Summary
Background: COVID-19, a novel coronavirus affecting the respiratory system, was diagnosed in China in December 2019. With the pandemic, many new changes had to be made in thoracic surgery clinics.Materials and Methods: The patients who underwent surgery at Thoracic Surgery Department between March 11, 2020, and October 11, 2020, during the COVID-19 pandemic were evaluated retrospectively. The precautions and new preoperative procedures in our thoracic surgery clinics were analyzed retrospectively.
Results: A total of 1177 patients were treated in thoracic surgery clinics, 299 underwent surgery under general anesthesia during the pandemic, and 948 patients were excluded. Common complications were prolonged air leakage and pleural effusion, and complications occurred in 16.4% of the patients. The mortality rate was 1%. One of the patients with bullae excision due to prolonged air leakage (with COPD) was diagnosed on the fifth postoperative day, another with right pneumonectomy had radiological findings compatible with COVID-19 on the fourth postoperative day, despite negative PCR results four times, and the third patient with thymoma who underwent extended thymectomy without any COVID-19 findings were deceased.
Conclusions: Considering that COVID-19 increases mortality due to increased inflammation and pulmonary involvement, COVID-19 infection co-occurring surgical interventions of the lung will adversely affect the patient’s prognosis and cause an increase in transmission. While caution should always be exercised in all surgical procedures in the pandemic, more severe precautions should be taken in thoracic surgery operations. Implementing comprehensive protective measures such as preoperative PCR test, thorax CT before surgery, quarantine, and disinfection are essential to control nosocomial infection.
Introduction
The first case of Coronavirus was reported in 1960 and was known as a common cold clinic, which was not fatal until 2002 [1]. In 2003, Coronavirus caused SARS (Severe Acute Respiratory Syndrome) with fatal pneumonia that affected many countries and caused more than 1000 people to die. In 2012, MERS (Middle East Respiratory Syndrome) caused a second epidemic with high mortality pneumonia and showed its effect in many countries. In December 2019, the first COVID-19 (Corona Virus Disease ID- 2019) findings were reported to the World Health Organization (WHO) as a new coronavirus pneumonia agent from Wuhan, China. COVID-19 has lower mortality compared to SARS and MERS (2.3%, 9.5%, and 34.4%, respectively), but it caused an epidemic worldwide in a short time due to its ability to spread much faster than the others [2]. The incubation period is about 1-14 days, primarily symptoms in 2-7 days [3].COVID-19 pandemic is a significant global health threat and has affected all aspects of the healthcare system. Healthcare professionals had to change their daily practice to adapt to this unexpected situation. In the healthcare services provided during the pandemic period with the principle of “First, Do No Harm- Primum non-nocere” the benefit-harm assessment for patients and measures should be taken to minimize the viral exposure of healthcare workers and other patients. Regulations such as predicting and managing the risks of perioperative complications, postponing elective surgeries, and using the intensive care capacity effectively gained importance in this process. Due to the long process of the COVID-19 disease, its long incubation period (1-14 days), and its asymptomatic cases with a frequency of 30-40%, preoperative selection and evaluation of patients to undergo surgery are difficult. The current preoperative evaluation and preparation approach in thoracic surgery clinics during the COVID-19 pandemic process will be discussed in our article.
Methods
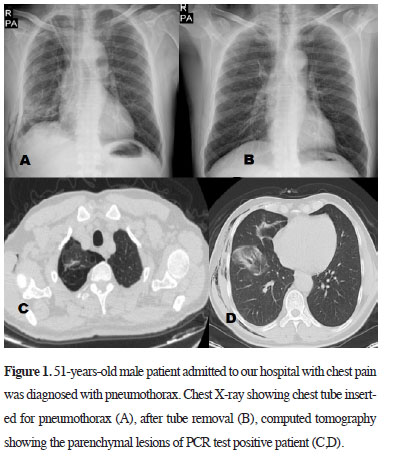
The patients who underwent surgery at Atatürk Chest Disease and Thoracic Surgery Research and Training Hospital, Thoracic Surgery Department, between March 11, 2020, and October 11, 2020, during the COVID-19 pandemic were evaluated retrospectively. Patient demographics, surgical procedures, complications, COVID-19 symptoms, PCR test results, radiologic assessments, and outcomes were evaluated. Procedures like tube thoracostomy for pleural effusion or pneumothorax, closed pleural biopsies, local biopsies, and bronchoscopies that do not require general anesthesia or operating room usage were excluded.Surgical activity changed significantly during the pandemic. Selection criteria for surgical patients are also described according to pandemic pace. In our hospital, in the first fifth month of the pandemic, PCR-positive patients were diverted to COVID-19 hospitals, and treatments of other pulmonary diseases, thoracic oncologic patients, and emergent disorders were carried out more safely. In the second five months of the pandemic, our hospital started giving healthcare services for COVID-19 patients with 20% capacity in the isolated Unit. New protocols were launched to reduce the risk of operating on patients with possible COVID-19, including symptom screening, a polymerase chain reaction test for COVID-19, and computed tomography scans of the chest (Figure 1). The surgery decisions and suitable time were considered according to these findings and protocol.
 Click Here to Zoom |
Figure 1: 51-years-old male patient admitted to our hospital with chest pain was diagnosed with pneumothorax. Chest X-ray showing chest tube inserted for pneumothorax (A), after tube removal (B), computed tomography showing the parenchymal lesions of PCR test positive patient (C,D). |
Patients referred to surgery and living in Ankara are recommended for home isolation preoperatively. Whether they come from another city, they are placed in hospital isolation, and PCR for COVID-19, blood tests, pulmonary function tests, and other deficient laboratory tests are completed during the hospital stay, preoperatively.
Initially, surgeries of patients with severe and urgent conditions such as malignancy were planned priority, and follow-up with radiological or medical treatment was recommended for other conditions. Since we did not predict the progress of the pandemic at first, we prioritized patients whose mortality would increase if they were not treated within two months and other conditions were postponed. Chemotherapy-radiotherapy (neoadjuvant or definitive) was primarily preferred for patients at the limit of operability due to low pulmonary function test results or low-performance status, and then the patients were then re-evaluated after medical treatments.
On the day of admission, we confirmed that the patient was asymptomatic. Preoperative routine blood testing (lymphocyte count, C-reactive protein, ferritin, lactate dehydrogenase (LDH) levels especially confirmed) was requested to check SARS-CoV-2, and PCR tests were applied twice in preoperative 48 hours were also added. Preoperative thorax computed tomography (CT) was evaluated seven days before surgery. After the surgical procedure, patients were treated in a COVID-19-free thoracic surgery intensive care unit (Trauma patients were hospitalized in negative pressure isolated rooms of ICU until their PCR test results came out.). Then they discharge to our thoracic surgery department room that disinfection and droplet precautions were performed. Patients were also placed in an individual room, and only one asymptomatic companion was allowed to accompany and isolated during hospitalization. Visits from family members were not allowed.
The following variables of the patients were determined: Age, sex, comorbidities, physical status, oncological diagnosis, procedure, postoperative complications, length of hospital stay, postoperative respiratory symptoms, time from operation to symptoms, PCR test for SARS-CoV-2, chest CT, chest X-ray, need for hospital re-admission and early postoperative mortality (death within 30 days after the surgical procedure).
Results
Between March 11, 2020, and November 11, 2020, 1177 patients were treated in thoracic surgery clinics, and a 34.8% decrease occurred compared to last year in the same period (1806 patients, last year for the same eight-month period). 299 patients underwent surgery under general anesthesia during the pandemic. 948 patients were excluded due to the study protocol that includes patients with tube thoracostomy for pleural effusion or pneumothorax, closed pleural biopsies, local biopsies, and bronchoscopies that do not require general anesthesia or operating room usage.A total of 299 patients (97 female/202 male) underwent surgery, and the median age of the patients was 50.4 (6-84 years), and hospital stay was 6.2 (0-40) days. 117 (39.1%) of patients had comorbidities. The demographics of the patients are summarized in table 1.
Table 1: Demographics of patients who had elective surgical procedures.
We performed 134 lung resections (120 lobectomies, 11 pneumonectomies, and three sublobar resections). Resections were performed in 32 patients via VATS and 102 with thoracotomy, and 8 of the patients underwent surgery after neoadjuvant chemotherapy. Mediastinal tumor excision was performed in 14 patients, VATS and pleura biopsy in 39, decortication in 39, diagnostic wedge resection via VATS in 44, metastasectomy in 6, bullae excision in 33, exploration for hemothorax in 10, trachea resection in 3, and cyst hydatic surgery in 11 cases. Nine of the patients underwent redo-surgery due to hematoma, hemothorax, and prolonged air leakage complications. Common complications were prolonged air leakage and pleural effusion, and complications occurred in 16.4% of patients (Table 2). Three deaths were recorded in the early stage (the first 30 days after surgery). A prolonged air leakage patient with COPD who was diagnosed with COVID-19 postoperative fifth day, a right pneumonectomy patient whose radiological findings are compatible with COVID-19 on the fourth postoperative day, but negative PCR results four times, and a patient with thymoma who underwent extended thymectomy without any COVID-19 findings were decreased (1%).
Table 2: Postoperative complications.
In the first days of the pandemic, PCR test results were delayed for 2 or 3 days. Preoperative PCR samples were taken twice for each patient for 42 days, but none were positive, and over time, a single sample was taken and continued to be evaluated. By the second peak, we started to apply the PCR test twice again due to the widespread of COVID-19. The surgery decision was reviewed with the updated thorax tomographies within 3-10 days preoperatively. Although there were deficiencies in the first period, PCR was taken from almost all patients, whether they underwent surgery or not. The patients with COVID symptoms or a high risk of contact were not allowed to enter the clinic. If the PCR test result was positive, the patient was isolated in the COVID-19 service. In our study, 5 patients (1.6%) were positive perioperatively. The surgical procedure was postponed due to positive PCR results in 5 of 299 patients scheduled for surgery. Postoperative infiltration compatible with COVID-19 was detected in thorax tomography in 2 patients.
Since March 11, 2020, four nurses, two cleaning staff, and a secretary in the Thoracic Surgery Department, four nurses in Thoracic Surgery ICU, one operating theater staff, two doctors of anesthesia and thoracic surgery departments had COVID-19, and all healed without any complication.
The American College of Surgery (ACS) prepared a guide on March 24, 2020, to classify the hospitals and determine the necessity and urgency of surgery [4]. According to this guideline, Phase 1 hospitals with a small number of COVID-19 infected patients are not yet experiencing a severe increase and are in a period of sufficient intensive care capacity. It defines partially emergencies and surgical indications that can be performed under appropriate conditions. In Phase 2, only emergency surgeries are required in cases where many infected patients are envisaged, limited intensive care facilities or a rapidly increasing number of patients are foreseen. In hospitals of this density, surgery can be performed on patients whose survival will be adversely affected within a few days if surgery is not performed. Phase 3 is situations where all the hospital facilities are directed to COVID-19 patients, and intensive care service or appropriate material supply cannot be provided. In this process, the urgency for surgery should be limited to situations where the patient’s survival will deteriorate within hours if not treated. According to this classification, our hospital services are in phase 1 for the first five months and phase 2 for two months.
Discussion
In the first half of 2020, a historical global crisis started with the COVID-19 outbreak caused by the SARS-CoV-2 Coronavirus. While many people were affected by severe illness, many lost their lives. Along with severe uncertainty in the health system, diagnosis, treatment, and prevention methods that cause concerns about the healthcare workers’ workforce and protective equipment have emerged. While elective surgeries were postponed in addition to changes in standard treatments, emergency surgical margins were frequently scrutinized. However, as urgent care for patients with confirmed or suspected COVID-19 is provided, there is also a concern regarding how to care for patients needing treatment for other diseases can be maintained [5]. There was a 34.8% decrease over the same period last year. This decrease is probably due to the selection of patients according to their urgency, the avoidance of patients to the hospital due to the risk of infection, and the lockdowns. We predict that the number of patients who underwent surgery will increase again with vaccinations, social immunizations, and the ease of the measures taken.With the pandemic, it was necessary to make regulations to minimize infection and use resources efficiently. Due to the urgency of the patients’ medical conditions and the density of pandemic patients, criteria were determined for the optimal use of the remaining facilities. This severe crisis will inevitably affect the diagnosis and treatment process for patients with lung space-occupying lesions. While surgery of some benign lesions may be delayed due to their slow progress, postponing surgery in lung malignancies may change the patient’s prognosis and even result in tumor progression at a level that can threaten life.
In a multidisciplinary retrospective study of 34 patients, Lei et al reported the results of COVID-19 patients who were operated on during the incubation period without knowing they were infected [6].
According to this study, while the need for intensive care was 26.1% in COVID-19 patients who did not undergo surgery, 44.1% of the patients who operated for any reason required postoperative intensive care follow-up due to the development of organ dysfunction or the need for a mechanical ventilator. Advanced age, comorbidity, and prolonged operative time are associated with poor prognosis.
This increased mortality and morbidity caused us to increase the number of precautions before surgery, routine preoperative PCR tests, and treatment planning with appropriate isolation. Preoperative two negative PCR conditions were applied in our clinic for a while. Still, the application was continued by retaking a single PCR sample due to the lack of significant results and loss of economic and time.
Although there are no standard clinical, laboratory, or radiological findings that can be used in preoperative evaluation during the COVID-19 pandemic, we evaluated the possibility of infection in our clinic by setting our standards through detailed preoperative anamnesis, contact history questioning, close fever follow-up, CBC, biochemistry, CRP, coagulation parameters, and naso-oropharyngeal PCR samples, thorax CT taken in the near operative period.
One of the essential steps in diagnosing COVID-19 is the demonstration of nucleic acid amplification by Reverse-Transcriptase Polymerase Chain Reaction (PCR) of SARS-CoV-2 RNA. Thorax computed tomography (CT) sensitivity is 97.2% when evaluated for diagnosis, while PCR sensitivity is only 83.3%. Therefore, evaluating patients with clinical suspicion with thoracic CT is essential. [7]. Serological tests for immunity developed after infection and antibodies produced against SARS-CoV-2 are evaluated with ELISA. After the disease develops, IgM can be detected in the blood on the 12th day and IgG on the 14th day [8].
In the study of Cai et al [9], seven patients who underwent thoracic surgery procedures and were infected with COVID-19 were evaluated. Preoperative tomography images taken two weeks ago were re-examined, and one of the three patients had bilateral ground-glass opacities and died of COVID-19 postoperatively. Also, radiographic changes such as infiltrates, atelectasis, and pleural effusion were found in the early postoperative period in all seven patients.
Procedures that cause intense aerosol formation, such as respiratory function tests and bronchoscopy, are kept to a minimum or not performed in many clinics. In addition to COVID-19 screening, standard preoperative evaluation methods of patients scheduled for surgery are also delayed in the pandemic process.
It is of vital importance to determine the preoperative respiratory capacity in thoracic surgery operations. Likewise, the presence of an endobronchial lesion to be detected preoperatively, observation of a bleeding focus, or bronchoscopic procedures in which the surgical margin is evaluated are evaluation methods that may be decisive for our surgeries.
If the respiratory function tests cannot be performed, evaluating respiratory capacity is feasible with other methods such as a 6-minute walking test, and the stair-climbing test can be done alternatively. Performing detailed preoperative respiratory function procedures (PFT, DLCO, VO2 max) is essential. Be aware of the risks of possible coagulation disorders, thrombosis, and embolism, and if necessary, prophylaxis and early treatment options should be evaluated.
It is essential to share all risks with the patient, provide detailed information, including the risk of infection during the perioperative hospitalization, and make a decision with the patient, if necessary, to refer to alternative treatment methods in cases where surgery cannot be performed.
In conclusion, the COVID-19 pandemic poses a significant challenge in deciding and managing surgical operations in patients with lung cancer and other lung conditions. SARS-CoV-2 is a highly contagious and life-threatening infection. The recent study results from limited cases suggest lung resection surgery may be a risk factor for death in COVID-19 patients during the perioperative period. Therefore, surgical treatment should be done with extreme caution during an epidemic. Implementing comprehensive protective measures such as preoperative PCR test, thorax CT before surgery, quarantine, and disinfection are essential to control nosocomial infection.
Declaration of conflicting interests
The authors declared no conflicts of interest with respect to the authorship and/or publication of this article.
Funding
The authors received no financial support for the research and/or authorship of this article.
Ethics approval
This retrospective analysis was approved by the Health Sciences University, Atatürk Chest Disease and Thoracic Surgery Research and Training Hospital Medical Specialty and Education Committee (No:2020/678).
Authors’ contribution
SH,NS,LNÜA,Fİ,KA,PB,GF,SŞEG; contributed substantially to study design, data analysis and interpretation, and writing of the manuscript, the conception or design of the study, the acquisition, analysis, or interpretation of the study, drafting the work or revising it critically for important intellectual content, final approval of the version to be published and agreed to be accountable for all aspects of the work in ensuring that questions related to accuracy or integrity of any part of the study are appropriately investigated and resolved.
Reference
1) Kumar D, Malviya R, Sharma PK. CoronaVirus: A Review of COVID-19. EJMO 2020; 4: 8-25.
2) Petrosillo N, Viceconte G, Ergonul O, Ippolito G, Petersen E. COVID-19, SARS, and MERS: are they closely related? Clin Microbiol Infect 2020; 26: 729-34.
3) Guan W, Ni Z, Hu Y, Liang WH, Ou C, He J et al. Clinical Characteristics of Coronavirus Disease 2019 in China. N Engl J Med 2020; 382: 1708-20.
4) American College of Surgeons. COVID-19 Guidelines for Triage of Thoracic Patients (2020). www.facs.org/ covid-19/clinical-guidance/elective-case/thoracic-cancer.
5) Jheon S, Ahmed AD, Fang VW, Jung W, Khan AZ, Lee JM et al. General thoracic surgery services across Asia during the 2020 COVID-19 pandemic. Asian Cardiovasc Thorac Ann 2020; 28: 243-9.
6) Lei S, Jiang F, Su W, Chen C, Chen J, Mei W et al. Clinical characteristics and outcomes of patients undergoing surgeries during the incubation period of COVID-19 infection. EClinicalMedicine 2020 5; 21: 100331.
7) Long C, Xu H, Shen Q, Zhang X, Fan B. Diagnosis of the Coronavirus Disease (COVID-19): rRT-pCR or CT? Eur j Radiol 2020; 126: 108961.






