Summary
Background: The most important treatment method in non-small cell lung cancer (NSCLC) is surgery. Detection of the disease at an early stage is one factor that determines the prognosis. This study investigates the impact of the novel coronavirus disease pandemic on the diagnosis and surgical treatment of NSCLC.Materials and Methods: Between March 2019 and March 2021, a total of 163 patients (142 males, 21 females, mean age 62.3 ± 7.8 years; range, 39 to 78 years) diagnosed with NSCLC who underwent surgery were retrospectively analyzed. The patients were divided into two groups according to COVID-19 pandemic period such as before (Group 1) and after (Group 2) March 2020. Demographic characteristics, symptoms, diagnostic method, pathological diagnosis, stage, surgical treatment method, and developing complications of patients were recorded.
Results: During the investigation of COVID-19, NSCLC was detected among 16.8% (n = 17) of the patients who underwent surgery. The number of NSCLC patients who underwent surgery during the pandemic period increased by 62.9% compared to the pre-pandemic period. (p=0.338). Despite patients with Stage 1 disease (30.6% vs. 9.9%, p = 0.007) and the rate of open surgery was significantly decreased (82.3% vs. 52.5%, p < 0.001) during the pandemic period for patients diagnosed with NSCLC, those who underwent surgery were most frequently determined on stage 1A when compared with the pre-pandemic period. In contrast, the video-assisted thoracoscopic surgery approach increased (17.7% vs. 47.5%, p < 0.001), and a statistically significant difference was found between the distributions of surgical procedures.
Conclusions: In the novel coronavirus pandemic, thorax computed tomography used for lung assessment affected the detection rate of NSCLC. The importance of VATS pulmonary resections increased in this period, thus shortening the hospital stay of the patients.
Introduction
The World Health Organization declared the novel coronavirus disease (COVID-19) a global pandemic on March 11, 2020 [1]. Most non-small cell lung cancers (NSCLC) are diagnosed in the late stages (Stages IIIB-IV) when 5-year survival is low (less than 36%) [2]. Radiologic imaging techniques such as chest X-ray and thorax computed tomography (CT) are not only used for the detection of asymptomatic early-stage lung cancer but also are used as initial screening tests to diagnose COVID-19 disease and helps for early detection of lung cancer. During the pandemic period, there was a decrease in the number of CT applications in the general population [3]. Especially during the periods when the number of COVID-19 cases has peaked, the rate of radiological examinations have increased in patients with respiratory system complaints. Lesions detected in thorax CT imaging in COVID-19 may appear as a ground-glass opacity, which is also highly similar to the lesions detected in lung cancer [4]. The similarities of the detected lesions suggest may affect the diagnosis and surgical treatment of lung cancer in the COVID-19 pandemic.In lung cancer, which has more opportunities to be detected in the pandemic process, new decisions were needed for the treatment plan. Guidelines for surgical treatment of lung cancer recommend to defer 3-month in case of early-stage disease and triage of patients for surgery, taking into account the safety of patients and surgical teams [5]. Despite pandemic, oncological surgeries were continued uninterruptedly by providing isolation and protection measures in our clinic. In this study aimed to evaluate the impact of the COVID-19 pandemic on patients with NSCLC who underwent surgical treatment.
Methods
A total of 163 (142 males, 21 females, mean age 62.3 ± 7.8 years; range, 39-78 years) patients who were diagnosed with NSCLC and underwent surgery between March 2019 and March 2021 were included in our study. The data were analyzed retrospectively.The patients were divided into two groups. Group 1 was patients with NSCLC who were surgically treated during the one year preceding the pandemic period between March 11, 2019, and March 10, 2020. Group 2 patients with NSCLC were surgically treated during the COVID-19 pandemic between March 11, 2020, and March 11, 2021. Sixty-two patients were considered in Group 1 and 101 patients were considered in Group 2. Demographic characteristics, symptoms, diagnostic method, pathological diagnosis, stage, surgical treatment method, and developing complications of patients were recorded separately for Group 1 and Group 2. The patients in the group 2 group were evaluated in detail regarding COVID-19 disease. The cases in which NSCLC was detected during investigation for suspected COVID-19 and delayed due to COVID-19 disease in the preoperative period were also evaluated for the effects of COVID-19 on morbidity and mortality in the postoperative period.
This study was conducted with the approval of the Ministry of Health Scientific Research Platform (No:2021-05-17T13_39_03) and our hospital’s ethics committee (approval number: 2021/277; approval date: May 20, 2021) approval. Informed consent was obtained from all patients.
Statistical Analysis
Collected data were analyzed using SPSS Statistics for Windows, version 23.0 (IBM Corp., Armonk, NY, USA). The suitability of the data to the normal distribution was examined with the Kolmogorov-Smirnov test. Chi-square and Fisher’s Exact tests compared categorical variables according to groups. The Kruskal Wallis test was used to compare quantitative data not normally distributed according to groups of three or more. Mann Whitney U test was used to compare data that did not show normal distribution according to paired groups. Analysis results were presented as mean ± standard deviation and median (minimum-maximum) for quantitative data and frequency (percent) for categorical data. The significance level was taken as p < 0.050.
Results
When the quantitative data were compared according to the groups, no statistical difference was found between the mean age of both groups [62.6 ± 8.1 (42-78) years vs 62.2 ± 7.6 (39-78) years]. No statistically significant difference were detected in terms of tumour size distribution, SUV max values, chest tube pulling time between groups (Table 1). While no statistically significant difference was detected between groups in terms of admission complaints, the rate of NSCLC detected during screening studies increased from 14.5% to 34.7% . In Group 2, the rate of detecting lung lesions on thorax CT during the COVID-19 evaluation was 16.8% (n = 17). Surgery was postponed for 1 month among 6 patients who were infected or exposed with COVID-19. The number of NSCLC patients who underwent surgery during the pandemic period (Group 2) increased by 62.9% compared to the pre-pandemic period. Median length of hospital stay was detected shorter in Group 2 [6(2-48) days vs 5(1-21) days, p = 0.014).Table 1: Comparison of quantitative variables by groups.
The most common diagnostic method for both groups was trans-thoracic tru-cut biopsy (TT-TCB) (53.2% vs 61.4%), and the most common histopathological diagnosis was adenocarcinoma (58.1% vs 52.5%). The rate of invasive mediastinal staging before resection was increased (45.2% vs. 68.3%, p = 0.006). We thought that the probable reason for this increase was intraoperative mediastinal invasive staging (VATS/thoracotomy) (24.2% vs. 46.5%) methods apart from mediastinoscopy (p = 0.006). In the pre-pandemic period, NSCLC patients who underwent surgery (Group 1) most frequently were stage 1A; however, it was determined that the rate of Stage 1 disease decreased significantly (30.6% vs. 9.9%, p = 0.007) during the pandemic period, and the rate of disease detected in Stage 3B increased significantly (1.6% vs. 10.9%, p = 0.007). It was found that a significant difference in the distribution of tumor sizes between the groups. It was determined that T1b size tumors decreased (24.2% vs 7.9%) T1c size tumors increased (14.5% vs 28.7%) (p = 0.042). There was a significant difference between the distribution of tumor positive lymph node stations, and a significant increase in the number of N2 positive patients (3.2% vs. 17.8%, p = 0.028) (Table 2).
Table 2: Comparison of categorical variables by groups.
It was determined that the rate of open surgery decreased (82.3% vs. 52.5%, p < 0.001). Besides that, the video-assisted thoracoscopic surgery (VATS) approach, increased (17.7% vs. 47.5%) and a statistically significant difference was found between the distributions of surgical procedures and applied surgical procedures (p < 0.001) (Table 3).
Table 3: Comparison of surgical variables by groups.
There was no significant difference between the complication rates for both groups. However, 5 patients were passed away during the pandemic period. One patient died on the 1st postoperative day due to acute myocardial infarction. The other 4 patients died in the hospital in the first 30 days due to secondary effects after pneumonia of unknown cause. The length of hospital stay during the pandemic period was shortened. (p = 0.014)
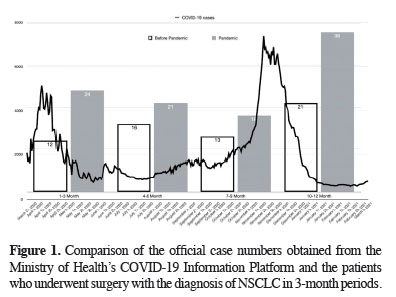
During the pandemic periods when the number of COVID19 cases peaked, the data were analyzed quarterly to compare the number of patients with NSCLC detected with the previous year. When comparing the number of patients with NSCLC who underwent surgery, it was determined that the number of cases increased by 100% in the March-May period, by 31.25% in the June-August period, by 38.46% in the September-November period, and by 80.95% in the December-February period. It was determined that the proportional increases in the first and last periods were correlated with the peak periods of the daily number of cases shared on the Ministry of Health COVID-19 Information Platform (6) (Figure 1). However, this correlation was not statistically significant.
 Click Here to Zoom |
Figure 1: Comparison of the official case numbers obtained from the Ministry of Health’s COVID-19 Information Platform and the patients who underwent surgery with the diagnosis of NSCLC in 3-month periods. |
A statistically significant difference was found between the distribution of the stages among groups in the first 3 months (p = 0.024). Patients with Stage 1A who underwent surgery was significantly reduced (58.3% vs 16.7%, p = 0.024). There was no statistical difference between groups in terms of the distributions of pathology, stage, surgery, and procedure variables in the June-August period. A statistically significant increase was detected in VATS rates in the September-November (23.1% vs. 66.7%, p = 0.005) and December-February (33.3% vs. 63.2%, p < 0.001) periods according to the surgical procedures applied (Table 4).
Discussion
The main findings of this study were when compared with the pre pandemic period, the number of patients who were incidentally diagnosed with lung cancer were increased during COVID-19 screening. In addition, minimally invasive techniques tend to be preferred more. The rates of invasive mediastinal staging were increased, and the rate of surgery performed on stage 1A patients decreased at the beginning of the pandemic and increased the risk of death due to postoperative pneumonia during the pandemic period.While the rate of surgery applied to patients with Stage 1 NSCLC decreased compared to the pre-pandemic period, the rate of surgery applied to Stage 3 patients increased. While symptoms occurring in stage 3 in the pre-pandemic period is not taken into account by patients and are included in advanced stage patient groups who lost the chance for surgery, it is clear that the symptoms that occur during the pandemic period are taken into account due to the risk of COVID-19. Besides, it was shown that the T1b patient group who underwent surgery decreased, and the T factor increased compared to the previous year. At the same time, video thoracoscopic lung resection rates were increased in our clinic by changing surgical procedures according to guidelines published in the pandemic and decreasing the rate of open surgery [7,8]. While the rate of thoracoscopic surgery was 17% before the pandemic, it was increased to 47.5% during the pandemic period. For this reason, it aims to protect the surgical team and health workers and shorten the patients’ hospitalization period.
It is obvious that surgery performed on a more risky patient group in terms of systemic diseases compared to the pre-pandemic period carries a higher risk for COVID-19. Infected with or exposed to COVID-19 were detected in 6% of the patients during the preoperative preparation phase, and to reduce the risks of COVID-19, surgeries were postponed for 1 month.
In the study conducted by Li et al, it was recommended to focus on clinical and pathological findings that require emergency surgery during the pandemic period and perform absolute surgery in resectable lung tumors with significant airway involvement, accompanied by massive hemoptysis and causing severe dyspnea [9]. It was recommended not to apply procedures that allow aerosol propagation, such as bronchoscopy and needle aspiration (EBUS-TBNA) guided by endobronchial ultrasound during the pandemic period [10]. Our findings revealed that the rate of diagnostic bronchoscopy during the pandemic period was 11.9% and without change with the previous period. Nevertheless, TT-TCB was the most frequently used diagnostic method for both groups. Cafarotti et al [11] published an algorithm to determine the urgency classification for patients with lung cancer which was based on TNM staging, the risk of cancer progression and the risks of COVID-19 are considered together. Adenocarcinoma of the lung and squamous cell carcinoma has the potential to progress from early-stage IA to stage IIIB in 1.17 and 2.5 years, respectively [12]. Quebec Lung Cancer Network also shared its recommendations for the surgical treatment of lung cancer during the pandemic [13]. It was emphasized that priority should be given to selected treatments for stage I-III NSCLC. In our study, it was revealed that there was a significant decrease in the T1b patient group who underwent surgery, and surgery was performed on the patients in the T1c patient group, in accordance with the guideline. The fact that the VATS procedure was preferred more as an invasive mediastinal staging method during the pandemic period explains the increase in the number of Stage IIIB patients who underwent surgery.
The high demand for radiological evaluation during the pandemic had a direct impact on patients diagnosed with confirmed or suspected lung cancer [14]. Opinions were advocating that the diagnosis and treatment of lung cancer due to the similarity of ground-glass opacity findings with infiltrates detected in thorax CT in COVID-19 pneumonia, the postponement of cancer screening studies was delayed during the pandemic period [15]. In our study, there was an increase in the number of patients who underwent surgery with the diagnosis of NSCLC. During the pandemic, NSCLC was detected at a rate of 16.8%, with radiological examinations performed with the suspicion of COVID-19. Especially during the peak periods of COVID-19 cases, the number of NSCLC cases that underwent surgery has increased. Compared to the previous year, the number of surgical cases increased by 100% in the Mar-May period and by 80.95% in the Dec-Feb period. In addition, diagnostic procedures such as pulmonary function testing or bronchoscopy, or CT-guided transthoracic biopsy, some preoperative studies were delayed, or certain cases were directly avoided, and this was a strategy that was considered inevitable in line with the measures at the time [16]. It was recommended that patients with nodules with ground-glass opacity (<50% solid component), <2 cm nodules or lung cancer, slow-growing (indolent) histology (carcinoid or slow-growing nodules), and those who may need long-term intensive care should be postponed for 3 months [5]. In accordance with this strategy, according to the T factor in the surgeries performed, it was shown that while the number of patients with T1b tumors decreased in the pandemic period compared to the previous year, there was an increase in the number of patients with T1c tumors. However, when the stages of lung cancer patients who underwent surgery during the pandemic period were compared with the previous year, it was statistically revealed that surgery applied to stage 1A patients was reduced. To keep the surgical time short, especially intraoperative (thoracotomy/VATS), the invasive staging was performed in accordance with the criteria for mediastinal invasive staging [17]. Therefore, it was observed that there was a significant increase in the rate of positive tumor detection in the ipsilateral lymph nodes during the pandemic period in our study.
Since lung surgery is the surgery with the highest aerosol formation, it had a special place in terms of surgical procedures to be applied in the COVID-19 pandemic [7]. Even if all personal protective measures and necessary operating room conditions are provided, it increases the risk of smog, aerosol formation, and spread of infection, especially due to the effect of the energy devices used. Therefore, in all surgical branches, it has been suggested that minimally invasive surgical procedures should be preferred in cases where surgery is unavoidable [18]. Vigneswaran et al argued that aerosolized virus could not cause active infection through the skin [19]. However, we preferred to perform surgical procedures in our clinic in accordance with the guidelines since the situation in question is absorption from the mucous membranes and spread by inhalation. Therefore, it was shown that VATS, which was applied at a rate of 17.7% in the pre-pandemic period, increased to 47.5% during the pandemic period, and this rate was a statistically significant increase. It was determined that the length of hospital stay decreased significantly, especially in correlation with the increasing minimally invasive surgical practice. Notwithstanding, there was no significant difference in surgical complications. Nevertheless, while no mortality was observed in patients who underwent surgery in the pre-pandemic period, mortality occurred in 5 patients during the pandemic period. One patient died on the 1st postoperative day due to acute myocardial infarction. Although the COVID-19 PCR test is negative, in the other 4 patients, COVID-19 pneumonia could not be excluded in computed tomography images. During the pandemic period, the length of hospital stay was statistically significantly shortened. Villena-Vargas et al similarly stated that the duration of hospital stay was shortened during the pandemic period, and this may affect the risk of hospital infection [20].
Our study has some limitations such as it was a single-center retrospective study. Because no surgically applicable lung cancer patient is delayed or referred to non-surgical methods, the effects of the COVID-19 pandemic on the non-surgical NSCLC patient group could not be evaluated. Besides, in the first period of the pandemic, the preoperative COVID-19 exclusion procedures and the difficulties in controlling the postoperative COVID-19 transmission risks directly affected the results.
In conclusion, the novel coronavirus disease, which affected people in all areas of life in the early stages of the pandemic in our country, directly affected the increase in the detection of patients with NSCLC. The importance of VATS pulmonary resections increased in this period, thus shortening the hospital stay of the patients. It is also thought that up-to-date guidelines can be created with studies to evaluate the effects of COVID-19 vaccine applications on the treatment processes of patients with NSCLC in the future.
Declaration of conflicting interests
The authors declared no conflicts of interest with respect to the authorship and/or publication of this article.
Funding
The authors received no financial support for the research and/or authorship of this article.
Ethics approval>br> This study was conducted with the approval of the Ministry of Health Scientific Research Platform (No: 2021-05-17T13_39_03) and Ondokuz Mayis University Faculty of Medicine ethics committee (approval number: 2021/277; approval date: May 20, 2021).
Authors’ contribution
SG: conceptualization, methodology, project administration, writing-original draft, writing-review and editing, visualization, validation, ATS: data curation, formal analysis, investigation, software, writing-review and editing, supervision, validation, MGP: data curation, investigation, formal analysis, YB: data curation, investigation, formal analysis, BC: supervision, validation and writing-review and editing, NGT: data curation and investigation, CI: data curation and investigation, AB: supervision, validation and writing-review and editing. All authors actively contributed to discussion of the results from the study and reviewed and approved the final version to be released.
Reference
1) Organization WH. Coronavirus (COVID-19) events as they happen. April 6, 2020. [Available from: https://www.who.int/ emergencies/diseases/novel-coronavirus-2019/events-as- they-happen.
2) Goldstraw P, Chansky K, Crowley J, Rami-Porta R, Asamura H, Eberhardt WEE et al. The IASLC Lung Cancer Staging Project: Proposals for Revision of the TNM Stage Groupings in the Forthcoming (Eighth) Edition of the TNM Classification for Lung Cancer. J Thorac Oncol 2016; 11: 39-51.
3) Agarwal M, Udare A, Patlas M, Ramonas M, Alaref AA, Rozenberg R et al. Effect of COVID-19 on computed tomography usage and critical test results in the emergency department: an observational study. CMAJ Open 2020; 8: E568-E76.
4) Bayramoglu Z, Canipek E, Comert RG, Gasimli N, Kaba O, Sari Yanartas M et al. Imaging Features of Pediatric COVID-19 on Chest Radiography and Chest CT: A Retrospective, Single-Center Study. Acad Radiol 2021; 28: 18-27.
5) Thoracic Surgery Outcomes Research Network I, Antonoff M, Backhus L, Boffa DJ, Broderick SR, Brown LM et al. COVID-19 Guidance for Triage of Operations for Thoracic Malignancies: A Consensus Statement From Thoracic Surgery Outcomes Research Network. Ann Thorac Surg 2020; 110: 692-6.
6) T.C.Saglik Bakanligi, COVID-19 Bilgilendirme Platformu 2021 [Available from: https://covid19.saglik.gov.tr/.
7) Jheon S, Ahmed AD, Fang VW, Jung W, Khan AZ, Lee JM et al. Thoracic cancer surgery during the COVID-19 pandemic: a consensus statement from the Thoracic Domain of the Asian Society for Cardiovascular and Thoracic Surgery. Asian Cardiovasc Thorac Ann 2020; 28: 322-9.
8) Berzenji L, Vercauteren L, Yogeswaran SK, Lauwers P, Hendriks JMH, Van Schil PE. Safety and Feasibility of Lung Cancer Surgery under the COVID-19 Circumstance. Cancers (Basel) 2022; 14: 1334.
9) Li X, Liu M, Zhao Q, Liu R, Zhang H, Dong M et al. Preliminary recommendations for lung surgery during COVID-19 epidemic period. Thorac Cancer 2020; 11: 1372-4.
10) Hilzenrat RA, Deen SA, Yee J, Grant KA, Ashrafi AS, Coughlin S et al. Thoracic Surgeon Impressions of the Impact of the COVID-19 Pandemic on Lung Cancer Care-Lessons from the First Wave in Canada. Curr Oncol 2021; 28: 940-9.
11) Cafarotti S, Patella M. Lung Cancer Surgical Management During the Outbreak of Coronavirus Disease 2019. J Thorac Oncol 2020; 15: e81.
12) Yuan P, Cao JL, Rustam A, Zhang C, Yuan XS, Bao FC et al. Time-to-Progression of NSCLC from Early to Advanced Stages: An Analysis of data from SEER Registry and a Single Institute. Sci Rep 2016; 6: 28477.
13) Blais N, Bouchard M, Chinas M, Lizotte H, Morneau M, Spicer J et al. Consensus statement: summary of the Quebec Lung Cancer Network recommendations for prioritizing patients with thoracic cancers in the context of the COVID-19 pandemic. Curr Oncol 2020; 27: e313-e7.
14) Van Haren RM, Delman AM, Turner KM, Waits B, Hemingway M, Shah SA et al. Impact of the COVID-19 Pandemic on Lung Cancer Screening Program and Subsequent Lung Cancer. J Am Coll Surg 2021; 232: 600-5.
15) Li Y, Wang X, Wang W. The Impact of COVID-19 on Cancer. Infect Drug Resist. 2021; 14: 3809-16.
16) Martinez-Hernandez NJ, Caballero Silva U, Cabanero Sanchez A, Campo-Canaveral de la Cruz JL, Obeso Carillo A, Jarabo Sarceda JR, et al. Effect of COVID-19 on Thoracic Oncology Surgery in Spain: A Spanish Thoracic Surgery Society (SECT) Survey. Cancers (Basel) 2021; 13: 2897.
17) De Leyn P, Dooms C, Kuzdzal J, Lardinois D, Passlick B, Rami-Porta R et al. Revised ESTS guidelines for preoperative mediastinal lymph node staging for non-small-cell lung cancer. Eur J Cardiothorac Surg 2014; 45: 787-98.
18) Moletta L, Pierobon ES, Capovilla G, Costantini M, Salvador R, Merigliano S et al. International guidelines and recommendations for surgery during Covid-19 pandemic: A Systematic Review. Int J Surg 2020; 79: 180-8.






