Summary
Bronchoscopy of a 58-year-old female patient who complained of dyspnea after prolonged intubation revealed stenosis of approximately 2 cm in length at a distance of 2 cm from the carina. Upon that, the patient underwent tracheal resection and reconstruction with VATS using 3 ports. Operations can be performed safely through minimally invasive surgical approaches for tracheal stenoses at the thoracic level.Introduction
Tracheal stenosis most commonly occurs due to prolonged intubation. The main treatment modality for postintubation tracheal stenosis (PITS) is surgery. While open surgical approaches are frequently used in treatment, the publications in the literature on endoscopic surgical treatments are limited [1,2].In this article, we evaluated our case who underwent tracheal resection and reconstruction with video-assisted thoracoscopic surgery (VATS), which is a rare approach in distal tracheal stenosis, based on the literature.
Case Presentation
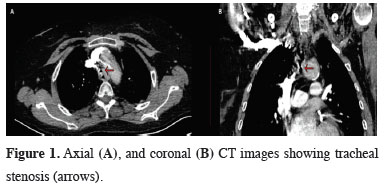
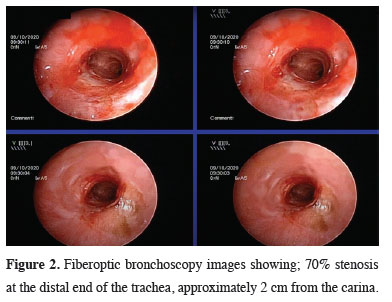
A 58-year-old female patient has known diagnoses of diabetes, congestive heart failure, hypothyroidism, and peripheral neuropathy. The patient has a history of prolonged intubation due to myocardial infarction. The patient complains of severe shortness of breath after extubation. Thorax tomography revealed an area of stenosis starting approximately 2 cm above the carina (Figure 1). Bronchoscopy revealed a mixed-type stenotic tracheal stenosis area accompanied by malacia, narrowing the lumen by 70% in a 2 cm segment, ending 2 cm proximal to the carina (Figure 2). Tracheal resection with VATS was decided for the treatment of stenosis at the level of the thoracic trachea. A one cm camera port incision was made in the posterior axillary line from the 7th intercostal space and an incision was made from the 4th intercostal space for intubation, in the left lateral decubitus position. A 4 cm utility incision was made in the third intercostal space. Since the patient’s tracheal stenosis area was 2 cm proximal to the carina, the stenotic trachea was resected, and then cross-field ventilation was started (Figure 3). The tracheal anastomosis was performed continuously with 3-0 polypropylene (PROLENE®, Ethicon, Inc.) sutures. Expansion of the right lung was prevented by using a right endobronchial blocker during the operation. The patient was discharged on the 7th postoperative day without complications. The patient is observed to be healthy in the first postoperative year, and the follow-up continues. Written informed consent was obtained from the parents for publication of her data.
 Click Here to Zoom |
Figure 1: Axial (A), and coronal (B) CT images showing tracheal stenosis (arrows). |
 Click Here to Zoom |
Figure 2: Fiberoptic bronchoscopy images showing; 70% stenosis at the distal end of the trachea, approximately 2 cm from the carina. |
 Click Here to Zoom |
Figure 3: Intraoperative pictures showing; resection of the trachea (A), and reconstruction with continued sutures (B). |
Discussion
Currently, major surgical operations can be performed through minuscule incisions by the advanced technology. There are quite a few publications in the literature on the endoscopic surgical treatment of benign tracheal stenosis. The most remarkable reason for this is the technical challenges of VATS. Many surgeons are reluctant to use this technique, particularly due to difficulties such as allowing intraoperative ventilation and performing the anastomosis in a narrow space. The concern about an intraoperative thoracoscopic major bleeding or the technical complication of performing radical resections by VATS in advanced cases are the main reasons for the low adoption. Major surgical operations (Tracheal resection and reconstruction, vascular and/or bronchial sleeve resection and reconstruction) can be performed through minuscule incisions by the advanced technology.The largest series in the literature is the series performed by Jiang et al [3] through VATS on a patient with 12 tracheal distal end stenosis with spontaneous breathing. The authors suggested that mobilization of the trachea is easier when the endotracheal tube is not used, and therefore spontaneous ventilation is effective. In our case, we preferred ventilation with an endotracheal tube, the most important reasons for this are to avoid potential intraoperative hypoxia and to minimize intraoperative complications.
During the operation anastomosis is much more challenging compared to open surgery because the intubation tube advances to the surgical site during intraoperative ventilation. Specifically, jet ventilation or extracorporeal support (ECMO-Extracorporeal Membrane Oxygenation) can be preferred to prevent this situation. Ko et al and Hoetzenecker et al have also stated that ECMO is much safer in airway surgery [4,5]. We preferred cross-field intubation at the onset of anastomosis in our case. Towards the end of the anastomosis, we performed selective lung ventilation using a right endobronchial blocker through the endotracheal tube. We think that through selective intubation, the tension of the anastomosis was adjusted more easily, and we have protected the patient from hypoxia. We did not prefer to use invasive surgical methods such as ECMO, since ventilation can be performed easily from the intraoperative surgical site and anastomosis can be performed rapidly by using endobronchial blockers when suturing is about to be completed.
Besides, one of the most important problems in sleeve resections and tracheal resections is the adjustment of anastomotic tension. Some authors use “interrupted sutures” for easier adjustment of the tension in the anastomosis and to avoid mixing of sutures [6]. On the other hand, Diego et al prefer “continue sutures” in sleeve resections [7]. We often prefer to continue sutures in our tracheal resection surgeries [8]. Thus, the anastomosis is completed not only in a shorter time but also the tension can be adjusted comfortably in the anterior part.
In conclusion, with the improving technological opportunities, major surgical procedures can be easily performed through minimally invasive techniques. We think that tracheal resection with VATS can be safely performed in distal stenosis of the trachea, instead of major incisions such as posterolateral thoracotomy.
Declaration of conflicting interests
The authors declared no conflicts of interest with respect to the authorship and/or publication of this article.
Funding
The authors received no financial support.
Authors’ contributions
SE, CBS, GT, YS,VE, MM: conceived and designed the current case report, co-wrote the paper, collected the clinical data. The authors discussed the case under the literature data together and constituted the final manuscript.
Reference
1) Ujiie H, Yasufuku K. New era of “resection of the carina and lower trachea.” J Thorac Dis 2017; 9: 4932-6.
2) Jiao W, Zhu D, Cheng Z, Zhao Y. Thoracoscopic tracheal resection and reconstruction for adenoid cystic carcinoma. Ann Thorac Surg 2015; 99: e15-7.
3) Jiang L, Liu J, Gonzalez-Rivas D, Shargall Y, Kolb M, Shao W et al. Thoracoscopic surgery for tracheal and carinal resection and reconstruction under spontaneous ventilation. J Thorac Cardiovasc Surg 2018; 155: 2746-54.
4) Ko M, dos Santos PR, Machuca TN, Marseu K, Waddell TK, Keshavjee S et al. Use of single-cannula venous-venous extracorporeal life support in the management of life-threatening airway obstruction. Ann Thorac Surg 2015; 99: e63-5.
5) Hoetzenecker K, Klepetko W, Keshavjee S, Cypel M. Extracorporeal support in airway surgery. J Thorac Dis 2017; 9: 2108.
6) Mahtabifard A, Fuller CB, McKenna Jr RJ. Video-assisted thoracic surgery sleeve lobectomy: a case series. Ann Thorac Surg. 2008; 85: S729-32.






