Summary
Background: To enhance postoperative outcomes in patients having video- assisted thoracic surgery (VATS) for spontaneous pneumothorax, it is necessary to determine the difference between the uses of each VATS treatment in such patients. Previous studies have revealed a discussion over the preference of one technique over the other.Materials and Methods: A comparative study was conducted on spontaneous pneumothorax patients (primary or secondary) undergoing VATS in Assiut University Heart Hospital from January 2017 till April 2019. Patients included in our study were prominent bullous forms in PSP pneumothorax lines, recurrent pneumothorax, bilateral pneumothorax, previous history of contralateral pneumothorax, and spontaneous hemothorax, air leakage more than five days with drainage catheter for first-episode patients. Patients were divided into two groups as group A patients who underwent uniport VATS procedure, and group B patients who underwent biport VATS procedure.
Results: The study included 32 patients, 22 were primary spontaneous pneumothorax (PSP), while 10 were secondary spontaneous pneumothorax (SSP). The male to female ratio (MF ratio) was 3.2:1. The mean ± SD for age was 30.04 ± 10.245 in PSP and was 50.43 ± 9.071 in SSP. Eighteen patients underwent uniport VATS, and 14 underwent biport VATS. The mean time for operation was 81.5 ± 33.74 in uniport VATS versus 109.79 ± 25.37 in biport VATS (p = 0.014). No significant statistical difference was found between uniport and biport VATS regarding pain, air leak, complications, hospital stay, recurrence, and mortality. Despite no statistical difference regarding mortality (p = 0.492), there were two mortalities in the uniport VATS group known as interstitial pulmonary fibrosis.
Conclusions: We concluded that there are no differences between both techniques except for operative time.
Introduction
Pneumothorax is a collection of air within the pleural sac; the incidence was reported to be 37 per 100,000 population per year in the United Kingdom. The incidence differs between men and women, being lower in women due to the 6:1 male to female ratio. The primary issue is a recurrence, which occurs at a rate of between 20% and 50%. The majority of recurrences occur during the first year [1,2].Pneumothorax can be classified into spontaneous and non-spontaneous. The spontaneous type is classified into primary (PSP) and secondary (SSP) [3]. The PSP is usually diagnosed in young males, smokers, and tall with no underlying lung disease, while the secondary type is usually diagnosed in older males with a previous history of lung diseases, mostly chronic obstructive pulmonary diseases (COPD). However, PSP occurrence in patients without underlying lung diseases, there are pathological changes in the lung known as emphysema-like changes (bullae/ blebs) [4].
Management of pneumothorax focuses on evacuating air from the pleural space to restore lung function and prevent further recurrences. Management options range from less invasive methods as simple observation, simple aspiration (with a catheter, with immediate removal of the catheter after pleural air is evacuated), insertion of a chest tube, and pleurodesis to more invasiveness, including video- assisted thoracic surgery (VATS) and thoracotomy. The approach selection depends on the size of the pneumothorax, the severity of symptoms, whether there is a persistent air leak, and whether the pneumothorax is primary or secondary [5-7]. The choice of surgical approach is a debate despite the statement of ERS (European Respiratory Society) for pneumothorax, which stated that VATS is the gold standard for surgery, yet the choice of VATS approaches, whether uniportal or multiport, fails to have a consensus. We assume that using uniportal VATS will encourage more patients to have their surgery performed as incision will be the chest tube size only and will get them the same clinical outcomes.
Methods
This is a comparative study included a total coverage of all patients who are presented to our hospital for surgery for spontaneous pneumothorax, whether primary or secondary starting from January 2017 to April 2019, and who fulfilled the inclusion criteria after filling the informed consent and ethical committee approval of Assiut University, Faculty of Medicine (No:17200669). Patients with evident bullous forms in PSP pneumothorax lines, recurrent pneumothorax, bilateral pneumothorax, previous history of contralateral pneumothorax, and air leakage for more than five days with drainage catheter for first-episode patients are all eligible. Patients who met the inclusion criteria will be divided into two groups: group (A) patients underwent uniport VATS procedure, and group (B) patients underwent multiport VATS procedure. Exclusion criteria included the patient’s refusal or reoperation case (for other thoracic diseases rather than pneumothorax).Preoperative variables include age, gender, smoking history, associated comorbidities, addiction history, the indication of surgery, the presence of morbidities (e.g., diabetes mellitus, systemic steroid intake, collagen, and autoimmune diseases and/or cardiac diseases), chest tube insertion (either applied or not before operation), duration of air leakage in patients with the intercostal tube. Intervention variables include date and time of surgical intervention, the procedure performed (uniport VATS, multiport VATS), intraoperative findings (i.e., pleural adhesions visible bleb, site of the bleb, clotted hemothorax etc.), surgical technique used, i.e., staplers, conventional sutures or ligation, operative time (from port opening/trocar insertion to skin closure), and method of pleurodesis (apical pleurectomy, pleural abrasions, or chemical pleurodesis). Post-intervention variables include postoperative pain score and need for opioid analgesics, duration of air leakage, complications (wound infection, recurrence, and need for intensive care unit admission), hospital stay, and morbidity and mortality.
Statistical Analysis
Data were collected from operative notes on the institutional data base on excel sheath. IBM SPSS version 22.0 (IBM Corporation -http://www.spss.com) was used for data analysis. Mean, standard deviation, median, frequency, and percentage were used as descriptive statistics for demographic data such as age, gender and other variables as smoking, diagnosis, and addiction history. Mann Whitney-test was used as non-parametric test of significance for comparison between two sample means. Fisher’s exact and Monte Carlo exact tests were used to analyze categorical variables. P-value was considered statistically significant when it was less than 0.05.
Results
During the study time frame, about 121 patients diagnosed with pneumothorax were admitted to our university hospital. Around 79 of them were treated conservatively via aspiration and/or chest tube, and 42 patients underwent surgery for pneumothorax. We found that 32 patients during the period of the study were eligible for inclusion criteria and underwent VATS wedge resection and mechanical pleurodesis for spontaneous pneumothorax (Primary spontaneous pneumothorax PSP (n = 22) and Secondary spontaneous pneumothorax SSP (n = 10) by uniport or multiport technique according to surgeon preference (Figure 1).
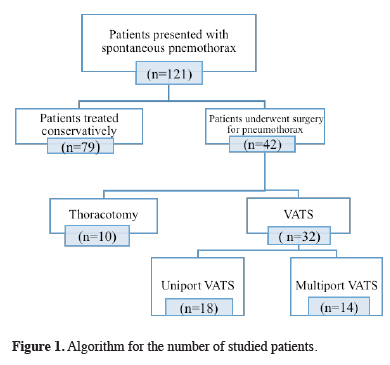 Click Here to Zoom |
Figure 1: Algorithm for the number of studied patients. |
The male to female ratio (MF ratio) was 3.2:1. The mean ± SD for age was 30.04 ± 10.25 in PSP and was 50.43 ± 9.07 in SSP. While 75% were smokers, all of them were males, and 25% were nonsmokers. We encountered that 31.2% had associated comorbidities (eight cases have chronic obstructive pulmonary diseases (COPD) (25%), and two cases with interstitial pulmonary fibrosis (6.3%) (Table 1). Thirty cases were unilateral (21 cases right, and nine cases left), and two were bilateral.
Table 1: Demographic data distribution in uniport and multiport VATS techniques.
Uniport VATS technique was performed in 56.3%, while the multiport technique was performed in 43.8%. In cases that performed in the uniport group, three cases were addicted, while no cases were addicted in multiport technique, the addicted cases were using tramadol (one case), hashish (one case), and both opiate and tramadol (one case).
All cases underwent stapling at the base of bleb or bullae, with two cases need the addition of suture to the stapler line due to stapler failure, which was complete or partial (6.3%). The resection was for apical bleb/bullae in all cases (100%), with one case needed resection for another posterior segmental bleb in the upper lobe (3.1%), and one case with superior segmental blebs in the lower lobe (3.1%). Surgical pleurodesis was performed in all cases with two different methods, first was pleurectomy (43.8%) which was performed at the beginning of the experience with the VATS technique, and the second pleural abrasion was performed by brushing the parietal pleura (56.3%).
The mean operative time (minutes) was 81.5 ± 33.74 in uniport technique versus 109.79 ± 25.37 in multiport technique with a significant statistical difference (p = 0.014).
Postoperative complications were reported in 15.6% of all cases. Complications were reported in three cases in the uniport technique versus two cases in the multiport technique with no statistical significance (p = 0.672). The complicated cases in uniport technique were SVT (supraventricular tachycardia) (n = 1, 5.6%) which need intensive care unit admission for two days, recurrence (n = 1, 5.6%), wound dehiscence (n = 1, 5.6%). The recurrence was reported in patients with bilateral pneumothorax, which occurred after seven days of discharge and was managed conservatively with no need for another intervention. The wound dehiscence was noticed in patients with interstitial pulmonary fibrosis (IPF) on corticosteroids treatment perioperatively. In the multiport group, complications were prolonged air leak (n = 1, 7.1%) and conversion to open thoracotomy due to complete stapler failure (n = 1, 7.1%).
Regarding pain scores, it was found that there was an insignificant relationship (p = 0.386) between both groups. Moreover, it was found that the mean duration (in days) of air leak was (3.50 ± 1.80) in the uniport technique, while it was (3.64 ± 3.59) days, in multiport technique, which was statistically insignificant (p = 0.289). Relatively, the mean duration of the intercostal tube was (4.22 ± 1.48) days, after the uniport technique compared to multiport technique (4.79 ± 3.47) days, which also statistically insignificant as p = 0.538 (Table 2).
Table 2: Postoperative outcomes.
The postoperative stay was measured in days, and the mean was statistically insignificant among the compared groups (p = 0.466). Mortality was reported in two patients among the group of uniport VATS technique (11.1%), while no mortality was reported in multiport technique, which indicated no statistically significant difference (p = 0.492). The two mortality patients were patients with interstitial pulmonary fibrosis (IPF).
Discussion
There is a notable evolution in the surgery for pneumothorax over the last years. The open thoracotomy and pleural abrasion were the main surgery for pneumothorax described by Tyson and Crandall in 1941 [8]. Recently, VATS has offered more advantages over open thoracotomy regarding postoperative stay, operative time, chest tube duration, and postoperative pain [9].Rocco et al introduced single-incision thoracoscopic surgery in 2004 [10]. At that time, the single incision laparoscopic surgery (SILS) port was not in use. One of the biggest reasons for the lack of progress of such technique is that surgeons found the process difficult without a specialized port. It was not easy to insert a 5-mm scope, an endograsper, and a stapler at the same time through a 2.5 cm incision. Incompatibility among instruments, the limited endoscopic field of view, and angulation management of staplers were added to the difficulty.
Chen et al published similar results on 40 patients over 6 months who underwent surgery for primary spontaneous pneumothorax comparing uniport VATS with triport VATS where he uses single incision laparoscopic port (SILS) in Uniportal cases while we don’t use (SILS) as we work from the port incision directly [11].
The wide range of patient’s ages in our study was explained by that we included patients with SSP (ten patients in our study, which have a mean age of 50.43 ± 9.071. Despite that, there was no difference in the mean age between both study groups (uniport group and multiport group). Most studies did not have such a wide range of age as they studied only patient with PSP [9,12-14].
We found significantly lower operative time among the uniport group than the multiport group (p = 0.014). Despite many reports clarify that there was no significant difference between the two groups [14], Kutluk et al also reported less operative time among the uniport group [12].
There was no significant difference between the studied groups regarding postoperative complications. A result which coincided with the result of a study conducted by Nachira et al in 2018 [9].
Several studies hypothesized that patients who underwent uniport VATS for pneumothorax had reduced postoperative pain than multiport VATS [9,15]. This was thought as a result of reduced number of intercostal spaces involved, and, in turn, intercostal nerves affected [16]. Moreover, Yang et al proposed that the cause of pain is mechanical pleurodesis [14]. However, we found no difference in the pain score of the patients in both groups regardless the number of ports and method of pleurodesis.
In a study by Nachira et al, it was reported that there was a significantly lower duration of air leak and chest tube duration in uniport VATS compared to multiport VATS (p < 0.001 ) [9]. In another study by Kutluk et al, who were comparing uniport, biport, and triport VATS, they reported no difference among the three procedures as regards the air leak and chest tube duration (p = 0.378) [12]. We reported no statistically significant difference between the two groups, which is consistent with Kutluk et al as our multiport procedure was biport VATS.
The overall hospital stay in both groups in our study was found 5.56 ± 2.01 for the uniport group and 5 ± 2.18 for the multiport group. Also, Kutluk et al reported 3.73 ± 0.22 for uniport, 3.78 ± 0.20 for biport, and 4.48 ± 0.36 for triport [12]. The diagnosis of secondary spontaneous pneumothorax was reported in 10 cases in our study (4 cases underwent uniport VATS and 6 cases underwent biport VATS) as many studies reported a higher incidence of prolonged air leak and complication due to associated COPD and increased number of blebs/bullae in SSP [15,19-21]. Another reason in our study is that the patient stays for another day after removing the chest tube because of our postoperative nursing care institutional protocol.
Regarding recurrence in comparing uniport VATS with multiport VATS, Nachira et al, also reported no significant differences between the two procedures [9]. In a study by Kutluk et al, they compared uniport VATS with biport and triport VATS, the overall recurrence rate was 5%, and it found no significant difference among the three groups [12]. The recurrence was reported in only one case in our study, with an overall recurrence rate of 3.13%. The recurrent case was within the uniport group with no recurrence reported within the multiport group with no significant difference between both procedures.
Notably, the recurrent case underwent pleural abrasion as surgical pleurodesis and did not need another intervention and was managed conservatively. Caecilian et al, in a study of 107 patients, showed a significant reduction in pneumothorax recurrence after pleural pleurectomy (PP) compared to pleural abrasion (PA) [21]. Even though both techniques were performed via the VATS approach. However, Ling et al compared the effects of pleural abrasion with other PSP treatment interventions in 2015 [22]. It was concluded that pleural abrasion and pleurectomy result in the same recurrence rates, but pleurectomy shows greater postoperative pain and more frequent complications, such as acute postoperative bleeding. Another explanation for recurrence in our case was that this case was operated for bilateral pneumothorax on the same session; while the patient in the supine position, the surgeon might be unable to do pleural abrasion for the whole circumference of the apical pleura in this position in comparison to lateral decubitus where lung drop to the mediastinum and the whole circumference of the pleural can be abraded.
Compared to the multiport-port VATS group, Nachira et al reported that there was no significant difference in the uniport VATS group in terms of mortality, with an overall mortality of 0% [9]. Consistently, we reported no significant difference between both multiport and uniport regarding mortality. However, we reported mortality in two cases among the uniport group with an overall mortality rate of 6%. The preoperative comorbid status of the two cases reported as fatal should be considered because both had IPF and suffered postoperative respiratory failure, raising the question of surgery’s suitability in IPF patients.
Nishimoto et al revealed that treatment of IPF patients complicated by pneumothorax is complicated as the lung is stiffer due to parenchymal fibrosis and associated with a high recurrence rate (70%) [23]. A common procedure is VATS which the intervention is advocated to treat prolonged air leaks in some patients and prevent recurrences in all patients with direct closure of the air leak, stapling/resection of any visible bleb, and mechanical pleurodesis (e.g., abrasion with dry gauze). However, it was concluded that surgical treatment for IPF patients complicated by pneumothorax has a dismal prognosis with high morbidity [23].
In conclusion, VATS is a milestone approach for surgery for pneumothorax with approved safety. In comparison between uniport VATS and multiport VATS, there was no clear evidence about which is superior to another and there were no differences between both techniques in most points that were studied except for operative time.
Declaration of conflicting interests
The authors declared no conflicts of interest with respect to the authorship and/or publication of this article.
Funding
The authors received no financial support for the research and/or authorship of this article.
Ethics approval
The study was approved by the institutional review board of Assiut University, Faculty of Medicine, Egypt
(No: 17200669).
Authors’ contribution
MS; collected all literatures and wrote the whole review, HE; helped in collecting the literatures and drafted the review, AE; helped in the discussion and drafting the review. All authors have read and approved the manuscript.
Reference
1) Sahn S, Heffner J. Spontaneous pneumothorax. N Engl J Med 2000; 342: 868-74.
2) Kucharczuk JC. The role of VATS pleurodesis in the management of initial primary spontaneous pneumothorax. In Difficult Decisions in Thoracic Surgery (Second Edition): An Evidence-Based Approach, Ed. Ferguson MK, Springer London, 2011: 401-7.
3) Costumbrado J, Ghassemzadeh S. Spontaneous Pneumothorax. In: StatPearls Publishing, 2020.
4) McKnight CL, Burns B. Pneumothorax. In: StatPearls Publishing, 2020.
5) Sakamoto T, Nishio W, Okada M, Harada H, Uchino K, Tsubota N. Management of air leak after pulmonary resection. Japanese J Thorac Cardiovasc Surg 2004; 52: 292-5.
6) Henry M. BTS guidelines for the management of spontaneous pneumothorax. Thorax 2003; 58: 39-52.
7) Baumann MH, Noppen M. Pneumothorax. Respirology 2004; 9: 157-64.
8) Tyson MD, Crandall WB. The surgical treatment of recurrent idiopathic spontaneous pneumothorax. J Thorac Surg 1941; 10: 566-70
9) Nachira D, Ismail M, Meacci E, Zanfrini E, Iaffaldano A, Swierzy et al. Uniportal vs. triportal video-assisted thoracic surgery in the treatment of primary pneumothorax - A propensity matched bicentric study. J Thorac Dis 2018; 10: S3712–9.
10) Rocco G, Martin-Ucar A, Passera E. Uniportal VATS wedge pulmonary resections. Ann Thorac Surg 2004; 77: 726-8.
11) P. R. Chen PR, C. K. Chen CK, Lin, Y. Sen Y, H. C. Huang HC, J. S. Tsai JS et al. Single-incision thoracoscopic surgery for primary spontaneous pneumothorax J Cardiothorac Surg 2011; 6: 1-4.
12) Kutluk AC, Kocaturk CI, Akin H, Erdogan S, Bilen S, Karapinar K et al. Which is the Best Minimal Invasive Approach for the Treatment of Spontaneous Pneumothorax? Uniport, Two, or Three Ports: A Prospective Randomized Trail. Thorac Cardiovasc Surg 2018; 66: 589-94.
13) Salati M, Brunelli A, Xiume F, Refai M, Sciarra V, Soccetti A et al. Uniportal video-assisted thoracic surgery for primary spontaneous pneumothorax: clinical and economic analysis in comparison to the traditional approach. Interact Cardiovasc Thorac Surg 2008; 7; 63-6.
14) Yang HC, Cho S, Jheon S. Single-incision thoracoscopic surgery for primary spontaneous pneumothorax using the SILS port compared with conventional three-port surgery. Surg Endosc 2013; 27: 139-45, 2013.
15) Rocco G, Martucci N, La Manna C, Jones DR, De Luca G, La Rocca A et al. Ten-year experience on 644 patients undergoing single-port (Uniportal) video-assisted thoracoscopic surgery. Ann Thorac Surg 2013; 96: 434-8.
16) Mcelnay PJ, Molyneux M, Krishnadas R, Batchelor TJ, West D, Casali G. Pain and recovery are comparable after either uniportal or multiport video-assisted thoracoscopic lobectomy: an observation study. 2015; 47: 912-5.
17) Ichinose J, Nagayama K, Hino H, Nitadori JI, Anraku M, Murakawa T et al. Results of surgical treatment for secondary spontaneous pneumothorax according to underlying diseases. Eur J Cardiothorac Surg 2016; 49: 1132-6.
18) Tschopp JM, Bintcliffe O, Astoul P, Canalis E, Driesen P, Janssen J et al. ERS task force statement: diagnosis and treatment of primary spontaneous pneumothorax Task force report ERS statement. Eur Respir J 2015; 46: 321-35.
19) Macduff A, Arnold A, Harvey J. Management of spontaneous pneumothorax: British Thoracic Society pleural disease guideline 2010. Thorax 2010; 65: ii18-31.
20) M. H. Bauman MH, C. Strange C, J. E. Heffner JE, R. Light R, T. J. Kirby TJ, J. Klein J et al. Management of spontaneous pneumothorax: An American College of Chest Physicians Delphi Consensus Statement. Chest 2001; 119: 590-602.
21) Ng C, Maier HT, Kocher F, Jud S, Lucciarini P, Öfner D et al. VATS Partial Pleurectomy Versus VATS Pleural Abrasion: Significant Reduction in Pneumothorax Recurrence Rates After Pleurectomy. World J Surg 2018; 42: 3256-62.






