2Department of Respiratory Medicine, Erciyes University, Faculty of Medicine, Kayseri, Turkey
3Department of Otorhinolaryngology, Erciyes University, Faculty of Medicine, Kayseri, Turkey DOI : 10.26663/cts.2022.017
Summary
Tracheal tumors are quite rare, with an incidence of 2.6 per 1,000,000 persons. Tracheal malignant melanomas are one of the least common types among these tumors due to the lack of natural epithelial tissue of melanocytes. There is no optimal treatment method for tracheal malign melanomas because they have an aggressive nature, have limited life expectancy and occur very rarely. This paper discusses the case of and treatment methods fora patient who was initially suspected to have a foreign body aspiration because of presenting to hospital with acute airway obstruction.Introduction
Tracheal tumors are a very rare form of cancer that occurs at a rate of 2.6 per 1,000,000 persons. Within this group of tumors, which mostly consists of squamous cell carcinomas and adenoid cystic carcinomas, malignant melanomas are rare and the least known type [1].Malignant melanomas constitute only 1% of the primary tracheal cancers even in the most comprehensive studies on primary tracheal tumors in the literature [1].
Depending on the limited number of studies, there is only limited information, if any, regarding the formation mechanisms of primary tracheal malign melanomas, their clinical course, optimal treatment methods, and their life expectancy, presented only as case reports for a limited number of patients.
Case Presentation
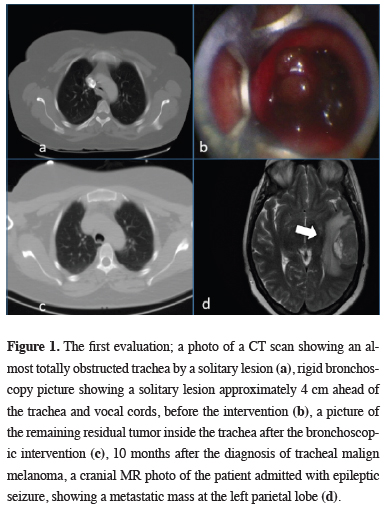
A 38-year-old female patient with no known history of disease presented to the emergency department of an external center due to the shortness of breath that had increasingly continued for 1 month. She was referred to our hospital in July 2019 because of suspected foreign body aspiration due to the presence of respiratory acidosis (PaCO2: 79 mmHg) and prominent stridor in the arterial blood gas examined. The patient was found to experience tachypnea and prominent expiratory stridor in the examination and her blood gas PaCO2 level was 50.9 (35-45) mmHg.The thoracic tomography report stated an appearance of a possible foreign body in the proximal trachea that obstructed the lumen almost completely (Figure 1a). The patient was immediately taken for the video rigid bronchoscopy procedure. A solitary lesion was observed in the trachea approximately 4 cm beyond the vocal cords, obstructing the lumen almost completely (Figure 1b). The lesion was dissected and removed from the rigid bronchoscope. During the procedure, it was determined that the lesion extended to the carina and originated from the trachea posterior wall. No massive bleeding was observed in the patient, who underwent debulking. However, cold saline solution was required from time to time. The total volume of the extracted material was 3 cubic centimeters.
 Click Here to Zoom |
Figure 1: The first evaluation; a photo of a CT scan showing an almost totally obstructed trachea by a solitary lesion (a), rigid bronchoscopy picture showing a solitary lesion approximately 4 cm ahead of the trachea and vocal cords, before the intervention (b), a picture of the remaining residual tumor inside the trachea after the bronchoscopic intervention (c), 10 months after the diagnosis of tracheal malign melanoma, a cranial MR photo of the patient admitted with epileptic seizure, showing a metastatic mass at the left parietal lobe (d). |
In the control process, the PaCO2 value (38.6 mmHg) of the blood gas of the patient, who was taken to the postoperative intensive care unit, regressed to the normal range. The patient’s stridor and complaint of shortness of breath regressed.
PET-CT was requested for the patient, who did not experience hemoptysis during the follow-up. The PET-CT imaging showed a residual lesion in the trachea, located about 2 cm proximal to the carina, and 9x8 mm in size with a SUV max value of 2.7 (Figure 1c. In addition, there were metastatic (SUV max: 4.9) nodules in both lungs, the largest of which was 15x9 mm.
Medical treatment was planned for the patient, who had been diagnosed with tracheal malignant melanoma, as a result of the pathology. It was learned that the patient had been diagnosed with melanoma by skin biopsy 3 years ago but had not received any treatment. The patient began to be treated with Dabrafenib + Trametinib in September 2019.
Five months after the diagnosis, the patient presented to the hospital again due to the shortness of breath and hemoptysis and was intubated and hospitalized in the intensive care unit. The patient underwent video rigid bronchoscopy again. A lesion was detected in the distal part of the trachea, approximately 2 cm from the carina. The lesion narrowing the trachea by 70% was initially cauterized with electrocautery. Then, debulking was carried out with rigid bronchoscopy. The lesion was removed in two parts, the first of which measured 1.7x0.7x0.6 cm and the second of which measured 0.9x0.8x0.7 cm. After debulking, a fiberoptic bronchoscope was passed through a rigid bronchoscope, and cryotherapy was applied under the lesion. The patient, who was intubated postoperatively, was extubated on the third day after the intervention.
Radiotherapy (30x216cGy, totally 6480cGy) was applied to the patient, who was discharged after her clinical course had improved, in March 2020. Upon the patient’s epileptic seizure in the 10th month after diagnosis, a cranial MRI was taken, which showed metastasis in the left parietal area (Fig 1d). During the examinations, progression of lung metastases and multiple metastases in the liver were also detected. The patient died 11 months after the diagnosis.
Discussion
Tracheal malignant melanomas are cancers that occur sporadically even among primary tracheal cancers [2]. There is no study in the literature involving patient series.One of the main reasons why they are so rare is that melanocytes are not the natural epithelium of the respiratory tract. Although there is no certain information on how melanocytes reach this area, there are several theories. These involve the migration of melanocytes during embryogenesis, the transformation of respiratory cells into melanocytes and the differentiation of neuroendocrine cells into melanocytes [3].
As in tracheal cancers, the clinical course can include cough, shortness of breath, and hemoptysis [1,2]. Since they are not included in the group of diseases that are suspected first by clinicians during diagnosis as they occur so rarely, patients in this group can also present to the hospital with airway obstruction, as was the case with our patient. Chest radiography and computed tomography can be used in the first step and to detect the tumor localization. PET-CT can be helpful in diagnosis and treatment planning and to indicate the presence of distant metastases [1,2].
Although malignant melanoma can be diagnosed histopathologically by S-100, melan-A, and HBM-45, it may not be distinguished from primary metastasis. Therefore, diagnostic criteria have been developed to distinguish true primary tracheal malignant melanomas from metastases. These criteria include i) solitary mass presence, ii) invasion from the epithelia to the submucosa iii) absence of a previously detected or excised skin lesions in the patient, iv) absence of a family history of skin disease v) provision of typical histopathological confirmation by electron microscopy or immunohistochemistry, and vi) ‘dropping off’ of melanoma cells together with junctional changes in the mucosa [4]. It was not considered primary because the patient had a previous skin biopsy.
There is no data on the survival time of patients with tracheal malignant melanomas. Considering the studies known in the literature including the one with the largest series, the 5-year survival rate of patients with primary tracheal cancers is reported to be between 15-27% [1,2]. Considering that malignant melanomas have the shortest known doubling time with 48 days, with the exception of anaplastic thyroid cancer and testicular cancer, the survival of patients is expected to be much shorter [5].
Except for one patient who underwent tracheal resection, almost all tracheal malign melanoma patients in the literature have been reported to die shortly after diagnosis [6].
Since tracheal malign melanomas are very rare and aggressive in nature, there is no consensus on an optimal treatment method. There are studies reporting that resection and end-to-end anastomosis prolong survival of all patients with no metastasis in primary tracheal cancers regardless of the histopathological type [1,7]. However, a study conducted with the largest series of patients in the literature reported that resection could be applied to only 14 of 308 patients and that surgery might not be effective upon life expectancy [2]. Tracheal reconstruction techniques, and debulking surgery, as we have done with our patient, have a place in the treatment because of the necessity of providing airway patency [1-2].
A recent study showed that bronchoscopic interventions of secondary pulmonary cancer may increase the average life expectancy of the patients. The life expectancy of this group of patients after the diagnosis was 10 ± 13.1 months. However, after the bronchoscopic interventions positive effects on life expectancy were seen. Also, in the same study, the mortality rate due to complications of the bronchoscopic interventions was found to be 0%.In our case, we performed two bronchoscopic interventions with no major complications to be mentioned. We are convinced that in these types of patients, bronchoscopic interventions can be applied safely [8].
In addition, although radiotherapy has a place in local treatment, its effectiveness on life expectancy has not been demonstrated. Chemotherapy and immunotherapy are used in the treatment of malign melanoma. Dacarbazine-based treatment protocols are preferred in chemotherapy whereas Vemurafenib (2011), Dabrafenib (2013) and Trametinib (2013) are used in immunotherapy. Programmed death-1 checkpoint (PD-1) inhibitors such as Pembrolizumab are also used in the treatment of malignant melanoma. Furthermore, in the literature we found information about using Pembrolizumab as a medical treatment choice which may be used during pregnancy [9].
When we examined the literature, we found a case similar to ours. In that case, after the patient was diagnosed with malign melanoma he was treated with interferon. Seven years later the patient developed lung metastasis. At the follow-up stage, in a 3 weeks period, a malign melanoma causing %90 obstruction of the patient’s airway was detected. Similar to our case the patient was treated with rigid bronchoscopy [10].
Especially after the first bronchoscopic intervention, and as a different approach, a stent or a course of radiotherapy could be applied. In our case, the short life expectancy of the patient and the low complication risk of the rigid bronchoscopic intervention were the reasons behind choosing this approach.
As a result, although there are no definitive data on this extremely rare type of tracheal cancer, resection and end-to-end anastomosis seem to be good options, if applicable. In order to provide airway patency in inoperable patients, debulking surgery can be performed safely without causing massive bleeding, as we applied to our patient twice.
Declaration of conflicting interests
The authors declared no conflicts of interest with respect to the authorship and/or publication of this article.
Funding
The authors received no financial support
Authors’ contributions
OFD; conception and design of the work, acquisition, analysis, interpretation of data, OO; acquisition, design of the work, BB; interpretation of data, analysis, design of the work, AV; acquisition, interpretation of data, OT;interpretation of data, analysis
Reference
1) Urdaneta AI, James BY, Wilson LD. Population based cancer registry analysis of primary tracheal carcinoma. Am J Clin Oncol 2011; 34: 32-7.
2) Honings J, van Dijck JA, Verhagen AF, van der Heijden HF, Marres HA. Incidence and treatment of tracheal cancer: a nationwide study in the Netherlands. Ann Surg Oncol 2007; 14: 968-76.
3) Jennings TA, Axiotis CA, Kress Y, Carter D. Primary malignant melanoma of the lower respiratory tract. Report of a case and literature review. Am J Clin Pathol 1990; 94: 649-55.
4) Jensen OA, Egedorf J. Primary malignant melanoma of the lung. Scand J Respir Dis 1967; 48: 127-35.
5) Henschke CI, Yankelevitz DF, Yip R, Reeves AP, Farooqi A, Xu Dewt al. Lung cancers diagnosed at annual CT screening: volume doubling times. Radiology 2012; 263: 578-83.
6) Terra RM, Minamoto H, Junqueira JJ, Falzoni R, Pêgo-Fernandes PM, Jatene FB. Tracheal malignant melanoma: successful outcome with tracheal resection. Ann Thorac Surg 2008; 86: 308-10.
7) Figueroa Rodriguez F, Uddin A, Nasr J. Primary Pulmonary Malignant Melanoma Found While Evaluating New Onset Cough: A Case Presentation and Literature Review. Case Rep Pulmonol 2019; 20109: 3867831. doi: 10.1155/2019/3867831.
8) Uğur Chousein EG, Turan D, Özgül MA, Çetinkaya E. Secondary pulmonary malignancies requiring interventional bronchoscopic procedures. Turk Gogus Kalp Damar Cerrahisi Derg 2021; 29: 360-9.






