2Department of Thoracic Surgery, Faculty of Medicine, Marmara University, İstanbul, Turkey DOI : 10.26663/cts.2017.0014
Summary
Postpneumonectomy syndrome is a rare condition caused by rotational displacement of mediastinum over time after pneumonectomy. Usually, dynamic airway obstruction is the predominant symptom. We report the case of a 40-year-old lady who underwent left pneumonectomy due to mucoepidermoid carcinoma 3 years ago and presented to our department with recalcitrant gastroesophageal reflux symptoms such as heartburn and odynophagia. She also had objective reflux findings in pH monitorization. Laparoscopic Toupet fundoplication was performed and resulted in symptomatic relief.Introduction
Postpneumonectomy syndrome (PPS) is a rare condition caused by extreme rotational displacement of mediastinal structures towards the pneumonectomy cavity, stretching the tracheobronchial tree and esophagus. PPS incidence varies greatly between different case series, within the range of 0.01-2% [1] and most of the authors report predominantly central airway obstruction symptoms as a chief complaint [1,2]. Dysphagia and gastroesophageal reflux symptoms are reported to a lesser extent [2]. Time to occurrence of symptoms after pneumonectomy also varies on case basis and can be as early as 6 months but usually presentation is delayed until 4-5 years after initial surgery [2].PPS is usually treated mechanically with tissue expanders or fixed volume prosthesis inserted in the pneumonectomy cavity either by re thoracotomy [2] or minimally invasive surgery [3], repositioning the mediastinum. This approach has proven to be successful in terms of restoring the respiratory and effort capacity of the patients in both subjective (quality of life) and objective (pulmonary function and exercise capacity tests) terms, but may result in significant need for reoperation, morbidity and mortality as well [2]. The overall effect of this kind of surgical correction on gastrointestinal symptoms is unclear.
In this article we present a patient with gastroesophageal reflux disease (GERD) due to post pneumonectomy syndrome, undergoing laparoscopic anti reflux surgery.
Case Presentation
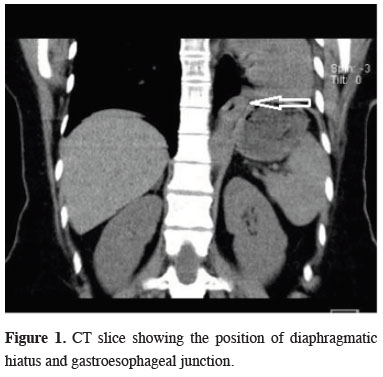
Our patient was a 40-year-old lady who underwent left pneumonectomy 3 years ago due to mucoepidermoid carcinoma of the left main bronchus. Her oncologic follow up showed no signs of recurrence and she was referred to our clinic due to progressive odynophagia and heartburn of one year, both unresponsive to optimal medical management. She reported no respiratory symptoms. She wasn"t receiving any medication such as bronchodilators and she was able to lead a normal life otherwise. Transthoracic ECHO was normal as well. Her FEV1 (1.7 L) and FVC (2.5 L) were within normal ranges.CT scan showed compensatory hyperinflation of the right lung and all mediastinal structures were rotated clockwise to the left hemithorax. Esophagus was stretched and showed crossing over to the left side, exiting the thorax through a larger diaphragmatic hiatus which was caused due to asymmetrical elevation of the diaphragm (Figure 1).
 Click Here to Zoom |
Figure 1: CT slice showing the position of diaphragmatic hiatus and gastroesophageal junction. |
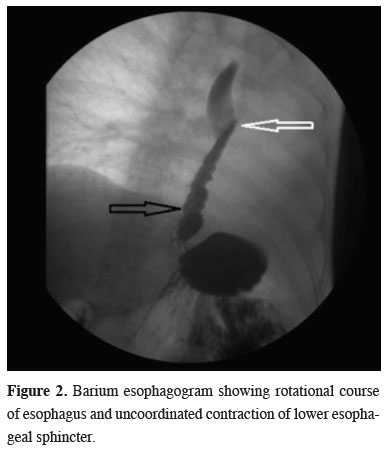
Barium esophagogram showed a normal caliber esophagus with unobstructed passage to stomach, rotational course of the esophagus (Figure 2, white arrow) and uncoordinated contraction of distal esophagus (black arrow) and a small sliding hiatal hernia. pH monitorization and high resolution manometry were concordant with GERD, showing a De Meester score of 70, lower esophageal sphincter (LES) pressure of 28 mmHg and LES length of 2.6 cm. Upper GI endoscopy also confirmed a Hill Class 2 hiatal hernia on retroflexion.
 Click Here to Zoom |
Figure 2: Barium esophagogram showing rotational course of esophagus and uncoordinated contraction of lower esophageal sphincter. |
Since the patient had an objective and severe gastroesophageal reflux, we decided to perform a laparoscopic antireflux procedure. Intraoperatively she was found to have a large hiatus, 3 cm hiatal hernia, a smaller and elevated left diaphragm (possibly causing traction to hiatus resulting in enlargement) and severe adhesions between the esophagus and posterior hiatus. Working ports were inserted accordingly, more to the left and superior than normal, adjusting to the patient"s anatomy. Dissection was carried forward towards posterior mediastinum, aorta was seen at the right side of the esophagus. With the help of the posterior mediastinal dissection, an additional 3-5 cm of esophageal length was gained and gastroesophageal junction was restored to its intraabdominal position easily. Diaphragmatic hiatus was repaired posteriorly with two separate 0 silk sutures, a posterior 270-degree fundoplication was also done with two 2-0 silk sutures on both sides. Intraoperatively we didn"t use either mesh or a gastroplasty procedure as repair was possible without any tissue tension.
The patient was able to tolerate clear liquids on postoperative day 1, progressed to soft foods on day 2, and was discharged on day 3 without any complications. She was maintained on soft food diet for 2 weeks, gradually introducing solids thereafter. She remains symptom free in terms of GERD at her 1 year follow up visit and is able to consume a normal diet.
Discussion
Post pneumonectomy syndrome is a rare and possibly under reported entity in thoracic surgery clinics. We have no way of prediction for this syndrome and attempts of preventing this natural space obliteration process have largely been abandoned [4]. We do know that together with displacement of mediastinal structures, hyperinflation of the contralateral lung becomes possible and is beneficial in terms of pulmonary function tests and quality of life in long term follow up of pneumonectomy patients [5]. The mechanism of GERD in our patient appeared to be mainly due to severe elevation of the diaphragm and thus secondary enlargement of esophageal hiatus due to superior traction of left crus. A second pathology secondary to her postpneumonectomy displacement was significant rotation of the esophagus in mid chest (Figure 2), but this was not the cause of her GERD symptoms. Thus our decision to perform an antireflux procedure instead of mediastinal repositioning with tissue expanders was based on the assumptions that antireflux surgery alone has less potential morbidity compared with the alternative. Tissue expanders would cause a net decrease in the lung volume without an underlying dynamic airway compression to correct, possibly undermining the patient"s effort capacity. Short term follow up of the patient was encouraging about the correctness of our approach.
Declaration of conflicting interests
The author declared no conflicts of interest with respect to the authorship and/or publication of this article.
Funding
The author received no financial support.
Reference
1) Soll C, Hahnloser D, Frauenfelder T, Russi EW, Weder W, Kestenholz PB. The postpneumonectomy syndrome: clinical presentation and treatment. Eur J Cardiothorac Surg 2009; 35: 319-24.
2) Shen KR, Wain JC, Wright CD, Grillo HC, Mathisen DJ. Postpneumonectomy syndrome: surgical management and long-term results. J Thorac Cardiovasc Surg 2008; 135: 1210-6; discussion 1216-9.
3) Avgerinos DV, Meisner J, Harris L. Minimally invasive repair of post-pneumonectomy syndrome. Thorac Cardiovasc Surg 2009; 57: 60-2.






