Summary
Background: This study aimed to evaluate the perspectives of residents working in thoracic surgery clinics at university, training, and research hospitals in Turkey, regarding their educational experiences, as well as their knowledge, attitudes, and expectations about the theoretical and practical aspects of practice.Materials and Methods: A total of 180 residents from thoracic surgery clinics in randomly selected university, training, and research hospitals in Turkey were contacted. A 37- question survey was designed using tr.surveymonkey.com and distributed via social media (WhatsApp). Of these, 160 residents participated, and the results were analyzed.
Results: Among the 160 respondents, 94 (58.8%) were male and 66 (41.2%) were female, with a mean age of 29.4 ± 2.9 years (range 25-39). In the medical specialty examination, 137 (85.63%) of the participants ranked thoracic surgery in the 1st to 5th positions. Clinics had a mean of 9 ± 5 residents (range 1-22). 37 (23.1%) reported 8 or more shifts per month, and 31 (19.4%) had no time off after shifts. Approximately 52% of clinics offered an average of 5 ± 2.5 hours of training per month. A total of 109 (68.1%) residents were able to perform cases as the primary surgeon. The main learning sources were mainly senior assistants (41.9%) and faculty members (31.2%). ‘Mobbing’ was reported by 26 (16.2%), and 88 (55%) expressed future career uncertainty. After training, 43.1% planned to work as specialists, and 32.5% aimed for academic careers.
Conclusion: The study offers insights to enhance thoracic surgery training programs, support residents, and improve professional satisfaction. These findings may guide future strategies and policies to foster a better educational environment in thoracic surgery.
Introduction
In our country, medical specialty education and its challenges are frequently discussed due to the unfortunate events that have occurred and require legal reforms. In recent years, the increase in the number and diversity of patients, particularly in tertiary healthcare institutions where education is provided, along with advancements in medicine, has led to a rise in the number and complexity of interventions. The combination of specialized education, healthcare delivery, working hours, shift frequency, job security, and working conditions adds to the difficulties faced by residents during their training period. Although these issues are common across all specialties, the long training periods make them more severe and challenging, especially for residents in surgical fields where they encounter more complex and difficult cases and diseases [1].Medical Specialization Board Curriculum Formation and Standard Setting System (TUKMOS) in Turkey is responsible for reviewing, developing, and formalizing previously established core curricula across all major and subspecialty fields. In this context, the core curriculum for thoracic surgery was finalized on 05.05.2016. In this program, thoracic surgery is defined as a surgical field that deals with lung, mediastinum, diaphragm, esophagus, trachea, pleura, chest wall, and trauma in both adult and pediatric populations [2].
According to TUKMOS, the goal is for a specialist who has completed their education to be capable of independently diagnose diseases related to thoracic surgery, performing medical and surgical treatments, providing postoperative care, and managing potential complications. As per this program, the total training duration for thoracic surgery specialization is 5 years, including 1 year dedicated to rotations. The rotations consist of 6 months in general surgery, 3 months in cardiovascular surgery, 2 months in thoracic diseases, and 1 month in anesthesiology and reanimation clinics [2].
The problems frequently encountered in thoracic surgery education include a lack or insufficiency of theoretical and/or practical education, differences in patient diversity across clinics, mobbing, the inability to take leave after shifts, and the inability to actively participate in rotations. This study was designed to substantiate these and similar issues, highlight challenges faced by residents in other clinical disciplines, and propose solutions.
In this survey, the issues faced by thoracic surgery residents during their training will be explored, and concerns related to their profession will be identified. Based on the results of this survey, solutions will be developed for the identified problems, and the findings will be communicated to relevant authorities through the Thoracic Surgery Association to guide legal reforms.
Methods
Approval for this cross-sectional study was obtained from the University Clinical Research Ethics Committee, with the reference number B.30.2.ODM.0.20.08/629-92. The study population consisted of thoracic surgery residents at the time of the study. No sample was selected; instead, an attempt was made to reach the entire population. As of November 20, 2023, the Republic of Turkey Ministry of Health reported that there were 322 thoracic surgery residents in Turkey. In the study, 180 thoracic surgery residents working in randomly selected university, training, and research hospitals were contacted. A total of 160 thoracic surgery residents completed the questionnaire.The data collection process was carried out using a questionnaire form, which was created by the researchers after a comprehensive review of the literature. It was made available online via the ‘en.surveymonkey.com’ website. To ensure the questionnaire was answered objectively, sincerely, realistically in line with its purpose, respondents were informed about the nature, aims, and reasons of the research in the introduction section of the questionnaire and their consent was obtained.
The questionnaire, consisting of a total of 37 multiple- choice questions, included 8 questions on sociodemographic data, 4 questions about the medical specialty examination and the thoracic surgery specialty, and 25 questions addressing participants' working conditions, the facilities and status of their training clinics, theoretical and practical training, rotations, and their thoughts on thoracic surgery specialization.
Inclusion criteria is; being a resident in thoracic surgery clinics, working in a university, training and research hospital, agreeing to participate in the survey. The exclusion criteria is; being a resident in a clinic other than thoracic surgery, having completed thoracic surgery specialty training and refusal to participate in the survey.
Statistical Analysis
The survey results were evaluated using the data obtained
from en.surveymonkey.com. Descriptive statistics were presented
as numbers, percentages, means ± standard deviations.
Results
Of the 160 thoracic surgery residents who participated in the survey, 94 (58.8%) were male, 66 (41.2%) were female, and the mean age was 29.4 ± 2.9 (range: 25-39) years. The demographic data of the participants are summarized in Table 1.Table 1. The social demographic features of participants.
The mean TUS score of the participants was 51.5 ± 4.7 (range: 45-68). When asked why they preferred the thoracic surgery specialty, the responses were as follows: 53% (n = 80) chose it because they wanted to pursue a surgical specialty, 45% (n = 72) were specifically interested in thoracic surgery, and 2% (n = 3) chose it because it was a specialty accessible with a lower TUS score. The answers given to the questions about the TUS process are presented in Table 2.
While 60% (n = 96) of the participants were working in a university hospital, 40% (n = 64) were working in a training and research hospital. The average number of patient beds in their clinics was 21 ± 11 beds, with the smallest ward having 5 beds and the largest ward having 60 beds. Additionally, 54% (n = 86) of the clinics had their own intensive care unit.
The distribution of the number of years completed by thoracic surgery residents who participated in the survey is shown in Figure 1.
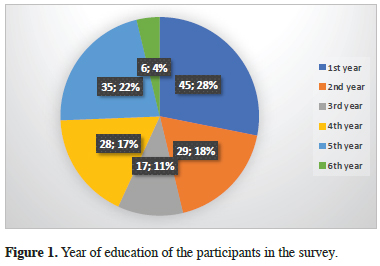 Click Here to Zoom |
Figure 1: Year of education of the participants in the survey. |
On average, thoracic surgery clinics had 9 ± 5 (range: 1-22) residents. The number of residents working shifts varied: 1-3 shifts per month was 30 (18.8%), 4-7 shifts per month was 93 (58.1%), 8-11 shifts per month was 33 (20.6%), and more than 11 shifts per month was 4 (2.5%).
Additionally, 108 (67.5%) of the residents worked shifts alone, while 52 (32.5%) residents worked shifts in pairs. About 80.6% (n = 129) of the participants stated they could take leave after shifts, whereas 19.4% (n = 31) could not.
Approximately 52% of thoracic surgery clinics had an average training program of 5 ± 2.5 (range:1-12) hours per month. Regarding theoretical education, 44% of clinics provided 4.6 ± 2.2 (range:1-10) hours per month. Additionally, weekly scientific and/or case discussion meetings (average 4.2 ± 1.9 hours per month) were held in approximately 70% of the clinics.
When the participants were asked, "Are residents allowed to perform cases as the primary surgeon in your clinic?", 109 (68.1%) responded that they could perform cases independently under the supervision of medical staff. The average time required to perform a case as the primary surgeon under the supervision of a faculty member was 2.7 ± 1.3 years of specialty training.
The response to the question, "From whom or where do you acquire the most theoretical and/or practical knowledge?", is presented in Figure 2.
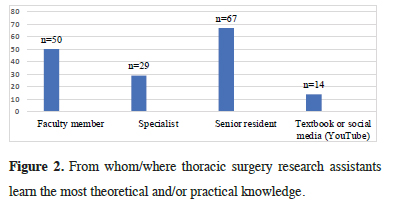 Click Here to Zoom |
Figure 2: From whom/where thoracic surgery research assistants learn the most theoretical and/or practical knowledge. |
When asked, "Which method is primarily used for surgical approaches in your clinic?", the responses were as follows: 94.4% (n = 151) for video-assisted thoracic surgery (VATS), 78.8% (n = 126) for thoracotomy, and 6.9% (n = 11) for robotic-assisted thoracic surgery (RATS).
Eighty-five percent (n = 136) of the participants expressed a preference for rotations between clinics that perform specialized procedures, such as esophageal surgery and endobronchial ultrasonography (EBUS).
When asked about the impact of the COVID-19 pandemic on specialty education, 45% (n = 72) stated that it had a negative impact, 22.5% (n = 36) reported a partially negative impact, and 32.5% (n = 52) indicated that it did not affect their specialty education. Approximately 54% (n = 86) of the participants worked as residents during the COVID-19 pandemic period.
Regarding the adequacy of the 5-year training period in thoracic surgery, 88.7% (n = 142) considered it adequate, 8.8% (n = 14) found it partially adequate, and 2.5% (n = 4) deemed it insufficient.
One of the questions in the questionnaire asked, "Do you have any concerns about your future in the profession?" While 55% (n = 88) of the participants expressed significant concerns, 22.5% (n = 36) reported partial concerns, and 22.5% (n = 36) stated that they had no concerns regarding their professional future.
When the diversity of post-specialty plans was assessed, 43.1% (n = 69) of the participants planned to continue as specialists after completing their specialty training, while 32.5% (n = 52) intended to pursue an academic career. Additionally, 18.1% (n = 29) planned to practice abroad, and 6.3% (n = 10) indicated that they did not intend to specialize further in thoracic surgery after completing their training.
Among the participants, 49% (n = 79) stated that they had attended a scientific congress, and 71% of whom did so with scholarships provided by the association, 19% with support from a corporate sponsor, and 10% through their own financial means.
While 23.7% (n = 38) of the participants reported being informed about the rotation learning objectives set by the medical specialty board, 21.9% (n = 35 indicated being partially informed, and 54.4% (n = 87) stated that they had no knowledge of these learning objectives.
When the effectiveness of the mandatory rotations during the training period was evaluated, 67% (n = 107) of the participants stated that the rotations were inefficient and ineffective. Among the participants who rotated in other clinics during the training period, 13.1% reported being actively involved in the clinics they attended, 33.8% reported being partially active, and 53.1% stated that they did not take an active role in the clinics during their rotations.
Furthermore, 66.9% of the participants expressed that the education they received in the departments they rotated through did not meet their expectations. The responses provided regarding experiences of ‘mobbing’ are presented in Table 3.
Table 3. Experiences of mobbing among thoracic surgery residents.
Discussion
Thoracic surgery education began with the establishment of the first thoracic residency program at the University of Michigan in 1928 [3]. In Turkey, TUKMOS plays an active role in reviewing, developing and formalizing the previously prepared core curricula in all major and subspecialty areas. Within this framework, thoracic surgery is defined as a surgical branch that encompasses the lung, mediastinum, diaphragm, esophagus, trachea, pleura, chest wall and traumas affecting both the adult and pediatric populations [2].In Turkey, physicians who earn the title of medical doctor after six years of medical education must take the TUS exam and pass it to specialize. In a study conducted by Akçam et al, thoracic surgery was ranked as the 4th and 1st choice in the TUS preferences, respectively. Furthermore, the reasons for choosing thoracic surgery were reported as interest in the specialty, a desire to perform surgery, and a pursuit of an academic career, respectively [4]. In our study, residents who ranked thoracic surgery between 1st and 5th in their preferences constituted 85.63% of the participants, and 73% indicated that they would choose thoracic surgery again if they had to take the TUS exam again. Regarding the reasons for their preference, half of the participants stated that they chose it because they wanted a surgical specialty, and 45% indicated that they chose it due to their interest in thoracic surgery.
In recent years, there has been a steady increase in the number of women in the medical profession. According to the Association of American Medical Colleges, 49.8% of medical school graduates in 2016 were women [5]. In a study of 23423 physicians conducted by Yılmaz et al in 2021, 41.5% of physicians were female, and 27% of those working in surgical medicine were reported to be female. Notably, 33% of those working in thoracic surgery were female [6]. In our study, 41% of the participants were female, which contrasts with the literature, despite thoracic surgery being a surgical discipline. This finding suggests that the interest of the female gender in surgical specialties has increased over the years.
It has been reported in many studies that excessive working hours and high number of shifts in the medical field are significant risk factors for burnout [7,8]. Residents also reported long working hours and heavy workloads as unfavorable working conditions [9,10]. In a study by Çelik et al, the prevalence of burnout syndrome among thoracic surgeons was found to be 40- 50%, a rate similar to that observed across all surgical branches [11]. In our study, 23.1% of the participants reported having eight or more shifts per month, and 67.5% of them were on duty alone during these shifts.
Although it is a legal obligation to take leave after a shift, 19.4% of the participants stated that they were unable to take this leave. We believe that this issue stems from the insufficient number of residents in the clinics and/or an excessive workload.
In a report by the International Labor Organization, it is highlighted that workplace violence, intimidation (mobbing) and burnout have become increasingly prevalent issues on a global scale [12]. Similarly, Xaplanteri et al found that mobbing levels significantly varied significantly across sectors, with the highest scores recorded in the surgical sector and the lowest in the laboratory sector. They attributed this disparity to the intense workload, high-stress environment, and strict hierarchical culture of surgical departments, which were observed to increase interpersonal conflicts and create a conducive environment for mobbing behaviors [13]. Consistent with these findings, our study revealed that 35.6% of participants experienced mobbing in their workplace, with 71.7% of them perceiving the mobbing as being directed specifically at them.
For effective residency training, at least 20 hours per week should be dedicated to education [14]. However, studies conducted throughout Turkey reported that only 2.5% of residents prioritized education, theoretical education was considered non-essential in one out of three specialty training institutions and mortality/morbidity meetings were held in only one out of four institutions [15,16]. In our study, 52% of the clinics had an educational program comprising an average of 5 ± 2.5 hours per month, theoretical education was provided in 42% of the clinics, and scientific meetings were organized in 70% of the clinics. Regarding practical training, 68.1% of the residents were allowed to perform cases as the primary surgeon.
Education in medicine is directly related to seniority and the experiences gained through seniority at every stage. Most theoretical and practical training is received from senior physicians. In the study by Akçam et al, 55.7% of the participants stated that their primary source of information was senior residents, while 32.6% reported classical books as their main source of information [4]. Similarly, in our study, 41.8% of the participants stated that their primary source of information was the senior resident, while 31.25% identified faculty members. Approximately 9% of the participants reported using textbooks or social media as their usual source of information.
In recent years, with the development of VATS and RATS in our country, the decline in thoracotomy approaches is thought to negatively impact resident training in open surgery [17,18]. However, when the preferred clinical surgical approach was examined in our study, 151 residents reported using VATS, while 126 residents reported using thoracotomy. We believe this reflects the diversity of cases encountered in our country, where, unfortunately, a significant proportion of patients present at locally advanced stages. Additionally, the high incidence of tuberculosis in our country leads to the presence of advanced intrathoracic adhesions, which is one of the most important factors limiting the use of VATS. However, despite its challenges, this situation increases the number and variety of cases observed and/or performed by thoracic surgery residents during specialty training. Moreover, the experience gained from open and complex operations provides a strong foundation for VATS and RATS training, thereby potentially shortening the training period and improving proficiency in minimally invasive techniques.
Another problem is that some clinics perform specialized surgical interventions (EBUS, esophageal surgery), which creates a significant disparity in training opportunities among clinics. In our study, 85% of the participating residents expressed a desire to address this disparity through rotations among clinics. To achieve this, residents and lecturers in our clinic frequently participate in national and international rotations and training programs.
The COVID-19 pandemic has negatively impacted medical education at all levels in our country as well as globally. These disruptions have particularly affected the education of residents in surgical specialties, including thoracic surgery [19]. In our study, 45% of the participants reported that their specialty education was severely affected by the pandemic, while 22.5% indicated that it was partially affected. Considering that 36% of the participants were 1st and 2nd-year residents, it can be inferred that nearly all residents whose training overlapped with the pandemic were significantly impacted. Similarly, Daniel et al emphasized that the pandemic posed unprecedented challenges to education systems worldwide, compelling institutions to rapidly transition from face-to-face education to remote learning with limited preparation time. This abrupt shift disrupted traditional teaching methods and exacerbated existing inequalities in access to educational resources, especially in technologically underprivileged settings [20]. The findings of our study align with these observations, underscoring the profound impact of the pandemic on surgical education, which heavily depends on hands-on training and face-to-face mentorship.
Akçam et al reported that 67.3% of thoracic surgery residents found the five-year training period sufficient [4]. In our study, 97.5% of thoracic surgery residents found the five-year training period sufficient. However, only 23.7% of the participants in our survey stated that they were fully informed about the rotation learning objectives set by the medical specialty board. In the study conducted by Çıtak et al in 2012, participants were asked which rotations they had actively performed or planned to perform. 44.8% of the participants answered general surgery, 26.9% cardiovascular surgery, 22.4% chest diseases, 13.4% anesthesiology and reanimation, 16.4% selected all of them, and 37.3% indicated none of them. In contrast, only 33% of the participants in our study stated that they had completed the required clinical rotations. Despite the passage of time, no significant improvement has been achieved in fulfilling the rotation learning objectives, and the rotations that did take place were not aligned with these objectives.
According to the Turkish Medical Association, more than 1400 physicians migrated abroad in 2021, and the total number of physicians migrating abroad in the past decade has reached 4000 [21]. Furthermore, a study on medical students in Turkey, 94% of the students were considering practicing medicine abroad [22]. In our study, 55% of thoracic surgery residents expressed concerns about their future profession, and we found that 43.1% of the participants planned to work as thoracic surgery specialist, 32.5% aimed to pursue an academic career, and 18.1% intended to practice abroad once their specialty training was completed.
In our study, significant findings were obtained by comprehensively examining the training processes, professional satisfaction, and challenges faced by thoracic surgery residents. The increase in the number of female surgeons’ highlights progress in gender diversity within the surgical, indicating that interest in thoracic surgery is growing, which suggests that this trend will likely continue in the future. Issues such as burnout, mobbing, and disruptions in education caused by long working hours and high workload have a negative impact on professional development and satisfaction. Considering the adverse effects of the COVID-19 pandemic on education, it is crucial to focus on how training processes can be improved during such crises.
The importance of interactions with senior residents and instructors as a significant source of knowledge underscores the need to enhance their roles and effectiveness in education. Additionally, the fact that the majority of residents are satisfied with their choice of the thoracic surgery specialty and would choose the same specialty again if they retook the TUS highlights the specialty's appeal and the effectiveness of the training. However, professional concerns and plans to work abroad provide important feedback on medical education and the healthcare system in Turkey.
One of the limitations of our study is the difficulty in reaching thoracic surgery residents, which may have affected the representativeness of our sample. Additionally, the lack of a dedicated communication network for thoracic surgery residents further contributed to the challenges in data collection. These, which we were able to address, might have influenced the scope and depth of the insights we gathered regarding the residency program and its associated issues.
In conclusion, our study offers valuable insights for improving thoracic surgery training programs, supporting residents in all aspects, and increasing their professional satisfaction. These findings can contribute to the development of future educational strategies and policies, helping to create a more effective and sustainable educational environment in the field of thoracic surgery.
Declaration of conflicting interests
The authors declared no conflicts of interest with respect
to the authorship and/or publication of this article.
Funding
The authors received no financial support for the research
and/or authorship of this article.
Ethics approval
This cross-sectional study was approved by the Ondokuz
Mayıs University Clinical Research Ethics Committee,
with the reference number B.30.2.ODM.0.20.08/629-92.
Authors' contributions
Cİ: Conceptualization of the research idea, study design,
data collection, analysis, and manuscript preparation,
MGP: study design, survey preparation, statistical analyses,
and manuscript review, BÇ: literature review, data
collection, survey preparation, and evaluation of study
findings, YBB: evaluation of study data, language and
content editing, and final proofreading of the manuscript.
Acknowledgement
We would like to express our deepest gratitude to all thoracic
surgery residents who participated in this study for
their valuable time and insights. Additionally, we extend
our sincere thanks to the Turkish Society of Thoracic Surgery
for their support and guidance throughout the research
process. We acknowledge Yavuz Karaca for their
invaluable assistance in translating this manuscript.
Reference
1) Guo C, Liu L, Zhang J, Zhao K, Li S. Revolutionizing thoracic
surgery education: a bibliometric analysis of the past decade’s
literature. J Cardiothorac Surg 2024; 19: 428.
2) TUKMOS. Göğüs Cerrahisi Uzmanlık Eğitimi Çekirdek
Müfredatı: Tıpta Uzmanlık Kurulu; 2016 [updated 05.05.2016;
cited 2024 Jul 1]. Available from: https://dosyamerkez.saglik.
gov.tr/Eklenti/14481/0/goguscerrahisimufredatv21pdf.pdf.
3) Crawford FA Jr. Thoracic surgery education: past, present, and
future. Ann Thorac Surg 2005; 79: S2232-S7.
4) Akçam Tİ, Çağırıcı U, Çakan A, Turhan K, Özdil A. Göğüs cerrahisi
asistanları cerrahi eğitimleri konusunda ne düşünüyor?
Turk Thorac Cardiovasc Surg J 2012; 20: 107-10.
5) Association of American Medical Colleges. FACTS: applicants,
matriculants, enrollment, graduates, MD-PhD, and residency
applicants data. 2018.
6) Yılmaz N, Alkan A, Ertümer AG, Kuh Z. Tıpta uzmanlık
alanlarının toplumsal cinsiyet açısından değerlendirilmesi. Cukurova
Med J 2021; 46: 1257-66.
7) Ozyurt A, Hayran O, Sur H. Predictors of burnout and job satisfaction
among Turkish physicians. J Assoc Physicians 2006;
99: 161-9.
8) Rosenberg T, Pace M. Burnout among mental health professionals:
special considerations for the marriage and family
therapist. J Marital Fam Ther 2006; 32: 87-99.
9) Buddeberg-Fischer B, Dietz C, Klaghofer R, Buddeberg C.
Swiss residents' arguments for and against a career in medicine.
BMC Health Serv Res 2006; 6: 1-9.
10) Moss PJ, Lambert TW, Goldacre MJ, Lee P. Reasons for considering
leaving UK medicine: questionnaire study of junior
doctors' comments. BMJ 2004; 329: 1263.
11) Çelik B, Canbaz S. Work-related strain and the prevalence of
burnout syndrome in thoracic surgeons and residents in Türkiye.
Curr Thorac Surg 2021; 6: 155-61.
12) Chappell D, Di Martino V. Violence at work. Geneva: International
Labour Organization; 2006.
13) Xaplanteri P. Correlates of mobbing among medical residents
in a university general hospital: the experience from Greece
and review of literature [Internet]. Stress-Related Disorders.
IntechOpen; 2022 [cited 2024 Jan 7]. Available from: http://
dx.doi.org/10.5772/intechopen.104041.
14) Bertizlioğlu O. Türkiye’de çocuk ve ergen ruh sağlığı ve
hastalıkları eğitiminin uzman gözünden değerlendirmesi ve mobbing
algısı. Gevher Nesibe J Med Health Sci 2022; 7: 121-30.
15) Çiçek C, Terzi C. Tıpta uzmanlık eğitimi (İzmir ölçekli iki
araştırma ve karşılaştırmalı sonuçları). Ankara: Türk Tabipleri
Birliği Yayınları; 2006. p. 1-132.
16) Çıtak N. The perspective of thoracic surgery and cardiovascular
surgery residents in Türkiye on the situation of medical
training programs and institutions. Turk Thorac Cardiovasc
Surg J 2012; 20: 299-305.
17) Kim MP, Nguyen DT, Meisenbach LM, Graviss EA, Chan EY.
Da Vinci Xi robot decreases the number of thoracotomy cases
in pulmonary resection. J Thorac Dis 2019; 11: 145-50.
18) Oparka J, Yan TD, Ryan E, Dunning J. Does video-assisted
thoracic surgery provide a safe alternative to conventional
techniques in patients with limited pulmonary function who are
otherwise suitable for lung resection? Interact Cardiovasc Thorac
Surg 2013; 17: 159-62.
19) Coyan GN, Aranda-Michel E, Kilic A, Luketich JD, Okusanya
O, Chu D et al. The impact of COVID-19 on thoracic surgery
residency programs in the US: a program director survey. J
Card Surg 2020; 35: 3443-8.
20) Daniel SJ. Education and the COVID-19 pandemic. Prospects
2020; 49: 91-6.






