zoonotic cause is expected to be localized in either lungs or the liver, depending on its life cycle. Soft tissue or intramuscular presence of the cyst is rare, and differential diagnoses include soft tissue tumors. Herein, we present a hydatid cyst case located out of the thoracic cavity.Case Presentation
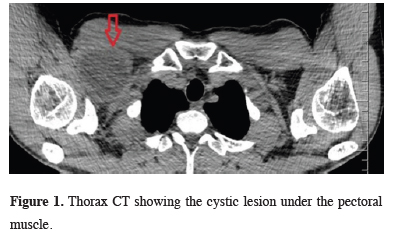
A 39-year-old male patient presented to our clinic with swelling, redness, and pain under his clavicular region. He had a history of a mass excision from the same area two years ago. He did not have a discharge report from the previous intervention but according to the patients statement ‘a cyst was removed’. When the patient was questioned about his postoperative medical treatment after the surgery he stated that he was given a prescription but he did not use any medication other than pain killers. He mentioned that during the last three months the swelling increased progressively. The previous incision scar was visible under the clavicle bone and the mass was round and palpable with well circumcision right under the clavicle bone during the physical examination.The ultrasound examination revealed a 55x42 mm lesion containing multiloculated cysts at the right infraclavicular region. Thorax computed tomography showed the cystic lesion located under the pectoral muscle, adjacent to the clavicle’s lower border and not related to the thoracic cavity (Figure 1). The reported multiloculation dominantly suggested the recurrence of hydatic cyst disease.
 Click Here to Zoom |
Figure 1: Thorax CT showing the cystic lesion under the pectoral muscle. |
Surgical excision was planned. It was observed that the cystic structure was in the pectoral muscle during the anatomical dissection. The pericystic structure was taut and thin, and punctured during the procedure and all round cysts filled with clear fluid meticulously enucleated (Figure 2). The macroscopic appearance was compatible with hydatid cyst.
 Click Here to Zoom |
Figure 2: Extracted cysts. |
The cavity was lavaged with a 20% hypertonic solution to achieve a scolicidal affect. No complications occurred postoperatively. The patient was discharged on the 1st postoperative day uneventfully. Histopathologic examination reported the presence of germinative membrane, eosinophilic stained nuclei, acellular lamellar cuticle layer and outermost fibrous tissue, in addition to inflammatory granulation tissue, and scolex in the cyst lumen, which was compatible with the diagnosis of hydatid cyst.
Albendazole treatment with a dose of 15 mg/kg/day, was initiated in the postoperative first outpatient clinic follow-up, which was advised for 6 months. No additional lesion was detected in the postoperative 3rd-month follow-up control.
Written informed consent was obtained from the patient for publication of his data.
Discussion
Humans are intermediate hosts for hydatid cyst. Orally taken parasite embryos due to contaminated food or water pass into the blood from the duodenal mucosa and can spread to all body tissues. The most common site of localization is liver (50-70%) and lung (11-17%). Whereas pericardium (5%), soft tissues (2.4-5.3%), heart (0.5-3%), and muscle and subcutaneous tissues (0.5-4.7%) are affected less frequently [3]. Extrahepatic localization of a hydatid cyst may be primary or secondary. Secondary involvement is mostly seen as a direct spread to proximal tissues due to the cyst’s rupture in the liver and lungs. In our case, the patient had a cystic lesion located under the clavicle bone region which was confirmed with CT imaging and superficial tissue ultrasound. No cystic lesion was detected in lungs and liver.In cases of muscular and subcutaneous hydatid cysts, the main symptom is localized palpable swelling. It is one of the options that should be considered in the differential diagnosis in endemic areas. Although some serological tests such as IHA and indirect immunofluorescence test may help diagnose hydatid cysts in the muscles, the diagnosis of muscular and subcutaneous hydatid cysts is usually made by the presence of scolex during the operation [3]. In cases where muscular cyst hydatid is suspected, diagnostic biopsy or aspiration should be avoided to prevent the disease’s rupture and spread [4,5]. In our case, patient had a history of surgery from the same area and multiple cysts suggesting recurrence infection.
The primary treatment method in cases diagnosed with muscular cyst hydatid is total excision of the cyst [4-6]. The measures taken to prevent contamination during excision are very important. In our case, the patient who had a second hydatid cyst operation from the same site was thought to have recurrence due to contamination in the first operation in addition to patient’s statement that he did not use the prescribed medication. Failure of the patient to use the treatment as recommended could lead to much more serious consequences and present with a clinically disseminated infection [7].
Scolicidal agents that can be used to destroy intracyst daughter vesicles are ethanol, 20-30% hypertonic saline, formaldehyde, 0.5% cetrimide, 0.5% silver nitrate and hydrogen peroxide solutions. The most commonly used scolicidal substance in thoracic surgery operations is hypertonic saline solution with a rate of 20-30%, due to its minimal toxicity. It can be used in the lavage of the cyst content as well as a barrier to prevent the cyst content from contaminating the surrounding tissues after an uncontrolled cyst puncture. As in our case, it is very important to prevent contamination during surgery and postoperative medical treatment to prevent recurrent infections.
Albendazole treatment was started for the patient after excision. Medical treatment with benzimidazole compounds (albendazole-mebendazole) seems to be far from curative treatment. However, these agents can be used for prophylactic purposes to prevent spread and recurrence at least for six months.
In conclusion, the atypical location should not be forgotten in the areas that are considered as endemic for cyst hydatid. Cyst hydatid should not be forgotten in the differential diagnosis of cystic mass lesions in muscle and subcutaneous tissues. Attention should be paid to perioperative contamination, and postoperative medical treatment support should be provided to prevent the recurrence.
Declaration of conflicting interests
The authors declared no conflicts of interest with respect to the authorship and/or publication of this article.
Funding
The authors received no financial support.
Authors’ contributions
FC, CH: conceived and designed the current case report, co-wrote the paper, FC: collected the clinical data. The authors discussed the case under the literature data together and constituted the final manuscript.
Reference
1) Sayır F, Çobanoğlu U. Yöremizin Endemik Paraziter Hastalığı: Kist Hidatik. Van Tıp Dergisi 2013; 20: 288-93.
2) Morar R, Feldman C. Pulmonary echinococcosis. Eur Respir J 2003; 21: 1069-77.
3) Di Gesu G, Picone A, La Bianca A, Massaro M, Vetri G. Muscular and subcutaneus hydatidosis. Minerva Med 1987; 30: 835-40.
4) Tatari H, Baran O, Sanlidag T, Gore O, Ak D, Manisalı M, et al. Primary intramuscular hydatidosis of supraspinatus muscle. Arch Orthop Trauma Surg 2001; 121: 93-4.
5) Duncan GJ, Tooke SM. Echinococcosis infestation of biceps brachii. Clin Orthop 1990; 261: 247-50.






